Agenesia of The Pulmonary Valve in A Young Guinean of 29 Years
Author'(s): Bah Mamadou Bassirou1, Balde Mamadou Dadhi1, Balde Elhadj Yaya1, Beavogui Mariam1, Camara Abdoulaye1*, Diallo Mamadou1, Barry Ibrahima Sory1, Ngaide Aliou Alassane3, Balde Mamadou Aliou1, Kone Alpha2, Sorya Ibamy Adrien Adrien1, Balde Thierno Hamidou4
1Ignace Deen cardiology department, Guinea.
2Department of cardiology Donka, Guinea
3Department of cardiology Grand Yoff, Senegal.
4Radiology department Ignace Deen, Guinea.
*Correspondence:
Camara Abdoulaye, Ignace Deen cardiology department, Guinea,Tel : 224 621 226 681 /664 933 740, ID: 0000-0002-8647-4383.
Received: 08 September 2020; Accepted: 27 September 2020
Citation: Bah Mamadou Bassirou, Balde Mamadou Dadhi, Balde Elhadj Yaya, et al. Agenesia of The Pulmonary Valve in A Young Guinean of 29 Years. Cardiol Vasc Res. 2020; 4(4): 1-4.
Abstract
The objective of this study was to describe the agenesis of the pulmonary valve in a young man of 29 years. Pulmonary valve agenesis is a rare birth defect, defined by complete absence or severe hypoplasia of the pulmonary sigmoid. It was a 29-yearold Guinean patient, artist with no particular history who consulted us for exercise dyspnea. Cardiac Doppler ultrasound (Figure 3,4,5) had highlighted a right auricle and left cavities of normal size, a good bi ventricular systolic function (FEVG = 60% TAPSE = 18mm). There was an 18 mm wide interventricular communication (VIC) with bidirectional shunt, agenesis of the pulmonary valve with an aneurysmal trunk and pulmonary branches as well as a tight pulmonary stenosis with a maximum gradient VD / AP = 134mmHg.
There was significant pulmonary insufficiency. Agenesis of the pulmonary valve is a rare congenital heart disease.
Clinical tolerance depends on the severity of the bronchial compression. This relative clinical tolerance as well as the absence of training on screening for congenital heart disease are responsible for delayed diagnosis in our context. However, a cardiac doppler ultrasound confirms the diagnosis.
Keywords
Introduction
Pulmonary valve agenesis is a rare birth defect, defined by complete absence or severe hypoplasia of the pulmonary sigmoid [1]. In the majority of cases, it is associated with other anomalies, in particular isolated inter ventricular communication [1]. It is associated in 3 to 6% of cases with a tetralogy of Fallot (TF) and is generally responsible for significant respiratory symptoms, due to bronchial compression by the pulmonary arteries (PA) strongly dilated [1- 3]. It is characterized by a weak cyanosis, a symptomatology of bronchial obstruction especially in expiration, simulating an asthma [4,5]. Nowadays, it can be easily diagnosed by a cardiac Doppler ultrasound due to its typical ultrasound characteristics, such as aneurysmal dilation of the pulmonary artery, significant pulmonary leakage and interventricular defect [6]. The exploration of congenital heart disease by angioscanography is a new technique proposed in addition to cardiac ultrasound and angiography [7]. In sub-Saharan Africa congenital heart disease (CC) in general poses a real problem of diagnosis and treatment because of a very deficient technical platform. The originality of this clinical case results from the fact that similar cases have not been described in Guinea.
This study has the advantage of allowing the description of the clinical, paraclinical and therapeutic aspects of agenesis of the pulmonary valve discovered late in a young man of 29 years.
Observation
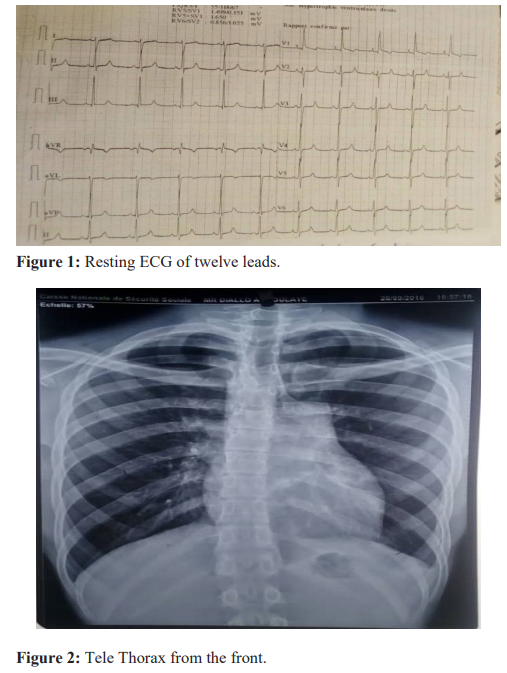
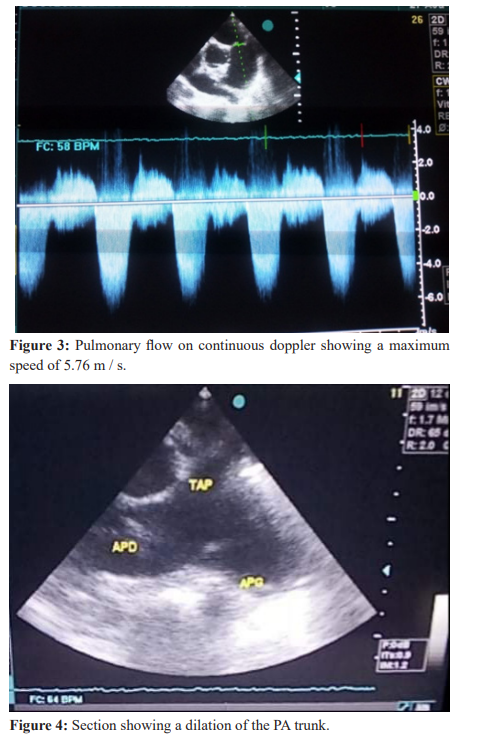
It was a 29-year-old Guinean patient, artist with no specific history who consulted us for effort dyspnea. The start of the symptomatology dates back to the age of 5 years according to the parents, marked by dyspnea of effort limiting his physical performance around childish games. At the age of 16, he consulted a general practitioner who would have evoked a cardiopathy congenital, but at the time the diagnosis was not refined. He remained symptomatic with episodes of dyspnea with intense efforts, it is in this context that the patient consulted us for an etiological assessment. He was smoking due to 16 Packs year (PA). On physical examination: the hemodynamic constants were as follows: blood pressure = 120 / 70mmhg; heart rate at 61 beats / minute; Height = 1.77m; SaO2 in ambient air at 85%. The examination of the general condition had found a satisfactory general condition with a WHO index 1. The integuments and conjunctiva well colored with good psychomotor development. There was a labial cyanosis associated with digital hippocratism. The cardiovascular examination noted a positive Harzer sign associated with a murmur of the systolic-diastolic pulmonary focus of 4/6, simmering. No peripheral signs of heart failure. The electrocardiogram had recorded (Figure 1): a regular sinus rhythm; a heart rate of 64 cycles per minute; a 120 degree right axis; a large R wave in V1 with a persistence of the S wave in V6 evoking a right ventricular hypertrophy (HVD). The frontal chest radiography had shown a bulging of the left middle arch, a point of the over diaphragmatic heart in connection with a dilation of the pulmonary artery and of the DV associated with a peripheral hypovascularization (Figure 2). Cardiac (Figure 3,4,5) had highlighted a right auricle and left cavities of normal size, a good bi ventricular systolic function (FEVG = 60% TAPSE = 18mm).
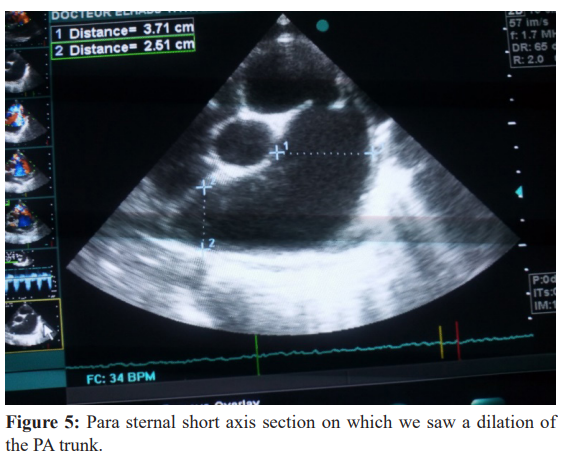
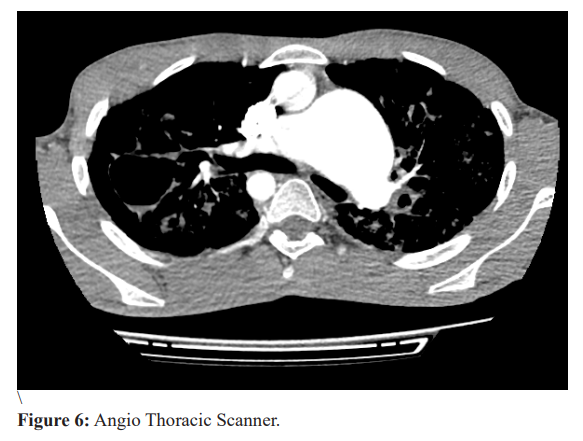
There was an 18 mm wide interventricular communication (VIC) with bidirectional shunt, agenesis of the pulmonary valve with an aneurysmal trunk and pulmonary branches as well as a tight pulmonary stenosis with a maximum gradient VD / AP = 134mmHg. There was significant pulmonary insufficiency. The aorta straddles the septum (50% dextrosition).There is mitro aortic continuity. Functional respiratory exploration (FRT) did not show obstructive ventilatory disorders. The tiffeneau index is higher than 70%. The CT angiography (Figure 6) had shown significant dilation of the pulmonary artery trunk measured at 65mm antero posterior diameter, 89mm transverse diameter and 82mm cranio- caudal diameter. The establishment of a VD / AP tube, possibly a plasty of the pulmonary branches are envisaged.
The progress is relatively good, the patient is independent and shows no signs of heart failure.
Discussion
We report the case of a patient we are monitoring at Ignace Deen’s cardiology department for pulmonary valve agenesis. It is a rare birth defect characterized by hypoplasia of the pulmonary sigmoid [1].
The case we report in our study is a young patient, aged 29 years. Affangla et al. In a similar case report in Senegal in 2014, an age of discovery close to that of our case was already reported, which was 24 years [1]. This indicates the delayed diagnosis of congenital heart diseases in sub-Saharan Africa, unlike in developed countries such as the United States where 95% of children are already hospitalized before the age of 1 year, in Switzerland about 90% of heart diseases are detected before the first year of life [7].
Furthermore, ante natal diagnosis of these congenital heart diseases would be possible through ultrasound [7]. Ashok et al. have already reported a case of ante natal diagnosis of agenesis of the pulmonary valves from the 27th week of amenorrhea [1]. This diagnostic delay in our context could be multi-factorial, including the weakness of the technical platform, the scarcity of well-trained specialists on prenatal screening for congenital malformations as well as the low level of information of the population on the need for regular monitoring. During pregnancy Clinical tolerance is most often poor associating respiratory signs by bronchial compression secondary to the aneurysmal pulmonary arteries with signs of heart failure. This malformation can sometimes be relatively tolerated and discovered in adulthood [8]. Our patient consulted us for relatively well tolerated stress dyspnea that occurred since the age of 5, sometimes with a restriction during play efforts with children of the same age.
The worsening of exercise dyspnea with recurrent squatting periods associated with systolic murmur of pulmonary stenosis could suggest a Tetralogy of Fallot. However, the Cardiac Doppler ultrasound was of great help in correcting the diagnosis.
The physical examination of our patient had revealed signs of chronic hypoxia consisting of labial cyanosis and digital hippocratism. Affanglan et al. In their case report have notified the same signs. This result would be due to the delay in diagnosing the disease in our context [1]. The frontal chest X-ray (Figure 2) contributed to the diagnosis by showing bulging of the left middle arch in connection with an dilation of the artery pulmonary associated with peripheral hypovascularization. Diane et al. Have already demonstrated the interest of radiography for the diagnosis of agenesis of the pulmonary valves in a case report relating to the Unrepaired Tetralogy of Fallot with pulmonary valve absent in a 16 year old boy, it had made it possible to highlight an enlarged central pulmonary artery and moderate cardiomegaly [9]. Functional respiratory exploration is necessary to confirm respiratory failure, the severity of which depends on the earliness of the diagnosis [10].
The functional respiratory exploration (FRA) of our patient did not show obstructive ventilatory disorders, the tiffeneau index greater than 70%. This result could explain the absence of severity of the bronchial symptoms. In our case, the ultrasound (Figure 3) confirmed the diagnosis by highlighting pulmonary valve hypoplasia, tight pulmonary stenosis with a maximum gradient of 134 mmhg and 18 mm wide inter ventricular communication (VIC) with bidirectional shunt. The aorta straddles the septum (50% dextrosition). There is mitro-aortic continuity. Surgical repair preserving the pulmonary valve in patients with a severely hypoplastic pulmonary valve has been difficult and controversial [11]. In a context where there is no cardiac surgery, the only medical treatment we have used is beta-blocker (Propranolol) and close monitoring.We noted a slight clinical improvement, however medical evacuation is being considered for cardiac surgery.
Conclusion
Pulmonary valve agenesis is a rare congenital heart disease. Clinical tolerance depends on the severity of the bronchial compression. This relative clinical tolerance as well as the absence of training on screening for congenital heart disease are responsible for delayed diagnosis in our context.
However, a cardiac doppler ultrasound confirms the diagnosis.
References
- Affangla DA, Leye M, Dia A, et al. Agenesis of the pulmonary valve: about a case in a Senegalese woman of 24 years old. Pan Afr Med J. 2014; 18: 76.
- Muhammad Y, Harold M, Burkhart, et al. Tetralogy of Fallot with Absent Pulmonary Valve Syndrome. Heart text Inst J. 2014; 41: 664-667.
- Adler M, Christpher C, Rbider G, et al. Lung function tests in infants with Fallot tetralogy and absent pulmonary valve syndrome. Ann Pediatr Cardiol. 2015; 8: 108-112.
- Khayat M. Surgery of the tetralogy of Fallot: about 64 cases. State doctorate thesis in medicine CHU Hassan II of Fez. 2018 in Morocco.
- Sachin T, Aabha D, Shiv K, et al. Medium-term results of the correction of tetralogy of Fallot with absent pulmonary valve. Indian heart J. 2017; 69: 767-771.
- Wen J, Zhong L, Jun J, et al. Prenatal ultrasound diagnosis of absent pulmonary valve syndrome: A case report. Medicine (Baltimore). 2017; 96: 7744-7747.
- Badia A. Congenital heart disease: Experience of the CHU Mohamed VI. State doctorate thesis in medicine. 2010.
- Diana E Drogalis-Kim, Brian L Reemtsen, Leigh Christopher Reardon. Unrepaired tetralogy of Fallot with missing pulmonary valve in a 16-year-old boy with mild symptoms. Tex Coeur Inst J. 2016; 43: 517-519.
- Alain B, Laurent F, Marline L. Practical pediar cardiology.4th ed. 2012.
- Hiroki I, Noritaka O, Massaya M, et al. Technical modification allowing the repair with pulmonary valve valve of a severely hypoplastic pulmonary ring in patients with a tetralogy of Fallot. Interagir Cardiovasc Thorac Surg. 2013; 16: 802-807.