An Algorithm for Evaluation and Management of Diabetic Foot Ulcers
Author(s): MB Strauss*, C Ko, LQ Lu, H Moon, and Miller SS
Memorial Care Long Beach Medical Center, 2801 Atlantic Avenue, Long Beach, California.
*Correspondence:
Michael B. Strauss, MD. Memorial Care Long Beach Medical Center, 2801 Atlantic Avenue, Long Beach, California 90801.
Received: 28 January 2021 Accepted: 24 February 2021
Citation: Strauss MB, Ko C, Lu LQ, et al. An Algorithm for Evaluation and Management of Diabetic Foot Ulcers. Diabetes Complications. 2021; 5(1); 1-5.
Abstract
Introduction: Diabetic foot ulcers (DFUs) are the leading cause of morbidity and amputations in the diabetic population. The Long Beach Wound Score (LBWS) is a tool that provides objectivity to evaluation of DFUs and rationale for their management.
With both tested reliability and published validity, the LBWS is unique among diabetic foot as well as other wound classification systems in this regard and is fundamental to our algorithm.
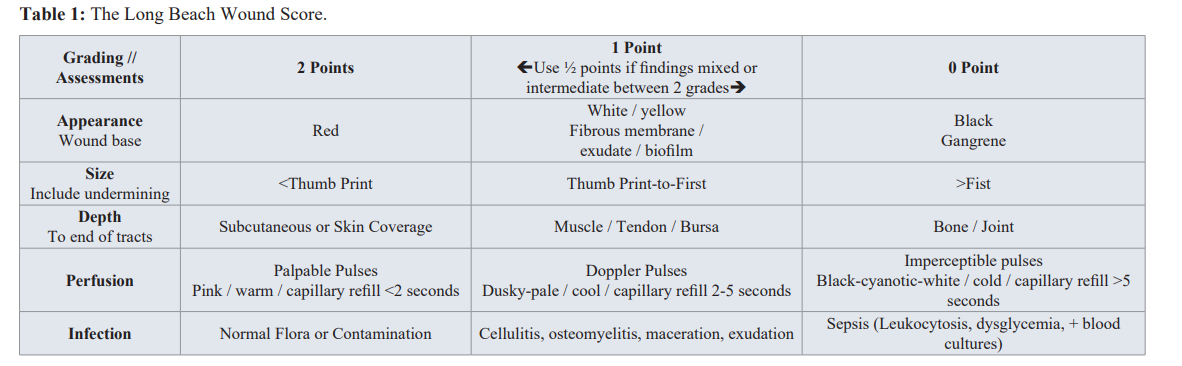
Methods: We generated an algorithm that is based on the three wound types, i.e. Healthy, Problem, and End-stage objectively derived from the LBWS. Five assessments each graded from 2-points (best) to 0-points (worse) using objective criteria for each grade establishes the 0 to 10-point LBWS. Each wound type has specific management requirements and predicable outcomes.
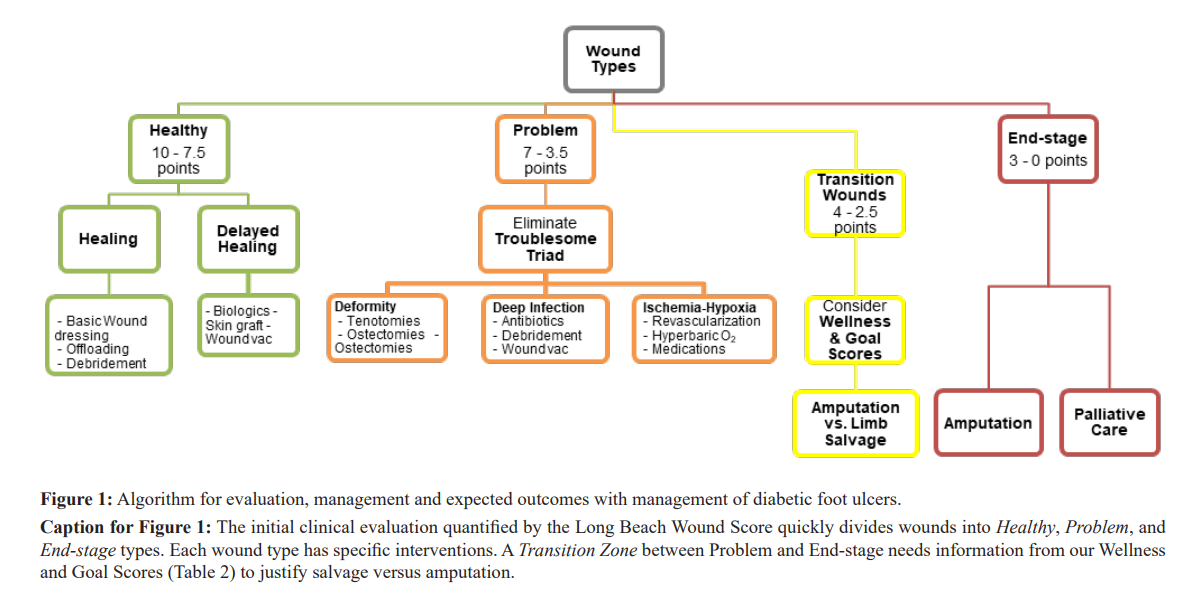
Results: Our algorithm shows that Healthy wounds (7.5 to 10-points) heal with few exceptions with the simplest of interventions. Problem wounds (3.5 to 7-points) typically have remedial causes and will usually heal by correcting the causes. End-stage wounds invariable require an amputation for management. Salvage attempt versus major amputation of a wound in a Transition zone (2.5 to 4-points) requires information about the patient’s health status and intentions for management decisions.
Conclusions: Use of our algorithm based on the LBWS optimizes management, prevents delays in initiating needed interventions, quantifies improvement, and ensures cost effectiveness in managing wounds in general and DFUs in particular
Keywords
Introduction
Enormous resources and investments are devoted to wound management, especially for diabetic foot ulcers (DFUs). Wound management can range from a few dollars for moistened gauze to $10,000 or more for a bioengineered dressing that requires application in an operating room. Unfortunately, logical management of DFUs is not inherent in commonly used scoring systems. The Long Beach Wound Score (LBWS) is a tool that quantifies wounds into Healthy, Problem and End-stage types using objective findings. From this classification system, rational and cost-effective interventions become obvious. It shows when simple wound dressings, offloading, biologic skin substitutes, hyperbaric oxygen therapy, antibiotics; debridements, revascularizations, amputations and palliative care only are indicated. The algorithm also utilizes Wellness and Goal Scores when decision making between limb salvage and amputation needs further justification.
The LBWS is obtained by summating five essential assessments that are essential for evaluating a wound. The assessments include
1) Appearance of the wound base,
2) Size (including recesses),
3) Depth (to the end of tracts),
4) Infection, and
5) Perfusion.
The assessment can be made on wounds of any part of the body and regardless of whether the patient has diabetes or not. Each assessment is graded on a two (optimal) to zero (most severe) point scale using objective, easily recognizable findings for each point on the scale (Table 1).
Long Beach Wound Scores of 7.5 to 10 points classify the wound as Healthy, 3.5 to 7 points as Problem, and 0 to 3 points as End- Stage. The scoring system has inter observer reliability of 0.81 [1]. Serial wound scoring quantifies wound progression providing an objective method for measuring Minimal Clinical Important Difference. Each wound category based on the initial evaluation (i.e. before any in-hospital management of nearly 100 patients) had an outcome accuracy of 75.3% [2].
Utilizing Wound Types to Guide Management
Healthy Wounds Healthy type wounds (LBWS 7.5-10 points) typically heal with basic and inexpensive wound dressing agents. The treatment should be focused on protecting the wound site with offloading, immobilization, and serial debridements of hyperkeratotic callus around the wound margins as well as fibrotic tissues and biofilms in the wound base. Hyperkeratotic callus, which has a propensity to recur especially in diabetic wounds, interferes with wound contraction and epithelialization around the wound margins. An even more serious concern is moisture developing between the undersurface of the callus and the skin around the wound. This fosters bacterial proliferation, which leads to localized sepsis and worsening of the wound. The moist, white callus appears to interfere with the mechanisms of wound contraction and epithelialization. Sharp debridement of biofilms and fibrotic tissues typically with scalpel or curette accomplishes in a few minutes what days or weeks of enzymatic debriding agents or autologous debridements (using frequent moist gauze dressing changes) try to achieve. However, sharp debridements compliment the latter two interventions to improve the wound as quickly as possible.
When epithelialization is not observed after six to eight weeks of standard wound care, negative pressure wound therapy, biologic skin substitutes, split thickness skin grafts or combinations should be considered. For the threatened skin graft, hyperbaric oxygen (HBO) treatments can be an adjunct when the wound site is ischemic based on the clinical evaluation or hypoxia confirmed with transcutaneous oxygen measurements (TCOMs). If juxta- wound TCOMs exceed 200 mmHg with a HBO exposure, there is almost a 90 percent likelihood of healing regardless of TCOM measurements in room air [3].
Problem Wounds For wounds in the Problem category (LBWS 3.5-7 points), the elimination of the “Troublesome Triads” (TT), namely deformity, deep infection, and ischemia/hypoxia, are essential for optimizing outcomes [1,4]. Over 90 percent of Problem wounds were found to have at least one of three TT components in a prospective series with 62 patients hospitalized for DFUs [4]. Deformity should be managed with callus debridement, offloading, and surgical interventions such as tenotomy, ostectomy and/or ostectomy to mitigate the mechanical pressure on the wound site [5]. When sensation, strength, balance, proprioception or combinations are impaired due to neuropathy, deformity can compound loading and/or shearing stresses on the wound and interfere with healing.
Deep infection is the second of the TT reasons for non-healing of the Problem Wound. It requires management with surgical debridement in addition to collaboration with infectious disease specialists for appropriate antibiotic selections. Often the infections in the diabetic foot are due to multiple drug resistant organisms. Antibiotic selection can be further challenging due to comorbidities. For example, impaired renal function requires precise dosing and careful monitoring usually in collaboration with clinical pharmacists. Rarely are deep infections resolved with antibiotics alone. To manage the deep infection adequately, not only is the removable of infected bone necessary, but debridement of surrounding tissue bursa and scar need to be done to optimize the wound environment. These supporting tissues are likely infected, also. The essentially avascular scar tissue is a relative barrier for antibiotic delivery and leukocyte entry into the wound.
Ischemia-Hypoxia is the third TT factor of the Problem Wound type. Minimum juxta-wound transcutaneous oxygen tensions of 30-40 mmHg are necessary for wound healing and infection control [6]. Anti-coagulants, revascularizations, hyperbaric oxygen or combinations are indicated in patients with the ischemia-hypoxia TT component of Problem wounds. Adequate perfusion and tissue oxygenation are necessary to ensure limb salvage [7].
With appropriate management of the three TT confounding factors, we observed that 83.3% of Problem Wounds healed in a prospective series of 85 patients [2]. Outliers to healing in this series included comorbidities such as vasculitis, uncontrollable deformities even with optimal protective footwear, pervasive diabetic neuropathic pain, and new vascular occlusive events. Identification of the TT and early interventions are essential to achieve good outcomes for the Problem Wound category.
End-Stage for the End-Stage wound (LBWS of 0-3 points); the likelihood of healing of the wound is low. Especially when revascularization is not an option for the patient due to existing comorbidities or ischemia is not adequately resolved. Occasionally a combination of anticoagulant therapy and hyperbaric oxygen treatment in conjunction with the revascularization is sufficient to achieve healing in the End-stage Wound. If perfusion is improved enough with these measures, it will be reflected in the LBWS and, consequently quantify the original End-stage Wound as a Problem Wound type. If ischemia-hypoxia is not resolved, amputation at the level of adequate perfusion is indicated for functional restoration and quality of life for the patient [8]. Major (mid foot and proximal) amputation, auto amputation (if the affected area is small such as a toe) or comfort care should be considered according to the patient’s biological (as contrasted to chronological) age, comorbidities and goals.
The Transition Zone Wound Type
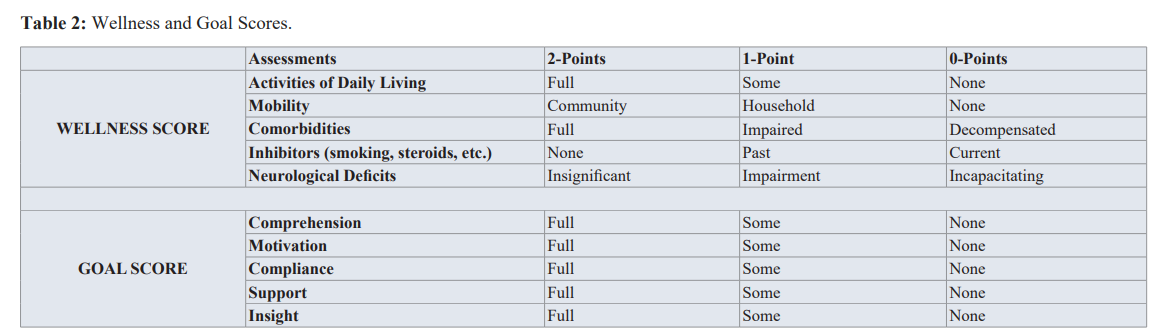
It takes an “act of faith” to believe that wounds with a LBWS of 3½-points (i.e. Problem) always heal while a wound with a score of 3-points (i.e. End-stage) invariably requires a major amputation. Since some Problem Wounds fail and some End-stage Wounds avoid major amputations, decision making for attempting to salvage versus immediate major amputation requires additional information. To resolve this dilemma LBWSs in an intermediate zone between Problem and End-Stage (2.5 to 4 points), are sub categorized as Transition Wounds. Decision making in the Transition Zone between attempting limb salvage or amputation is aided by knowing and objectifying the patient’s health status and goals. Care providers can quantitatively assess those factors using our Wellness and Goal Scores to help make appropriate management decisions (Table 2) [1,2]. If Wellness or Goal Scores are greater than 4-points, attempt to avoid a major amputation is justified for the transitional wound.
Discussion
Many wound scoring systems have been proposed to help clinicians make treatment decisions for patients with diabetic foot ulcerations. The Wound, Ischemia, and Foot Infection (Wi-Fi) score from the Society for Vascular Surgery evaluates wounds with critical limb ischemia into four stages based on the wound extent, the perfusion level and the presence and severity of infection [9]. The statistical correlation between the limb amputation rate and the Wi-Fi wound scores was shown in a retrospective case series with 201 patients to be 0% in stages 1-2 and 8% in stage 3. Sixty-four percent of the stage 4 wounds led to major limb amputation [10]. Obviously, the Wi-Fi focus is on the peripheral artery disease patient rather than the diabetic foot ulcer. With its multiple assessment permutations, a copy of the system with it is over 1000 permutations would seem to be required by the evaluator in order to consider all the grading choices. Yet, the data it presents regarding the amputation risk in wounds is helpful in making decisions about amputations in the presence of wound ischemia.
Perfusion, Extent, Depth, Infection and Sensation (PEDIS) Score is a system that assesses diabetic foot wounds based upon the vascular status, extent of the wound, the presence of infection and peripheral neuropathy. Chuan et al. retrospectively reviewed 364 patients with DFUs according to the PEDIS system. PEDIS scores greater than 7 were 82% specific for the non-healing ulcer, need for amputation, or death at 6 months [11]. The team reported PEDIS system’s sensitivity at 93% and specificity at 82% for calculating negative outcomes for diabetic foot ulcerations. Although notable for its high sensitivity and specificity, it should be noted that this wound score includes the level of intact sensation in the assessment. The presence of peripheral neuropathy is a risk factor for the formation of DFUs, but is not a reason diabetic wounds fail to heal. In fact, a patient’s lack of sensitivity to pain optimizes management by allowing dressing changes, wound debridements, suturing and even tenotomies and partial toe amputations to be done without the need for analgesia.
In the Site, Ischemia, Neuropathy, Bacteria infection, Area and Depth (SINBAD) wound classification system, six assessments are graded using whole numbers from 0-to-1 point [12]. Grades range from the best being 0 (no problem) to 6 (being the worst). Validity is suggested in this scoring system with the authors reporting there is a failure to heal if the point total is greater than three are. As in the PEDIS system, neuropathy is one of the assessments. Like the PEDIS system, the SINBAD system is non-intuitive with the higher the 0-to-6 score, the worse the outcomes.
A reliability study comparing the Wi-Fi, PEDIS, and SINBAD scoring systems, showed excellent inter observer reliability, but poor intra-observer reliability [13]. The authors explained the discrepancy by using averaging techniques and observers judging wounds at different stages of healing. These three systems deserve credit for providing objective criteria for grading wound severity, which can facilitate determining Minimal Clinical Important Differences and Comparative Effective Research, but they do not provide user-friendly grading systems nor algorithms for evaluation and management.
Three other frequently used DFU need to be mentioned because of their widespread use. These are the Wagner system, the Infectious Diseases Society of American Clinical Practice Guideline for the Diagnosis and Treatment of Diabetic Foot Infections (IDSA) and the University of Texas Health Science Center San Antonio
Diabetic Wound Classification (UTSA) [14-16]. The Wagner system provides treatment algorithms, but only uses a single wound observation for making all decisions for the algorithm selected for management. The IDSA system is limited to only the evaluation and treatment of the infection aspects of the diabetic foot wound. The UTSA uses only present or absent criteria for depth of wound and for a combination of ischemia and infection. None has reliability or validity studies although the UTSA system showed poorer outcomes with deep wounds coupled with ischemia and infection [17]. These three DFU grading systems do not facilitate measuring Minimal Clinical Important Difference for wound healing nor enable comparison of interventions for assessing Clinical Effectiveness Research.
When the above information is considered, it substantiates the use of our algorithm for the evaluation and management of DFUs. In addition, it is also applicable for other wound causes and at locations other than the foot. By integrating the LBWS into an algorithm, wound evaluation and management become objective, quantifiable and predictable in addition to being logical (high 0-to- 10 scores have better outcomes) and easy to use with objective findings to grade each of the five assessments on 0-to-2 scales. Our algorithm approach using tangible numbers to grade wounds makes it possible to measure progress, Effectiveness Research and quantify Minimal Clinical Important Difference.
Conclusions
Our algorithm based on the LBWS provides a logical approach for decision making for evaluation and management of DFUs as well as other types of wounds. Established scoring systems have not unified their wound scoring into a cohesive management algorithm as we have done. Use of our algorithm prevents delays in initiating appropriate interventions and facilitates cost effectiveness by detailing the wound characteristics that need interventions at the time of the initial evaluation. Our system makes it possible to quantify progress (or deterioration) by using a 0-to10 wound scoring system. The LBWS measures improvement as scores improve. If the wound does not improve or deterioration is observed, it is quantified and justifies a change in management. Finally, our LBWS enables Comparative Effectiveness Research by making it possible to compare outcomes of treatment interventions for wounds with similar LBWSs and quantify Minimal Clinically Important Difference as wounds change with management.
References
- Strauss MB, Moon H, Busch JA, et Reliability Assessment of an Innovative Wound Score. Wounds. 2016; 28: 206-213.
- Strauss MB, Moon H, La S, et al. Clinical Applications and Validation of an Innovative Wound Wounds. 2018; 30: 154-159.
- Moon H, Strauss MB, La SS, et The validity of transcutaneous oxygen measurements in predicting healing of diabetic foot ulcers. Undersea Hyperb Med. 2016; 43: 641- 648.
- Strauss MB, Moon H, La S, et The incidence of confounding factors in patients with diabetes mellitus hospitalized for diabetic foot ulcers. Wounds. 2016; 28: 287-294.
- Strauss MB. Surgical treatment of problem foot wounds in patients with Clin Orthop Relat Res. 2005; 439: 91-96.
- Hunt TK, Pai MP. The effect of varying ambient oxygen tensions on wound metabolism and collagen synthesis. Surg Gynecol 1972; 135: 561-567.
- Kabra A, Suresh KR, Vivekanand V, et Outcomes of angiosome and non-angiosome targeted revascularization in critical lower limb ischemia. J Vasc Surg. 2013; 57: 44-49.
- Kinlay Management of Critical Limb Ischemia. Circ Cardiovasc Interv. 2016; 9: e001946.
- Mills JL, Conte MS, Armstrong DG, et The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: risk stratification based on wound, ischemia, and foot infection (Wi-Fi). J Vasc Surg. 2014; 59: 220-234.
- Zhan LX, Branco BC, Armstrong DG, et The Society for Vascular Surgery lower extremity threatened limb classification system based on Wound, Ischemia, and foot Infection (Wi-Fi) correlates with risk of major amputation and time to wound healing. J Vasc Surg. 2015; 61: 939-944.
- Chuan F, Tang K, Jiang P, et al. Reliability and Validity of the Perfusion, Extent, Depth, Infection and Sensation (PEDIS) Classification System and Score in Patients with Diabetic Foot PLOS ONE. 2015; 10: e0124739.
- Ince P, Zulfigarli G, Lutae JK, et al. Use of the SINBAD classification system in comparing outcome of foot ulcer management on three continents. Diabetes Care. 2008; 31: 964-967.
- Forsythe RO, Ozdemir BA, Chemla ES, et al. Inter observer Reliability of Three Validated Scoring Systems in the Assessment of Diabetic Foot Int. J Low Extrem Wounds. 2016; 15: 213-219.
- Wagner, FWW The dysvascular foot: A system of diagnosis and treatment. Foot Ankle Intl. 1981; 2: 64-122.
- Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot Clin Infect Dis. 2012; 54: 132-172.
- Lavery LA, Armstrong DG, Harkness LB. Classification of diabetic foot J Foot Ankle Surg. 1996; 35: 528-531.
- Armstrong DG, Lavery LA, Harkness LB. Validation if a diabetic wound classification The combination of depth, infection and ischemia to risk of amputation. Diabetes Care. 1998; 21: 855-859.