A New Model for Integrative Diagnosis and Management of PTSD in a Large Population
Author'(s):Julian Ungar-Sargon*
Franciscan Hospital System, IN 47978, Indiana, US.
*Correspondence:
Julian Ungar-Sargon, Franciscan Hospital System, IN 47978,Indiana, US.
Received: 24 Apr 2024; Accepted: 02 Jun 2024; Published: 10 Jun 2024
Citation: Ungar-Sargon J. A New Model for Integrative Diagnosis and Management of PTSD in a Large Population. Addict Res. 2024;8(1): 1-13.
Keywords
Preamble
After decades working in the field of chronic degenerative neurological disorders, I turned my attention to interventional pain management strategies in an effort to become more effective as a healer.
I discovered that the same issues were behind the symptoms of acute pain disorders as were chronic and that the human dimension of pain and suffering and the human experience of disease was as much a factor in the diagnostic and healing process of both acute and chronic disease.
Nowhere more did I discover these factors than in the disorder known as PTSD. Here, in seeing my brothers in arms in the military as well as in civilian practice, the influence of past trauma, and the coping mechanisms learned or inherited, played as important a role in predicting outcome as any intervention, physical or psychological.
Over the decade my approach to hard core neurological disease has evolved yet centered around listening to the patient, what the focus of his or her concern is, what bothers him more than others, for the same disease model, and how does his or her experience of the disease affect the way they view themselves, the future and their decline. Disease names such as Parkinson’s or Alzheimer’s strike fear and dread into the hearts of patients and their caregivers yet calling it by a different name often does not carry the same social cultural stigma [1].
In Listening to the Patient and Understanding their Cultural, Socioeconomic Resources and Spiritual Heritage I Am Able to Conjure an Inner Landscape Where I Might Empathize Better with What the Patient is Experiencing.
By appreciating the inner dimension of the human suffering and anguish I am a better healer since I am able to tailor the therapeutics taking into account the fear and anxieties that might otherwise be overlooked when administering this or that therapeutic regime. If the patient is deadly afraid of side effects, I might be more sensitive to a lower dose of the drug regime because of my concern about compliance.
In listening to each patient closely like a sacred text, I must “interpret” and engage in hermeneutics the way I do when reading the subtext and nuances of grammar prosody syntax and literary constructs. My research into Midrash helped me a lot, to understand the very history presented to me, paying closer attention to the stylistics of speech of the patient and such as the verbal content. All this must be interpreted and mined for inconsistencies gaps, repetitions etc the way I would read a verse of scripture.
This emphasis on listening and communication has its roots in medicine itself. Medicine has many tools, instruments, technologies, measures, test and methods. But the most basic of all its measures is language. For anything to happen between caregiver and patient, anything at all, there must be communication, each speaking to the other. And more than that, because doctor and patient often start from such different places of speaking, healing is an act, or multiple acts, of translation.
This healing language of which I speak can be at times in tension with the medical language that doctors and many other health- care professionals become fluent in in the course of their training. The language of medicine, paradoxically, keeps the patient at a distance. Most patients never learn to speak the Latinate argot of medicine, and typically find it very removed from their own experience, sometimes traumatically so.
We learn to speak of the patient’s body as an object to be known and dissected and disciplined and fought, not as of them, belonging to them. But as comforting as it can be to feel that our illnesses have comprehensible, treatable, even mechanical causes, to have our individual suffering knowable and classifiable in this totalizing way can evoke for the sufferer, as the medical sociologist Arthur Frank argues in “The Wounded Storyteller: Body, Illness, Ethics,” a duality of sensibility, a conflictual experience of the body as, simultaneously, an object to be known, and the subjectively felt collection of sensations which we alone experience as ourselves [2].
Today as never before, both the experience of illness and the experience of treating affliction take place within relationship and often within a complex series of relationships. In their reliance on witch doctors, oracles, shamen, priests, as well as in the family- wide and community-wide experience of illness, our forebears well understood this, and the severance of the simultaneous connections of spiritual and social bonds to the body in pain and illness is a recent development, another artifact of the modern situation of the body within the biomedical model.
Intuitive Practice of Medicine
A study investigated real cases of physician intuition. Eighteen family medicine doctors were interviewed about their intuitive decision-making processes with patients [3]. Their responses were sorted into three different types of intuitions: “gut feelings,” which triggered a sense of alarm that spurred them to take action; “recognitions,” decisions made in the face of conflicting information or a lack of evidence; and “insights,” occurring as a rapid flash of inspiration that connected the dots to a correct diagnosis when no symptom interpretation was obvious.
I am sure all three of these types play a role in my analyzing of patient’s complaints but there is another intangible dimension of the interaction. It is a spiritual connection whereby my ego has to get out of the way as I am listening intently. I become lost in their narrative, exploring their inner landscape engaged fully without even awareness of myself.
This kind of self- nullification is the mirror image of what I was trained to do, an objective analysis of the symptoms and signs looking for patterns that compare this case with the body of medical literature for common threads allowing for a diagnosis.
My project is to integrate this approach yet all the while making use of state of art techniques to bridge the gap between the inner experiential and outer objective evidence based scientific analysis.
I am submitting this as a preliminary proposal for an institute for the study and treatment of PTSD in a large population such as Israel that has been subjected to over 7 months of continuous media coverage and nonstop displays of families of hostages, murder scenes from the Hamas brutality, and recounts of torture rape and murder by survivors and their families. This institute would be devoted to the diagnosis treatment and research into better methods for managing the ongoing trauma through an eclectic approach both scientific and intuitive.
The use of state of art imaging electrophysiological and AI tools will allow the parameters of therapy to measured scientifically in an evidence based environment. I believe that my approach to the dignity of the individual patient combined with the exacting scientific data-driven method of measuring outcomes is a unique model.

The Problem Background
On October 7th, 2023, a mass terror attack was launched by Hamas militants, which was followed by the Israel-Hamas war. These events constitute a nationwide trauma with major ramifications for public mental health.
In a recent study Yossi Levi-Belz Yoav Groweiss Carmel Blank and Yuval Neria found an alarmingly high incidence of PTSD, depression, and anxiety after the October 7, 2023 attack in Israel: in a nationwide prospective study
The magnitude of the Oct 7, 2023 attack in southern Israel was without precedent. More than 1300 civilians were murdered, and 240 civilians were kidnapped and taken hostage. In this national cohort study, for which baseline outcome data were established before the attacks, a prospective assessment of posttraumatic stress disorder (PTSD), depression, and generalized anxiety disorder (GAD) was conducted one month after the attack [4].
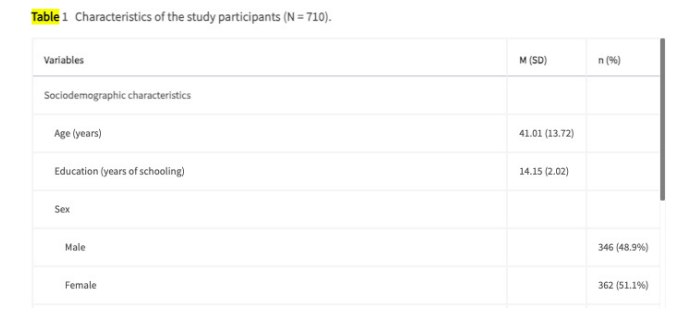
Participants’ Demographics and Trauma Exposure
The sample's demographic and October 7 attack-related variables are presented in Table 1. The study sample (n = 362, 51% women) had a mean age of 41 years (SD = 13.7) and a mean level of education that exceeded secondary, as measured by years of schooling (mean = 14.15, SD = 2.01). The sample comprised 80% Jewish Israeli citizens and 20% Arab Israeli citizens, reflecting the national proportionality. Comparing participants who participated only at T1 with those at both T1 and T2, we found no significant differences in most sociodemographic variables (see Supplement S2). Moreover, the sample at T2 comprise a close representation of the Israeli population (e.g., the proportion of Jews and Arabs, sex, and age). The vast majority of the sample (n = 669, 95.7%) were not present in the Gaza envelope communities during the October 7 attack, but almost one in five participants (n = 131, 18.6%) had a close friend or family member who was harmed during the attack.
Less than one-third (n = 212, 30%) of the sample reported they sought shelter due to rocket attacks once or not at all, and almost 35% (n = 245) reported seeking shelter many times.
Discussion
This study is the first to examine, longitudinally, the mental health consequences of the Oct 7, 2023, terrorist attack among Israeli civilians. Following the attack, the prevalence of probable PTSD, depression, and anxiety were found to be high (29% for PTSD, 42%-44% for depression and GAD, respectively), almost doubling the prevalence’s recorded two months before the attack. As noted, the brutality and the sheer number of casualties in the October 7 attack were unprecedented in Israel's history and likely beyond. Moreover, these events seem to have affected the participants' lives, including grieving those murdered, concern over those kidnapped, and the threat to personal safety (both personally and collectively). Thus, it may not surprise that the prevalence of PTSD, depression, and GAD are considerably higher than those reported in previous studies focusing on terrorist attacks, such as the 9/11 attacks and other terrorist attacks.
Following that, the current findings may reflect the psychological burden of the attack on the Israeli population, underscoring the impact of the attack on both Jews and Arabs within the community.
Aligning with other studies [5],
We found that direct exposure to the attack had a high impact on both probable PTSD and depression, as those present in the Gaza envelope communities during the attack had a 3-times higher likelihood of presenting with probable PTSD and a 2-times higher likelihood of presenting with depression. These findings are alarming, emphasizing the importance of implementing prevention efforts aimed at reducing chronicity [24]. Exacerbating the upended life of many citizens, those with direct exposure were compelled to evacuate their homes due to the war with Hamas that commenced following the attack.
Prediction Model
A Prediction Model of PTSD in the Israeli Population in the Aftermath of October 7th, 2023, Terrorist Attack and the Israel- Hamas War in a collaborative study [5].
The article presents an evidence-based model for the prediction of the prevalence of posttraumatic stress disorder (PTSD) related to the terrorist attack and the war. Main body: The creation of the model consisted of several steps. Firstly, the Israeli population was divided into six groups based on the intensity, context, and type of traumatic exposure (direct exposure to terror, close proximity to terror, soldiers in combat and support units, intense exposure to rocket attacks, moderate exposure to rocket attacks, and indirectly affected communities), and the population size of each group was assessed using official national databases.
Secondly, an estimation of the expected prevalence of PTSD in each of the exposure groups was based on a review of the relevant literature. A random-effects meta-analysis of the prevalence rates was conducted separately per each exposure group. Finally, the predicted number of PTSD causalities in the population was calculated by multiplying the group size and the PTSD prevalence estimation.
Based on population size and estimated PTSD prevalence within each exposure category, the model predicts that approximately 5.3% (N=519,923) of the Israeli population (95% prediction interval, 160,346- 879,502), may develop PTSD as a result of the terrorist attack and the war.
Review study [6]
The study, found the prevalence of probable PTSD, depression, and anxiety in the weeks following the attacks (29% for PTSD, 42%-44% for depression and GAD, respectively), almost doubling the prevalence recorded two months before the attack.
"The prevalence’s of PTSD, depression, and anxiety are considerably higher than those reported in previous studies focusing on terrorist events, such as the 9/11 attacks and other attacks," said Yossi Levi-Belz, Ph.D., a professor of clinical psychology and chair the Lior Tsfaty Center for Suicide and Mental Pain Studies at the Ruppin Academic Center in Israel who led the study.
The nationwide cohort study, according to the researchers, addressed limitations of previous research by using prospective study design to evaluate the impact of the attack. The researchers employed a wide range of probable outcome measures including PTSD, depression, and generalized anxiety disorder (GAD), assessing a cohort of Israeli citizens, both Jews and Arabs, twice, 6-7 weeks before the attack and 5-6 weeks after the attacks.
Since the beginning of the conflict 240,000 Israeli civilians have evacuated their homes and 129 Israelis are still held hostage. The ground war in Gaza has also taken a heavy toll on Palestinians. The health ministry in the Hamas-ruled Gaza Strip said that more than 20,000 people have been killed in the Palestinian territory since the beginning of the war.
Prior Conflicts [7]
Many studies attempt to gauge population prevalence of post- traumatic stress disorder (PTSD) following a major catastrophe. However, little is known about the validity of these estimates in the increasingly common situation of ongoing trauma. During the period of the Second Intifada in Israel, which involved frequent and widespread terrorist attacks, several studies generated estimates of PTSD prevalence in the Israeli population, but yielded widely discrepant findings. A number of focused surveys using symptom checklists estimated population prevalence of PTSD or probable PTSD diagnosis at about 9%. However a large population health study conducted during this same time period using a structured diagnostic interview yielded a very low estimated prevalence of PTSD (0.5%). We examined methodological differences that might account for these striking discrepancies. Inherent limitations of both checklist and structured interview methods may be especially problematic in the context of ongoing trauma. Findings regarding PTSD and associated factors obtained during ongoing trauma should be interpreted with caution.
Prolonged Grief Disorder
In 2019, Clare Killikelly et al. examined Prolonged grief disorder and Its co-occurrence with adjustment disorder and post-traumatic stress disorder in a bereaved Israeli general-population sample [8].
Prolonged grief disorder (PGD) is a new disorder included in the WHO International Classification of Diseases 11th version (ICD- 11). This study is the first to use these new ICD-11 PGD guidelines to examine prevalence rates, predictors of PGD and disorder co- occurrence with other stress-related disorders in a survey of 544 bereaved Israelis.
Methods
Descriptive statistics, correlation, linear regression and mediation analysis examined the validity of the ICD-11 diagnostic algorithm.
Results
Prevalence of PGD in the Israeli population sample is low (2%). The prevalence rate of post-traumatic stress disorder (PTSD) was 7.2% and for adjustment disorder (AjD) was 17.8%. A significant positive correlation found between scores on these measures indicates concurrent validity. Mediation analysis found that symptoms of PGD were predicted by serious life events, and significantly mediated by symptoms of PTSD and AjD. A regression analysis found significant predictors of PGD symptom severity, including socio-demographic and person-specific predictors.
Limitations
This study did not assess the index-death of the grief questionnaire. No conclusions could be made regarding the relationship between the type of loss and grief severity. Furthermore, the time since loss (time criterion) was not assessed.
Conclusions
This study is the first to examine prevalence rates of ICD-11 PGD in a population-based survey. The mediation relationship between serious life events, AjD, PTSD and PGD supports a vulnerability model of stress related disorders whereby the number of stressful life events may predict symptoms of stress related disorders.
Clinical Presentation
What Are the Symptoms of PTSD? [9]
PTSD symptoms usually start soon after the traumatic event, but they may not appear until months or years later. They also may come and go over many years. If the symptoms last longer than 4 weeks, cause you great distress, or interfere with your work or home life, you might have PTSD.
There are 4 types of PTSD symptoms. To be diagnosed with PTSD, you need to have each type. That said, everyone experiences symptoms in their own way.
1. Reliving the event (also called re-experiencing symptoms).
Memories of the traumatic event can come back at any time. They can feel very real and scary. For example:
- You may have nightmares.
- You may feel like you are going through the event again. This is called a flashback.
- You may see, hear or smell something that causes you to relive the event. This is called a trauma reminder, cue or trigger. News reports, seeing an accident, or hearing fireworks are examples of trauma reminders.
2. Avoiding things that remind you of the event. You may try to avoid situations or people remind you of the trauma event. You may even avoid talking or thinking about the event. For example:
- You may avoid crowds because they feel dangerous.
- You may avoid driving if you were in a car accident or if your military convoy was bombed.
- If you were in an earthquake, you may avoid watching movies about earthquakes
- You may keep very busy or avoid getting help so you don't have to think or talk about the event.
3. Having more negative thoughts and feelings than before the event. The way you think about yourself and others may become more negative because of the trauma. For example:
- You may feel numb-unable to have positive or loving feelings toward other people-and lose interest in things you used to enjoy.
- You may forget about parts of the traumatic event or not be able to talk about them.
- You may think the world is completely dangerous, and no one can be trusted.
- You may feel guilt or shame about the event, wishing you had done more to keep it from happening.
4. Feeling on edge or keyed up (also called hyperarousal). You may be jittery, or always alert and on the lookout for danger. You might suddenly become angry or irritable. For example:
- You may have a hard time sleeping.
- You may find it hard to concentrate.
- You may be startled by a loud noise or surprise.
- You might act in unhealthy ways, like smoking, abusing drugs or alcohol, or driving aggressively.
Diagnosis [10] How is a PTSD diagnosis made?
A PTSD diagnosis requires exposure to at least one trauma. Traumas include being exposed to threatened death, actual or threatened serious injury, or actual or threatened sexual violence. Examples are direct exposure, witnessing a trauma, or learning that a relative or close friend was exposed.
At least one “intrusion” symptom is required for a PTSD diagnosis. These symptoms include unwanted and upsetting memories, nightmares, flashbacks, and emotional distress or physical reactions following reminders. At least one “avoidance” symptom is also required for a PTSD diagnosis. These symptoms include avoidance of trauma-related thoughts or feelings, and/or avoidance of trauma-related reminders. At least two “negative alterations in cognitions and mood” are required. These include negative thoughts or feelings that began or worsened after the trauma, an inability to recall key features of the trauma, overly negative thoughts and assumptions about oneself or the world, exaggerated blame of self or others for causing the trauma, negative mood, decreased interest in activities, feeling isolated, and difficulty experiencing positive mood. Finally, there needs to be at least two “hyperarousal” symptoms, such as irritability or aggression, risky or destructive behaviour, hypervigilance, heightened startle reaction, difficulty concentrating, and difficulty sleeping.
Symptoms must last for more than one month and cause significant distress or problems to the individual’s daily functioning. Symptoms must not be due to medication, substance use, or other illness. The latest World Health Organization’s International Classification of Diseases (ICD-11) also includes complex PTSD, which involves the core symptoms of PTSD plus disturbances in self organization, mood dysregulation, negative self-concept, and disturbances in relationships.
A variety of tools have been developed to screen for or diagnose PTSD. The gold standards for diagnosis are the Clinician- Administered PTSD Scale (CAPS) and the Structured Clinical Interview for DSM-V (SCID-5), PTSD module. There are also a wide range of self-report PTSD measures, including the Primary Care PTSD Screen (PC-PTSD) and the PTSD Checklist (PCL), which are mostly used to monitor PTSD symptom severity, but can also be used for screening and diagnosing PTSD in people who have been exposed to trauma.
What is the evidence regarding diagnosis and detection of PTSD?
Moderate to high quality evidence finds a small increase in the severity of PTSD symptoms in people exposed to DSM-5 nominated traumas of actual or threatened death or serious injury or of threat to the physical integrity of self or others compared to people exposed to other traumas such as divorce, financial stress, or minor car accidents. Around 24.5% of people diagnosed with PTSD have a delayed onset (>6 months post trauma), with most of these people experiencing earlier and milder subclinical symptoms. Delayed-onset PTSD is highest in professional groups and in those who experienced combat trauma (prevalence in both is around 40%).
There is reasonable sensitivity and good specificity of the PC- PTSD and the PCL for predicting a diagnosis of PTSD. There is good diagnostic validity and internal consistency, and reasonable test-retest and external (convergent) validity of the PCL. For children, the average T score on the Trauma Symptom Checklist for Children is around 50 in those exposed to traumatic events, which is 15 points less than the clinical cut-off for PTSD on this scale. Factors associated with increased scores on the Trauma Symptom Checklist for Children include international (vs. U.S.) samples, sexual abuse (vs. neglect, community violence, or complex trauma), female sex, and older age in sexual abuse samples. Moderate to low quality evidence finds machine learning techniques (mostly support vector machine learning) using neuroimaging, neuropsychological, or audio data can reasonably predict PTSD in people previously diagnosed with PTSD using traditional means (mostly the CAPS or PCL). Outcome assessment tools [11].
What are assessment tools for PTSD?
Standardized assessment tools for PTSD are vital for assessing a range of variables including symptoms, functioning, and quality of life. They are often used within a controlled research environment, but high-quality assessment tools are also useful in practice for both clinical management and outcome prediction.
What is the evidence for outcome assessment tools for PTSD?
Moderate quality evidence finds a model comprising 4-factors of intrusions, avoidance, hyperarousal, and dysphoria/numbing yielded the best fit for clustering PTSD symptoms. Assessment measures for this model included the Clinician-Administered PTSD Scale, Harvard Trauma Questionnaire, Modified PTSD Symptom Scale, PTSD Checklist, PTSD Diagnostic Scale, PTSD Symptom Scale, SCID = Structured Clinical Interview for DSM-IV Diagnosis, Screen for Post-traumatic Stress Symptoms. Intrusions symptoms included intrusive thoughts of trauma, recurrent dreams of trauma, flashbacks, emotional reactivity to trauma cues, and physiological reactivity to trauma cues. Avoidance symptoms included avoiding thoughts of trauma and avoiding reminders of trauma. Hyperarousal symptoms included hypervigilance, exaggerated startle response, sleep disturbance, irritability, and difficulty concentrating. Dysphoria/numbing symptoms included inability to recall aspects of the trauma, loss of interest, detachment, restricted affect, and sense of foreshortened future. Sleep disturbance, irritability, and difficulty concentrating may also be classed as dysphoria symptoms.
Moderate to high quality evidence finds similar scores on clinician- administered and self-report PTSD rating scales in clinical trials. Subgroup analysis found a trend for more conservative scores on clinician-administered scales in trials of children and adolescents, but not in trials of adults.
There were weak to moderate correlations between increased Centrality of Event Scale scores (having a negative event central to one’s identity and life story) and increased PTSD symptoms (avoidance, arousal, re-experiencing), post-traumatic growth, grief, trauma cognitions, memory vividness, emotional intensity, shame, physical reaction, depression, anxiety, negative trauma emotions, dissociation, neuroticism, life danger and injury traumas, female sex, and openness. There were no or very weak correlations between increased Centrality of Event Scale scores and decreased satisfaction with life, social support, extraversion, conscientiousness, and agreeableness. There were small to medium-sized associations between increased PTSD symptom scores and decreased mindfulness scores on the Five Facet Mindfulness Questionnaire.
Moderate to low quality evidence is unable to recommend the use of any particular scale for assessing outcomes in youth exposed to traumatic events. Scales assessed were; the Child Behaviour Checklist-PTSD, University of Los Angeles-Post-Traumatic Stress Disorder Scale - reaction index, Child PTSD Symptom Scale, Child Dissociative Checklist, Adolescent Dissociative Experiences Scale, Solution Focused Recovery Scale, Child and Youth Resilience Measure-28, Child and Youth Resilience Measure-12, Minnesota Multiphasic Personality Inventory-Adolescent, Beck Self-Concept Inventory for Youth, Adult Attachment Interview, Global Assessment of Functioning Scale, Children’s Global Assessment of Functioning Scale, Adolescent Clinical Sexual Behaviour Inventory, Child Sexual Behaviour Inventory, Vineland Adaptive Behaviour Scale-II, Trauma Symptom Checklist for Young Children, Trauma Symptom Checklist for Young Children- Short Form, Assessment Checklist for Children, Brief Assessment Checklist for Children, Trauma Assessment for Young Children, Child Pediatric Emotional Distress Scale, Trauma Play Scale, Story Stem Assessment Profile, Dominic Interactive Assessment, Assessment Checklist for Adolescents, and the Brief Assessment Checklist for Adolescents.
General signs and symptoms
• Anger and aggression
• Anxiety
• Avoidance
• Depression
• Dissociation
• Distress
• Hyperarousal
• Intrusions
• Negative thoughts and mood
• Perceptions of defeat and entrapment
• Personality and temperament
Cognition [12]
Some people with PTSD show cognitive alterations, which may interfere with an individual’s ability to function. Cognitive alterations have been found in attention, memory, planning, and social cognition. Some symptoms of PTSD may contribute to poor cognition.
Symptoms of intrusions and hyperarousal can result in poor sleep, which in turn affects cognition. Symptoms of avoidance can result in poor attention. PTSD is also characterized by alterations in the hypothalamic-pituitary-adrenal axis, in neuro-metabolites, and in inflammatory response, which could all affect cognitive ability.
General signs and symptoms [13]
This category provides information about the general signs and symptoms of PTSD. Common PTSD symptoms include unwanted and upsetting memories, nightmares, flashbacks, emotional distress and physical reactivity after exposure to reminders, which leads to avoidance of these reminders.
There may also be symptoms of poor sleep, negative thoughts and mood, depression, anxiety, dissociation, and anger. There may also be problems with cognition, such as memory, attention, executive functioning, general cognition, social cognition, and difficulty processing new information
Cognition
• Attention
• Cognitive failures
• Episodic future thinking
• Executive functioning
• General cognition
• Information processing
• Language
• Learning
• Memory
• Social cognition
• Visuospatial ability
The Field of Psychiatry and PTSD
Defining Trauma and PTSD
As the majority of the studies discussed within this review define PTSD on the basis of Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria, we will first outline these criteria and then elaborate upon recent DSM-5 revisions. PTSD is the primary disorder characterized by exposure to a traumatic event, wherein one encounters or witnesses actual or threatened death or severe injury and reacts with intense fear, helplessness,and/or horror. Traumatic events include child abuse (physical, sexual, emotional), child neglect, domestic violence, physical/ sexual assault, accidents, life-threatening illness, death of a family member, natural disasters, war, combat, and community or school violence.
Other DSM-IV PTSD criteria include at least one symptom of recurrent and intrusive thoughts (e.g., flashbacks), three or more symptoms of persistent avoidance and numbing of stimuli related to the trauma (e.g., avoiding thoughts and activities), and two or more symptoms of increased arousal (e.g., hypervigilance and difficulty falling/staying asleep) for at least 1 month.
Symptoms of re-experiencing include recurrent nightmares, physical responses to trauma cues, and/or sensations that the trauma is continuing. For example, Iraqi veterans may have frequent nightmares of their experiences in Iraq, sweating every time they remember particular situations such as bombings; additionally, veterans may avoid visiting places similar to Iraq to avoid aversive feelings, memories, and physiological sensations linked to these violent attacks.
A PTSD diagnosis requires that symptoms cause significant disturbance and impairment to social, vocational, and other imperative life functioning (7). PTSD criteria in DSM-5 (9) were updated by transforming these three clusters (re-experiencing, avoidance/numbing, and arousal) into four symptom clusters present for 1 month or longer:
1) Intrusions;
2) Avoidance of trauma-related thoughts or activities;
3) Negative alterations in cognition and mood (e.g., negative affect, anhedonia, self- and other-blame, inability to recall details of the trauma, and isolation); and
4) Changes in arousal (e.g., hypervigilance, exaggerated startle response, irritability, aggression, sleep problems, and concentration difficulties).
One important issue to consider with respect to categorical classification of disorder is that there are many paths to a PTSD diagnosis, and symptom heterogeneity is the rule, not the exception. As a result, in addition to evaluating brain activity as a function of presence versus absence of a PTSD diagnosis, relating brain processes to dimensional symptom presentations in line with the Research Domain Criteria may facilitate more rapid development of precision medicine for treatment of trauma-related dysfunction.
Psychological Backgrounds of Subjects
To address trauma encountered during childhood and adolescence, three questionnaires have been utilized in the EEG literature:
1) The Early Life Stress Questionnaire (ELSQ), which queries experience of adverse childhood events including abuse, neglect, natural disasters, major illness, adoption, poverty, and domestic violence
2) The Childhood Trauma Questionnaire (CTQ), which focuses on multiple facets of abuse and neglect and
3) The Childhood Experiences of Victimization Questionnaire (CEVQ), which evaluates peer bullying, corporal punishment, domestic violence, and facets of abuse (emotional, physical, and sexual)
In contrast to early life trauma, two scales capture traumatic symptoms suffered as a result of military service:
1) The Mississippi Scale for Combat-Related PTSD (M-PTSD) queries DSM-IV PTSD symptoms as well as comorbid substance use, suicide, and depression and
2) The Combat Exposure Scale (CES) is a short questionnaire determining degree of trauma experienced in the military (from “light” to “heavy”) that is moderately correlated with M-PTSD
Treatments [14]
Psychotherapies are considered first-line treatments for PTSD. These include cognitive behavioral therapy (CBT), exposure and cognitive therapies, and eye movement desensitization and reprocessing therapy (EMDR).
This category covers both pharmacological and psychological treatments, as well as non-pharmaceutical physical treatments such as transcranial magnetic stimulation (TMS).
Physical [15]
Physical treatments for PTSD include medications such as antidepressants, anticonvulsants, antipsychotics, and psychedelics, as well as non-pharmaceutical treatments such as transcranial magnetic stimulation, exercise, and acupuncture.
• Non-pharmaceutical
• Acupuncture
• Biofeedback
• Exercise
• Hyperbaric oxygen
• Transcranial magnetic stimulation
Pharmaceutical [16]
Pharmaceutical treatment options for PTSD primarily include antidepressants. Several other medications have been investigated for PTSD, these include antipsychotics, cannabinoids, and psychedelics, among others. Medications have also been investigated as preventative measures for PTSD following exposure to trauma.
• All pharmaceutical treatments for prevention of PTSD
• All pharmaceutical vs. psychological treatments
• Alpha blockers
• Anticonvulsants
• Antidepressants
• Antipsychotics
• Benzodiazepines
• Glutamatergic modulators
• Medicinal cannabis
• Oxytocin
• Placebo effect
• Psychedelics
Psychotherapy [17]
Psychotherapies are first-line treatments for PTSD. They include cognitive behavioral therapy (CBT), cognitive and exposure therapies, and eye movement desensitization and reprocessing (EMDR), among other therapies. There are also therapies that target specific symptoms and patient groups.
• Therapies
• Acceptance and commitment therapy
• All psychological therapies for PTSD
• Animal-assisted psychotherapy
• Brief eclectic psychotherapy
• Cognitive behavioral therapy
• Cognitive therapies
• Creative arts therapy
• Emotion-focused therapies
• Emotional freedom techniques
• Exposure therapies
• Expressive writing
• Eye movement desensitization and reprocessing
• Family therapies
• Group therapies
• Hypnotherapy
• ICU diaries
• Imagery rehearsal therapy
• Interpersonal psychotherapy
• Memory specificity training
• Metacognitive therapy
• Mindfulness and meditation
• Narrative exposure therapy
• Present-centred therapy
• Psychoeducation
• Self-help treatment
• Stress inoculation training
• Stress management
• Structured approach therapy
• Supportive counselling
• Telemental health
• Trauma affect regulation
EEG
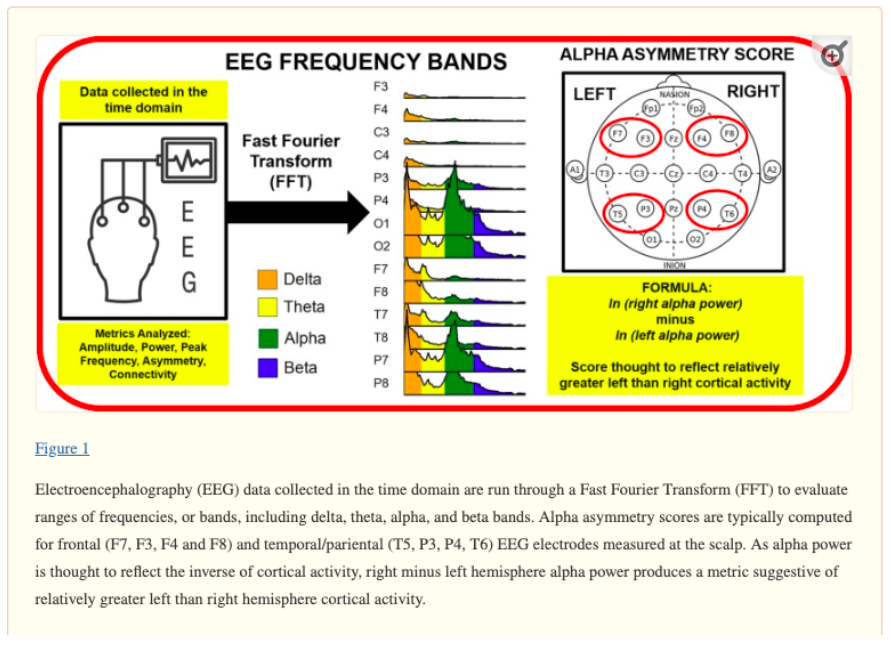
What is electroencephalography (EEG) and PTSD? [18]
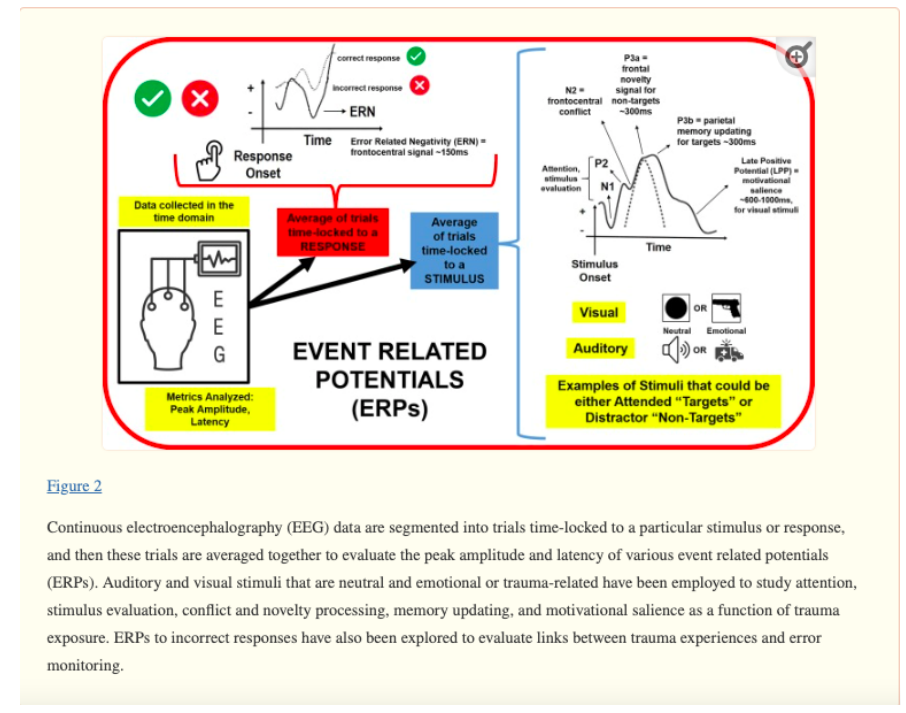
Electroencephalography (EEG) has been used to study changes in brain functioning in people with PTSD. It uses electrodes on the scalp to measure electrical activity from the brain. Quantitative spectral EEG investigates several waveforms so the activity can be measured. However, EEG also gives rise to event related potentials (ERP). These measure the EEG activity directly evoked by a stimulus, often using cognitive or perceptual stimuli.
P300, also referred to as P3, may be the ERP most suitable for the assessment of PTSD. This is because it is well documented, and with the appropriate stimulus can convey information about attention and working memory. P300 refers to a spike in activity approximately 300ms following presentation of a target stimulus. The target stimulus is alternated with standard stimuli to create an ‘oddball’ paradigm, which is most commonly auditory. In this paradigm, the subject must respond only to the infrequent target stimulus rather than the frequent standard stimulus. The amplitude of the P300 response is proportional to the amount of attentional resource devoted to the task and the degree of information processing required. The latency is considered a measure of stimulus classification speed, unrelated to behavioral response time.
What is the evidence for changes in electroencephalography (EEG) readings in people with PTSD?
Moderate quality evidence found large increases in P3a (involuntary attention) amplitude with trauma-related distractors in people with PTSD compared to trauma-exposed people without PTSD. Medium-sized effects showed P3b (voluntary attention) amplitude was also increased with trauma-related distractors in people with PTSD. This was found in frontal and central brain regions, but not in parietal brain regions.
There were medium-sized reductions in P3b amplitude with neutral distractors in people with PTSD compared to healthy controls. There were also small reductions in P3wm (working memory) amplitude with neutral distractors in parietal, but not in frontal and central regions of people with PTSD.
The Electrical Aftermath: Brain Signals of Posttraumatic Stress Disorder Filtered through a Clinical Lens was evaluated [19].
Mamona Butt et al., aimed to identify patterns of electrical signals identified using electroencephalography (EEG) linked to posttraumatic stress disorder (PTSD) diagnosis and symptom dimensions. We filter EEG findings through a clinical lens, evaluating nuances in findings according to study criteria and participant characteristics.
Within the EEG frequency domain, greater right than left parietal asymmetry in alpha band power is the most promising marker of PTSD symptoms and is linked to exaggerated physiological arousal that may impair filtering of environmental distractors.
The most consistent findings within the EEG time domain focused on event related potentials (ERPs) include: 1) exaggerated frontocentral responses (contingent negative variation, mismatch negativity, and P3a amplitudes) to task-irrelevant distractors, and 2) attenuated parietal responses (P3b amplitudes) to task-relevant target stimuli. These findings suggest that some individuals with PTSD suffer from attention dysregulation, which could contribute to problems concentrating on daily tasks and goals in lieu of threatening distractors. Future research investigating the utility of alpha asymmetry and frontoparietal ERPs as diagnostic and predictive biomarkers or intervention targets are recommended.
New Technologies in EEG Telemetry
Recent development of bio-integrated technology based on wearable and implantable electronics has made it possible to continuously measure bioinformation, such as physiological, electrophysiological, and chemical signals. Such devices can be utilized in a human-machine interface (HMI) integrated with advanced Internet of Things (IoT) and artificial intelligence (AI) technologies.
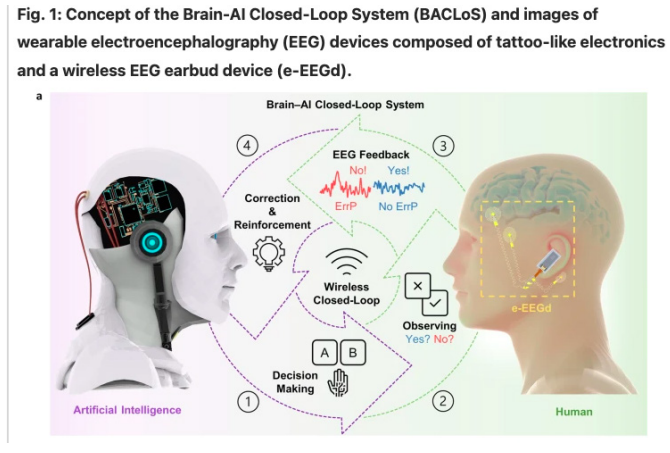
Wearable EEG electronics for a Brain-AI Closed-Loop System
Joo Hwan Shin, et al. have described a Brain-AI Closed-Loop System (BACLoS), a wireless interaction platform that enables human brain wave analysis and transfers results to AI to verify and enhance AI decision-making [20].
Human nonverbal communication tools are very ambiguous and difficult to transfer to machines or artificial intelligence (AI). If the AI understands the mental state behind a user’s decision, it can learn more appropriate decisions even in unclear situations. We introduce the Brain-AI Closed-Loop System (BACLoS), a wireless interaction platform that enables human brain wave analysis and transfers results to AI to verify and enhance AI decision-making. We developed a wireless earbud-like electroencephalography (EEG) measurement device, combined with tattoo-like electrodes and connectors, which enables continuous recording of high- quality EEG signals, especially the error-related potential (ErrP). The sensor measures the ErrP signals, which reflects the human cognitive consequences of an unpredicted machine response. The AI corrects or reinforces decisions depending on the presence or absence of the ErrP signals, which is determined by deep learning classification of the received EEG data. We demonstrate the BACLoS for AI-based machines, including autonomous driving vehicles, maze solvers, and assistant interfaces.
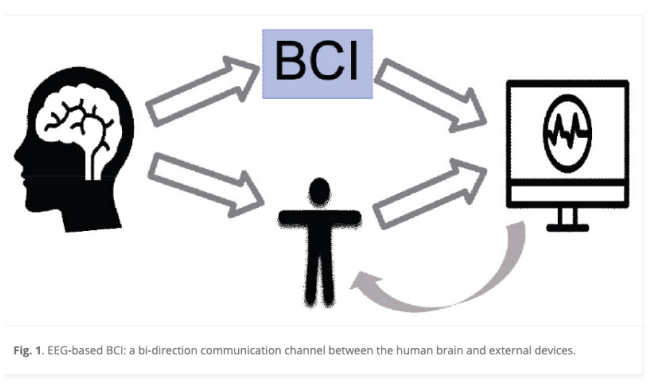
Use of AI EEG-based brai-computer interfaces and applications
Zehong Cao has reviewed last ten years of interactive technologies and AI [21]. The advancement in neuroscience and computer science promotes the ability of the human brain to communicate and interact with the environment, making brain-computer interface (BCI) top interdisciplinary research. Furthermore, with the modern technology advancement in artificial intelligence (AI), including machine learning (ML) and deep learning (DL) methods, there is vast growing interest in the electroencephalogram (EEG)- based BCIs for AI-related visual, literal, and motion applications. In this review study, the literature on mainstreams of AI for the EEG-based BCI applications is investigated to fill gaps in the interdisciplinary BCI field. Specifically, the EEG signals and their main applications in BCI are first briefly introduced. Next, the latest AI technologies, including the ML and DL models, are presented to monitor and feedback human cognitive states. Finally, some BCI-inspired AI applications, including computer vision, natural language processing, and robotic control applications, are presented. The future research directions of the EEG-based BCI are highlighted in line with the AI technologies and applications.
Based on the EEG-based BCI classification algorithms in the past ten years [11], the classifier options that go with different kinds of EEG patterns/features were reviewed as follows:
EEG features with noise and/or outliers
We suggest choosing regularized classifiers, such as the SVM, which is suitable for handling outliers. The discriminative classifiers [12] may be a back-up choice, as it showed better performance compared to generative classifiers in the presence of noise or outliers.
EEG features with high dimensions
The SVM may be the most suitable classifier for processing high- dimensional feature vectors. Alternatively, using dimensionality reduction techniques for feature selection may solve this problem as well.
EEG features with non-stationarity
Since combination strategy classifiers reduce the information variance, some stable linear classifiers, such as LDA and SVM, are suitable for testing the classification performance.
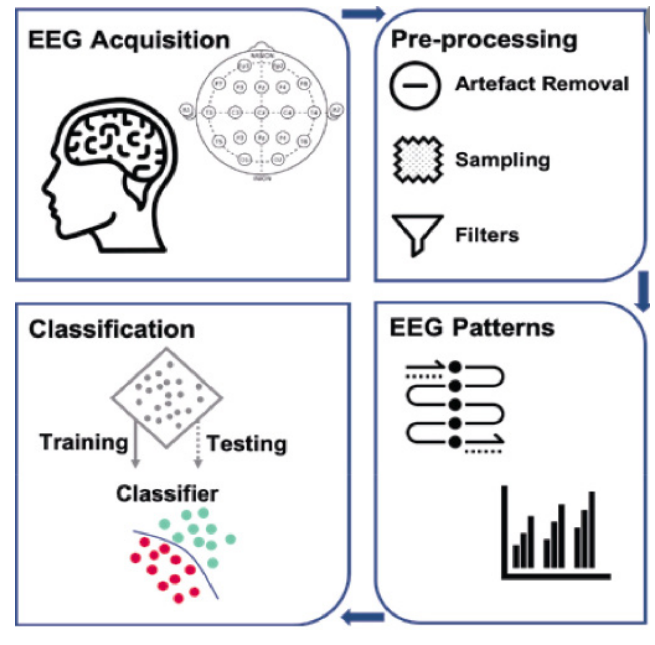
Neural Decoding of EEG Signals with Machine Learning
Electroencephalography (EEG) is a non-invasive technique used to record the brain’s evoked and induced electrical activity from the scalp. Artificial intelligence, particularly machine learning (ML) and deep learning (DL) algorithms, are increasingly being applied to EEG data for pattern analysis, group membership classification, and brain-computer interface purposes. This study aimed to systematically review recent advances in ML and DL supervised models for decoding and classifying EEG signals. Moreover, this article provides a comprehensive review of the state-of-the-art techniques used for EEG signal preprocessing and feature extraction. To this end, several academic databases were searched to explore relevant studies from the year 2000 to the present.
Our results showed that the application of ML and DL in both mental workload and motor imagery tasks has received substantial attention in recent years. A total of 75% of DL studies applied convolutional neural networks with various learning algorithms, and 36% of ML studies achieved competitive accuracy by using a support vector machine algorithm. Wavelet transform was found to be the most common feature extraction method used for all types of tasks. We further examined the specific feature extraction methods and end classifier recommendations discovered in this systematic review.
The human brain is a complex system containing approximately 100 billion neurons and trillions of synaptic connections [1,2]. The brain’s electrical activity became a research focus in the 19th century when Richard Caton recorded brain signals from rabbits [3,4]. Brain recordings were also performed by Hans Berger, the first person to record electroencephalogram (EEG) signals from the human scalp [5]. EEG-based research has since increased significantly, and EEG is now the most commonly used noninvasive tool to study dynamic signatures in the human brain [6,7]. EEG signals measure voltage fluctuations at the scalp and reflect the instantaneous superposition of electric dipoles, primarily from dendritic inputs to large pyramidal cells in the neuropil [8]. Signals traveling in white matter have traditionally been thought to be too fast to superimpose temporally, although recent cable theoretic models [9] and empirical work [10] suggest that white matter may also contribute to brain rhythms measured at the scalp.
Classically, the three primary forms of the brain’s activity based on EEG signals are brain waves, event-related potential (ERP), and steady-state visual evoked potentials (SSVEPs). Among those, brain waves are most commonly used in EEG signal analysis for different types of tasks. Brain waves have been categorized in terms of five frequency bands: delta, 0.5-4 Hz; theta, 4-8 Hz; alpha, 8-13 Hz; beta, 13-30 Hz; and gamma, 30-150 Hz [11]. Other classifications of brain signals can be found in previous publications [12,13].
EEG is a low cost, noninvasive neuroimaging technique that provides high temporal resolution recordings of dynamic signatures in the brain; it has therefore become an indispensable tool in a variety of applications, including clinical diagnosis of a range of epileptic seizure types [14,15], brain-computer interface (BCI) systems, sleep analysis, and decoding behavioral activity [6,16,17]. When interpreted carefully [18], classification tools can be used not only for prediction but also to gain neuroscientific knowledge. However, EEG signals are complex, high-dimensional the temporal domain. Therefore, careful preprocessing is often required to remove artifacts [20], particularly when EEG data are collected concurrently and in the MRI setting [21].
Maham Saeidi et al. have reviewed obtained 764 articles from all database searches after the removal of duplicates. To determine which articles were appropriate to consider in this study, they reviewed all abstracts to determine whether the findings met their inclusion criteria. A total of 254 articles remained after this evaluation.
Research Questions (RQs)
• What classification tasks have received the most attention with the introduction of ML and DL algorithms and the use of EEG brain data?
• Which feature extraction methods were used for each task to extract appropriate inputs for ML and DL classifiers?
• What are the most frequently used ML and DL algorithms for EEG data processing?
• Which specific ML and DL models are suitable for classifying EEG data involving different types of tasks?
Imaging Studies fMRI and PET [23]
What is brain functioning in PTSD, measured with fMRI, PET and SPECT?
Functional magnetic resonance imaging (fMRI) measures blood flow to determine activation and deactivation of specific brain regions. Positron emission tomography (PET) is a nuclear based imaging technique that utilizes a radioactive tracer to visualize functional brain activity. The radioisotope tracers are coupled with a biological molecule such as glucose, which is used during cellular metabolism and can be used to highlight areas with changes in metabolic activity. Single-photon emission computed tomography (SPECT) offers more limited spatial and temporal resolution than PET but is less expensive as it does not require a cyclotron in close proximity.
What is the evidence for changes in brain functioning in PTSD?
Compared to non-trauma-exposed controls, moderate to high quality evidence found clusters of increased activation in PTSD during resting state or task processing in bilateral anterior insula, left amygdala, left putamen, left precuneus, right hippocampus, right middle frontal gyrus fusiform gyrus, and right postcentral gyrus. Clusters of decreased activation were found in bilateral precentral gyrus, left angular gyrus, left supramarginal gyrus, left middle frontal gyrus, right posterior cingulate cortex, right medial prefrontal cortex, and right caudate nucleus.
Compared to trauma-exposed controls, people with PTSD showed clusters of increased activation in the left fusiform gyrus, right precuneus, right thalamus, dorsal anterior cingulate cortex, and lateral medial temporal lobe. Clusters of decreased activation were found in the left thalamus, left parahippocampal gyrus, right medial prefrontal cortex, right orbitofrontal cortex, right precentral gyrus, left frontal pole, bilateral inferior frontal gyrus, bilateral middle frontal gyrus, and dorsal anterior cingulate cortex.
During trauma-related autobiographical memory tasks, moderate quality evidence found increased clusters of activation in PTSD
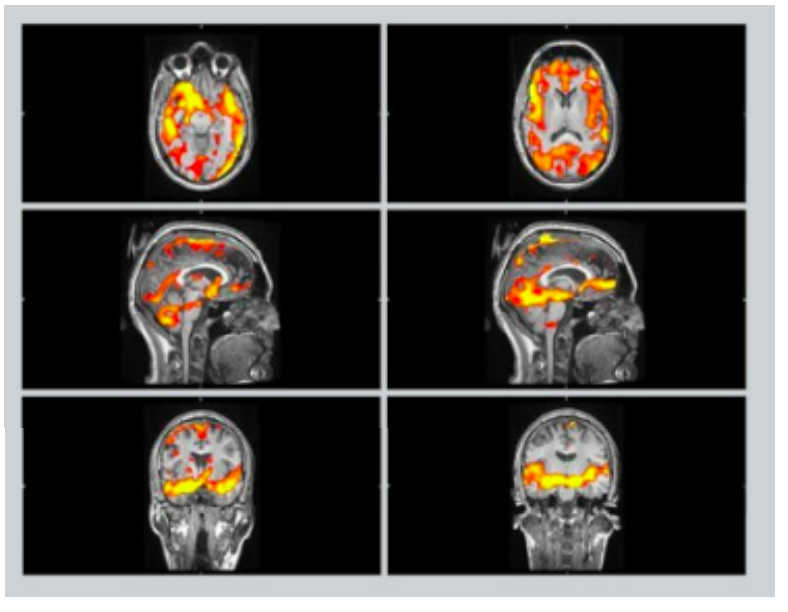
compared to trauma-exposed controls in the left posterior cingulate extending into the precuneus and the mid-cingulate cortex, right parahippocampal gyrus, and the right dorsal anterior cingulate cortex. There were clusters of decreased activation in PTSD in the right ventromedial prefrontal cortex extending into the orbitofrontal and the perigenual anterior cingulate, and the left midline nucleus of the thalamus extending into the medial and the lateral dorsal nuclei and the left angular gyrus.
Compared to people with major depressive disorder, there was more activation in the PTSD group during negative affect processing in the left inferior frontal gyrus (including ventrolateral prefrontal cortex), bilateral amygdala and hippocampus, left superior frontal gyrus, dorsolateral prefrontal gyrus, and right middle frontal gyrus.
Compared to people with borderline personality disorder, moderate to low quality evidence found more activation in the PTSD group during negative affect processing in the left inferior frontal gyrus, left middle temporal gyrus, right striatum, bilateral middle frontal gyrus (including parts of the left superior frontal gyrus, dorsolateral), ventral premotor cortex, and the right posterior parietal cortex.
Outcome Analytic Tools
Functioning and Other Outcomes [24]
Below is an alphabetical list of measures of functioning and other outcomes related to PTSD and trauma. For each measure, a brief description, sample items, versions and references are provided. Information on how to obtain the measure is also provided.
Endorsed and Anticipated Stigma Inventory (EASI)
Inventory of Psychosocial Functioning (IPF)
Late-Onset Stress Symptomatology (LOSS) Scale Posttraumatic Maladaptive Beliefs Scale (PMBS)
Well-Being Inventory (WBI)
Measure availability
We provide information on a variety of measures assessing trauma and PTSD. These measures are intended for use by qualified mental health professionals and researchers. Measures authored by National Center staff are available as direct downloads or by request. Measures developed outside of the National Center can be requested via contact information available on the information page for the specific measure.
Reference guides used
https://www.ptsd.va.gov/professional/assessment/overview/use_pilots_assessments.asp
Literature Searches Databases used
https://www.proquest.com/ptsdpubs/indexNationalCenterforPTSD[25]
Plan Logistics
1. Physical plan for structure of institute, planning operations
2. Division into
A. Diagnostic wing including clinic, imaging, electrophysiology, neurobehavioral labs.
B. therapeutic wing including hyperbaric chambers, therapeutic areas, magnetic brain stimulation clean rooms, individual counselling areas, group therapy areas,
3. Administrative area for management team, grant team research coordinators and writers.
4. Time-Line for gathering the team of scientists and academics from each field.
5. Hiring of staff personnel
6. Engaging with KUPOT and Israel military for contracts and grants
7. Reaching the population cohort through print social media advertizing
References
1. Elaine Scarry. The Body in Pain: The Making and Unmaking of the World. 1985.
2. Frank A. The wounded storyteller: body, illness and ethics.Chicagod London: University of Chicago Press. 1995.
3. Greenhalgh T. Intuition and Evidence- Uneasy Bedfellows. Br J Gen Pract. 2002; 52: 395-400.
4. Yossi Levi-Belz, Yoav Groweiss, Carmel Blank, et al. PTSD depression and anxiety after the October 7, 2023 attack in Israel: a nationwide prospective study. eClinical Medicine. 2024; 68: 102418.
5. Dana Katsoty, Michal Greidinger, Yuval Neria, et al. A Prediction Model of PTSD in the Israeli Population in the Aftermath of October 7th, 2023 Terrorist Attack and the Israel-Hamas War. Medrxiv. 2024.
6. PTSD depression and anxiety nearly doubles in Israel in aftermath of Hamas attack. Medicalxpress. 2024. https://medicalxpress.com/news/2024-01-ptsd-depression-anxiety-israel-aftermath.html
7. Yaakov SG Hoffman, Gary M Diamond, Joshua D Lipsitz. The challenge of estimating PTSD prevalence in the context of ongoing trauma: The example of Israel during the Second Intifada. Journal of Anxiety Disorders. 2011; 25: 788-793.
8. Clare Killikelly, Louisa Lorenz, Susanna Bauer, et al. Prolonged grief disorder Its co-occurrence with adjustment disorder and post-traumatic stress disorder in a bereaved Israeli general-population sample. J Affect Disord. 2019; 249: 307-314.
9. https://www.ptsd.va.gov/understand/what/ptsd_basics.asp
10. https://library.neura.edu.au/ptsd-library/assessment-and-diagnosis-ptsd-library/diagnosis/index.html
12. https://library.neura.edu.au/category/ptsd-library/signs-and-symptoms-ptsd-library/cognition-signs-and-symptoms-ptsd- library/index.html
13. https://library.neura.edu.au/category/ptsd-library/signs-and-symptoms-ptsd-library/general-signs-and-symptoms-signs- and-symptoms-ptsd-library/index.html
14. https://library.neura.edu.au/category/ptsd-library/treatment/index.html
15. https://library.neura.edu.au/category/ptsd-library/treatment/physical-treatments/index.html
17. https://library.neura.edu.au/category/ptsd-library/treatment/psychological-treatments/index.html
19. Mamona Butt, Elizabeth Espinal, Robin L Aupperle, et al. The Electrical Aftermath: Brain Signals of Posttraumatic Stress Disorder Filtered Through a Clinical Lens. Front Psychiatry. 2019; 10: 368.
20. Joo Hwan Shin, Junmo Kwon, Jong Uk Kim. Wearable EEG electronics for a Brain–AI ClosedLoop System to enhance autonomous machine decision-making. npj Flexible Electronics. 2022; 6: 32.
21. Zehong Cao. A review of artificial intelligence for EEG-based brain-computer interfaces and applications. Brain Sci Adv. 2021; 6: 162-170.
22. Maham Saeidi, Waldemar Karwowski, Farzad V Farahani, et al. Neural Decoding of EEG Signals with Machine Learning A Systematic Review. Brain Sci. 2021; 11: 1525.
24. https:// www.ptsd.va.gov/professional/ assessment/ functioning-other/index.asp
25. https://www.ptsd.va.gov/publications/electronic_pubs.asp