A Case Report: Misdiagnosed Ectopic Cornual Rupture with Positive Fetal Heart at 13 Weeks Gestation
Author'(s): DIARI Jed*, DARIDO Jessie, BOUZID Nassima, El HADDAD Cynthia, DEROUICHE Yasmine, GREVOULFESQUET Julie, KHADAM Louay and RIGONNOT Luc
Department of Obstetrics and Gynecology, Sud Francilien Hospital. 40, Avenue Serge DASSAULT - 91106 CorbeilEssonnes, France.
*Correspondence:
DIARI Jed, Centre Hospitalier Sud Francilien. Service de Gynécologie Obstétrique. 40 Avenue Serge Dassault, 91100 Corbeil Essonnes, France.
Received: 10 April 2020; Accepted: 03 May 2020
Citation: DIARI Jed, DARIDO Jessie, BOUZID Nassima, et al. A Case Report: Misdiagnosed Ectopic Cornual Rupture with Positive Fetal Heart at 13 Weeks Gestation. Gynecol Reprod Health. 2020; 4(3): 1-5.
Abstract
Cornual pregnancy is an uncommon rare variant of ectopic pregnancies. Its diagnosis is challenging. Ruptured cornual pregnancy is still encountered nowadays with a very high consequent morbidity and mortality.
We hereby report the case of a ruptured ectopic cornual pregnancy with positive fetal heart that presented with initial hemodynamic stability and that was misdiagnosed on ultrasound to be an abdominal pregnancy in a thirtythree-year-old lady, that was previously operated of two laparotomies. In the presence of free intraabdominal fluid reaching the Morrison’s pouch diagnostic and therapeutic laparoscopy was done and intraoperatively a ruptured cornual ectopic pregnancy is diagnosed and a right cornual resection with ipsilateral salpingectomy are performed after conversion into laparotomy due to operational difficulties and intraabdominal active bleeding.
The ruptured ectopic cornual pregnancy is a situation that should be prevented via an exhaustive first trimester ultrasound examination. The ultrasound remains a helpful but not conclusive tool in the diagnosis of this condition.
Keywords
Introduction
Among ectopic pregnancies, cornual pregnancy is considered to be an uncommon hazardous variant. Its incidence is low ranging only between 2 to 3 percent of all ectopic pregnancies [1,2]. The diagnosis of cornual pregnancy remains difficult and challenging to all clinicians despite the availability of different imaging modalities especially the advances in the transvaginal ultrasound that increased the specificity and sensibility of diagnosing.
A massive life-threatening internal bleeding and consequent hypovolemia due to uterine rupture is still encountered nowadays. The rate of mortality is about two percent which consists twenty percent of all deaths due to ectopic pregnancies [3,4]. Two major conditions can be found: a misdiagnosis or a noncompliance of the woman to the classical follow up of pregnancy. Because of the myometrial stretch ability, a cornual rupture generally occurs later than 9 weeks and as late as 20 weeks [5].
In the literature, the reported cases of ruptured cornual ectopic pregnancies are limited due to the rarity of this complication. Some of them discuss the advantages and disadvantages of different treatment modalities while others reveal the sonographic pitfalls and diagnostic modalities [6].
We hereby report the case of a ruptured ectopic cornual pregnancy with positive fetal heart, initial hemodynamic stability and that was misdiagnosed to an abdominal pregnancy.
The Case
A thirty-three-year-old lady, previously healthy, Gravida 5 Para 4, presenting with acute diffused severe abdominal pain irradiating to the back associated with mild metrorrhagia and hematuria. There is no dysuria, no abnormal vaginal secretions, no nausea no vomiting or any other gastrointestinal tract symptoms. The patient has got four normal vaginal deliveries and was operated of two laparotomies for ovarian cysts (Operative report not available). No medical treatment at home. Note that the patient has not been aware of her pregnancy state up until her current presentation.
Upon presentation, she was hemodynamically stable (pulse 71, blood pressure 126/71). Her abdomen was soft and the pain was present on deep palpation only. No palpable mass on vaginal examination but Cervical Motion Tenderness is present. On speculum exam, there is mild vaginal bleed coming out from the cervix.
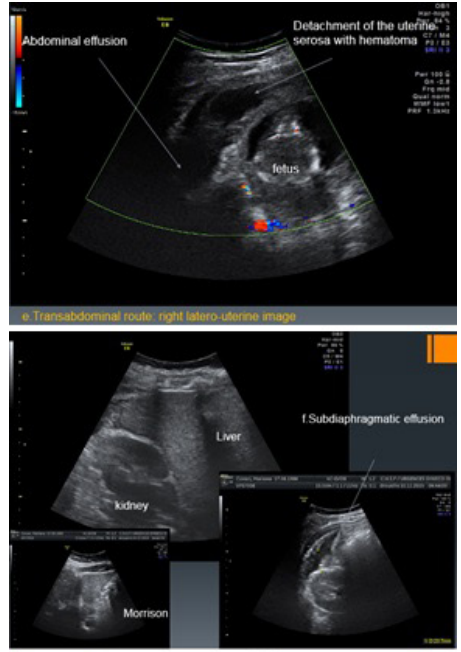
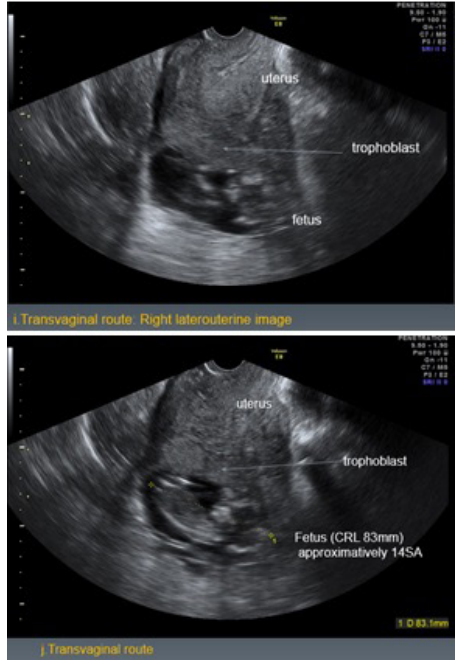
Ultrasound is done showing the suspicion of an extrauterine abdominal pregnancy of 13 weeks and 4 days that consists of a mass containing the fetus and trophoblastic tissue. It also reveals free fluid in the paracolic gutters and Morrison’s pouch.



Her labs are as follow: Prothrombin Time 100%, creatinine 47, C Reactive Protein 4.6, Hemoglobin 12.3 then 9.3 on preoperative control, White Blood Count 16.24, platelets 307 and the ionogram is normal.
Diagnostic and therapeutic laparoscopy is decided and the patient is transferred to the operating room. Intraoperatively, a ruptured cornual ectopic pregnancy is diagnosed and a right cornual resection with ipsilateral salpingectomy are performed.
Under general anesthesia, the patient is in dorsal lithotomy position. Scrubbing and draping is performed and the Foley catheter is in place. Laparoscopy is started via Subumbilical incision where the open technique is used. Two trocars are inserted on the right and left lower quadrants.
Upon inspection, severe parietal epiploic adhesions are noted with a large intra-abdominal hemoperitoneum. Both ovaries are of normal volume and aspect and at the level of the uterus there is a right cornual rupture. Then, in the presence of hemodynamic instability and active bleeding that is taking place, a conversion of the operation into laparotomy is done.
Pfannenstiel incision is performed on the previous skin scar followed by a layer by layer dissection till reaching the intra- abdominal cavity. Aspiration of the hemoperitoneum estimated the blood loss about two liters. Then we proceeded into right salpingectomy and right cornual resection taking the pregnancy implantation site. Two layers interrupted closure of the uterine cavity with vicryl 1 then continuous closure of the uterine serosa with monosyn 2.0. Hemostasis is observed and reassured then copious irrigation of the abdominal cavity. A hemovac drain is inserted into the douglas pouch. Parietal peritoneum is closed with continuous Vicryl 2.0.
The Fascias at the level of the subumbilical and pfannenstiel incisions are closed using interrupted and continuous vicryl 1 sutures respectively. Skin is closed using staplers and interrupted monosyn 3.0. The pad count is verified and correct. Urine is clear at the end of the intervention. Note that the patient received two PRBC postoperatively. The patient’s clinical and hemodynamical state is stable postoperatively.



At day 1 postoperatively, the patient is clinically stable with mild pain, negative flatus, mild tachycardia (100 bpm), soft abdomen, positive peristaltism and clean dressing. Drain is giving 270 ccs of serosanguinous fluid over 24 hours. Hemoglobin is 8.7. We have discussed with the couple upcoming recommended contraception and they both approved for subcutaneous hormonal implant. At the end of day 1, the patient is hemodynamically stable, no tachycardia, no vertigo and the drain is giving 10 ccs over 6 hours. Discharged home at day 2 in good general state with positive flatus and after the insertion of the subcutaneous levonorgestrel implant.
Discussion
The cornual ectopic pregnancy is considered as a part of the non- tubal ectopic pregnancies that are commonly misdiagnosed [7]. It is very important to distinguish between interstitial pregnancy and cornual pregnancy. They are not interchangeable. They are different in terms of localization, clinical presentation and the gestational age at which they got diagnosed. The cornual pregnancy is a uterine but localized ectopically at the upper and lateral uterine cavity whereas the interstitial one is implanted in the proximal intramural portion of the tube [8,9].
Furthermore, as reported in the case series of Tulandi T et al that in contrast with the interstitial pregnancy which ruptures before 12 weeks, the cornual pregnancy rupture occurs after 12 weeks [2], an evidence that was clearly supported by our case.
Many predisposing factors can be listed in cornual pregnancy: the assisted reproductive techniques, a history of pelvic inflammatory disease and sexually transmitted diseases, rudimentary horn, previous ipsilateral salpingectomy, previous ectopic pregnancy. However, we can encounter cases with no risk factors [10]. In our case, the patient was operated of two laparotomies. Therefore, we can predict that the main risk factor in our case is the possible proximal intratubal adhesions [2,11,12]. In addition, the absence of a correct follow up and first trimester localization is a major cause of this kind of complications.
In 1983, the first sonographic diagnosis of unruptured cornual pregnancy was reported [13]. However, till now, the sensitivity of ultrasound in the ectopic pregnancy diagnosis remains not more than twenty six percent [14]. In 2007, Mavrelos et al made a prospective study over eight cases of cornual pregnancy out of 978 ectopic, which is equivalent to 0.8 percent. In these observed cases, the pregnancy occurred in the rudimentary horn of a unicornuate uterus and the diagnosis was made based on specific ultrasound criteria. The majority was nulliparous, with thirty-one years old mean of age and sixteen weeks mean of gestational age. Six out of eight had a positive fetal heart [15]. So, excluding her state of a multiparous, our patient is similar to the latter studied cases. Note that in our case the ectopic pregnancy in itself was not misdiagnosed. However, the localization of it was not clearly revealed especially in the presence of positive fetal heart and initial hemodynamic stability. In addition, the possible abdominal ectopic pregnancy couldn’t be ruled out especially that the product of conception was not mobile on palpation.
The treatment of cornual ectopic pregnancies consists of either a medical treatment with systemic methotrexate injected systematically or locally or a surgical treatment. The latter one includes:
- Laparotomy with cornual resection or hysterectomy,
- Laparoscopy with cornual resection and salpingectomy,
- Hysteroscopy with endometrial resection or cornual evacuation under ultrasound or laparoscopic guidance [16,17]. In 2009, MacRae R et al reported eleven consecutive cases of cornual ectopic pregnancy that all presented with abdominal pain and vaginal bleeding: two of them (18%) became unstable before laparoscopy. Their mean of gestational age was 8 ± 2 weeks and the diagnosis were done via a transvaginal ultrasound. Only ten percent of the cases were missed. On the other hand, one patient had the conversion into laparotomy while in other cases the cornual resection was performed laparoscopically. Methotrexate was needed post laparoscopy only in ten percent of the cases. So, most of the reported cases of cornual pregnancies were treated laparoscopically even the ones with hemoperitoneum with a nine percent conversion into laparotomy. In fact, laparoscopy is considered safe and less invasive with an acceptable percentage of consequent It decreases the hospital stay and health care costs [18,19].
In our case, the team was well experienced in the laparoscopic technique and has the capacity to turn immediately into laparotomy if the state of the patient required. Therefore, we have started a minimally invasive laparoscopic surgery. However, in the presence of the active bleeding and huge hemoperitoneum, the laparoscopic approach was difficult and the decision of conversion into laparotomy was done. A cornual resection with ipsilateral salpingectomy was performed. The technique of suturing that was done and that consists of suturing the uterine wall will reinforce the defective area of the uterus and can prevent subsequent ruptures in case other pregnancies occurred.
Despite the decreased fertility rate that will be consequent to this surgical approach and considering the socio economic status of the patient and the risk of recurrence not only of the rupture but also of the ectopic pregnancy that can occur as early as 4 months and as late as 5 years after the first ectopic pregnancy [20], contraception based on subcutaneous hormonal implant was strongly recommended to this patient at day 2 postoperatively and to be renewed after three years.
Conclusion
Finally, the ruptured ectopic cornual pregnancy is a situation that should be prevented via an exhaustive first trimester ultrasound examination and localization of the gestational sac and the introduction of the four-dimensional ultrasound imaging that provides more accurate images than the two dimensions transvaginal ultrasound. Despite its limitation’s ultrasound in association with the clinical features remains the basically, helpful but not conclusive tool in the diagnosis of cornual pregnancy. The ultimate goal is fertility preservation and conservative treatment. It is very important to establish accurate ultrasound criteria in order to not only improve the diagnosis but also prevent misdiagnosis of cornual ectopic pregnancy. Furthermore, we as obstetricians should increase our awareness regarding all non-tubal pregnancy despite their rarity and this will be our challenge towards an optimized management and the pillar towards patient safety.
References
- Malinowski A, Bates SK. Semantics and pitfalls in the diagnosisof cornual/interstitial Fertil Steril. 2006; 86: 1764.
- Tulandi T, Al jaroudi D. Interstitial pregnancy: results generated from the society of reproductive surgeon’s Obstet gynecol. 2004; 103: 47-50
- MolinaroT, Barnhart K. Ectopic pregnancies in unusual locations. Semin Reprod Med. 2007; 25: 123-130.
- Tang A, Baartz D, Khoo SK. A medical management of interstitial ectopic pregnancy: a five-year clinical study. Aust N Z J obstet Gynaecol. 2006; 46: 107-111.
- M Sami Walid, Richard L Diagnosis and laparoscopic treatment of cornual ectopic pregnancy. Ger Med Sci. 2010; 8.
- Ackerman TE, Levi CS, Dashefsky SM, et Interstitial line: sonographic finding in interstitial cornual ectopic pregnancy. Radiology. 1993; 189: 83-87.
- Parker VL, Srinivas Non tubal ectopic pregnancy. Archives of gynecology and obstetrics. 2016; 294: 19-27.
- Sargin MA, Tug N, Ayas S, et al. Is interstitial pregnancy clinically different from cornual pregnancy? A case report. J clin Diagn Res. 2015; 9: QD05-QD06.
- Botros rizk, Candice P holliday, Mostafa Challenges in the diagnosis and management of interstitial and cornual ectopic pregnancies. Middle East fertility society journal. 2013; 18: 235-240.
- Oldamaa T, Stucka S, Ivory C, et al. survival of cornual (iinterstitial) pregnancy. European journal of obstetrics and gynecology and reproductive biology. 1999; 84: 103-105.
- Chopra S, keepanaseril A, Rohilla M, et Obstetric morbidity and the diagnostic dilemma in pregnancy in rudimentary horn. Retrospective analysis. Arch Gynecol obstet. 2009; 2809: 907-910.
- Pluchino N, Ninni F, Angioni S, et al. Sponatenous cornual pregnancyafter homolateral salpingectomy for an earlier tubal pregnancy: a case report and literature review. J minim Invasive Gynecol. 2009; 16: 208-211.
- Holden R, Hart First trimester rudimentary horn pregnancy: prerupture ultrasound diagnosis. obstet gynecol. 1983; 61: 56S-58S.
- Jayasinghe Y, Rane A, stalewski H, et al. The presentation and early diagnosis of the rudimentary uterine horn. Obstet gynecol. 2005; 105:1456-1467.
- Mavrelos D, Sawyer E, Helmy S, et al. Ultrasound diagnosis of ectopic pregnancy in the non-communicating horn of a unicornuate uterus (cornual pregnancy). Ultrasound in obstetrics gynecology. 2007; 30: 765-770.
- Faraj R, Steel Review management of cornual (interstitial pregnancy. The obstetrician and gynecologisy. 2007; 9: 249- 255.
- Choi Y, Eun D, Choi J, et Laparoscopic cornuotomy using a temporary tourniquet suture and diluted vasopressin injection in interstitial pregnancy. Fertil Steril. 2009; 91: 1933-1937.
- Soriano D, Vicus D, Maschiash R, et al. Laparoscopic treatment of cornual pregnancy: a serie of 20 conservative cases. Fertil Steril. 2008; 90: 839-843.
- MacRae R, Olowu O, Rizzuto MI, et al. Diagnosis and laparoscopic management of 11 consecutive cases of cornual ectopic pregnancy. Arch Gynecol Obstet. 2009; 280: 59-64.
- Tinelli A, Malvasi A, Pellegrino M, et al. Laparoscopical management of cornual pregnancies a report of three cases. Eur J Obstet Gynecol Reprod Biol. 2010; 151: 199-202.
- Abdelazim I, Shikanova S, Bekzhaniva M. Laparoscopic management 4 cases of recurrent cornual ectopic pregnancy and review of literature. Journal of Minimally Invasive Gynecology. 2019; 26: 774.