Anaesthesia for thyroidectomy at the Niamey National Hospital
Author'(s):Chaibou MS1*, Labo Madougou R1, Daddy H1, Dodo Siddo MN2, Nanzir Sanoussi M1, Gagara M1,James Didier L3, Younssa H3, Sanoussi S3 and Sani R3
1Department of Anesthesiology, Niamey National Hospital (HNN),Niger.
2Department of Medicine, Niamey National Hospital (HNN), Niger.
3Department of Surgery, Niamey National Hospital (HNN), Niger
*Correspondence:
CHAIBOU Maman Sani, Department of Anesthesiology, Niamey National Hospital, Tel: 0022794777766.
Received: 11 November 2021; Accepted: 22 December 2021
Citation: Chaibou MS, Labo Madougou R, Daddy H, et al. Anaesthesia for thyroidectomy at the Niamey National Hospital . Anesth Pain Res. 2021; 5(2): 1-4.
Abstract
Objectives: To describe anesthesiological management of thyroidectomy at Niamey National Hospital.
Method: This was a prospective study conducted from, January 1st to June 30th 2018. Were been included all patients who underwent an anesthesiological procedure with a complete record for a thyroidectomy at the National Hospital of Niamey. The following variables were studied: age, sex, comorbidity, ASA class Status, Mallampati class, operative indication, anesthesia technique, anesthetic protocol, intraoperative anesthetic incidents and accidents, duration of surgery, duration of anesthesia, duration in resuscitation room, postoperative follow-up. The data were analyzed by the software Word 2013 and Epi Info 3.5.4.
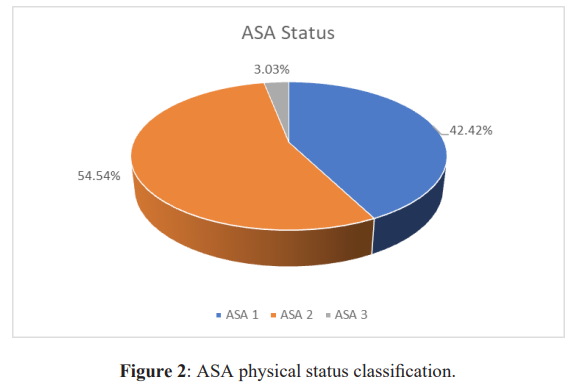
Results: The series included 33 patients, 28 women (84.84%) and 5 men (15.16%). The average age was 42 years ± 8.3 with extremes of 24 years to 78 years. The operative indications were dominated by multinodular goiter with 42.42%; the Mallampati 1 class was predominant with 51.51% of cases; the ASA 2 class status represent 54.54% of cases; difficult intubation involved 18.20% of patients. General anesthesia was the only technique used in all our patients. Hypotension was the major perioperative incident for 6 of 7 patients involved. Total thyroidectomy was the most performed procedure in 72.72% of patients. Postoperative analgesia was provided by paracetamol, NSAIDs, tramadol and nefopam with a predominance of paracetamol+tramadol combination in 66.60% of cases. The average duration of the surgery was 80 minutes with extremes of 36 minutes to 120 minutes. The operative follow-ups were simple in 97% of cases with a zero-mortality rate. The average hospital stay was 7 days with extremes of 3 days to 14 days.
Conclusion: Thyroidectomy under general anesthesia is a well-understood procedure today in our context, but it is necessary to train teams in the practice of locoregional anesthesia adapted to our environment.
Keywords
Introduction
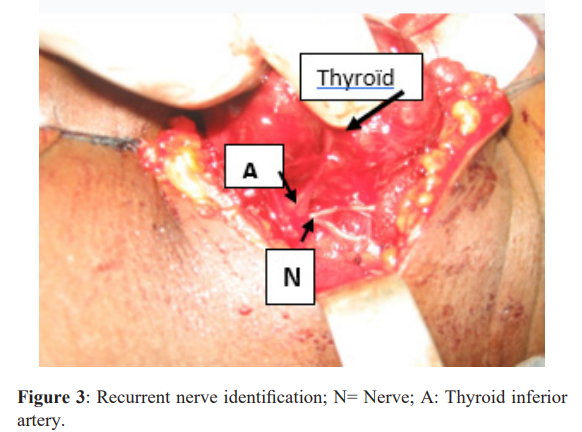
Thyroid surgery was recognized for its difficulty with a significant mortality rate. The prognosis has improved markedly, benefiting from innovations in anesthesia, anti-infective prophylaxis and hemostasis. Thyroid surgery is very meticulous and requires the practitioner to be extremely rigorous, especially in achieving hemostasis, but also in preserving the lower laryngeal nerve and parathyroid glands. General anesthesia with orotracheal intubation is the most appropriate and widely used technique. Locoregional anesthesia is an alternative used in some countries. No study has looked at anesthesia for thyroidectomy in our context, hence the interest of our study which will allow us to make an inventory of the anesthesiological management of this condition [1-6].
Method
This is a prospective and descriptive study carried out from January 1st to June 30th , 2018; or six months. Were been included all patients who had undergone an anesthesiological procedure for a scheduled thyroidectomy at the Niamey National Hospital. The following variables were studied: age, sex, comorbidity, ASA class, Mallampati class, surgical indication, anesthesia procedure, anesthetic protocol, intraoperative anesthetic incidents and accidents, duration of surgery, duration of anesthesia, duration in the intensive care unit, postoperative follow-up. The data were analyzed by Word 2013 and Epi info3.5.4 software.
Results
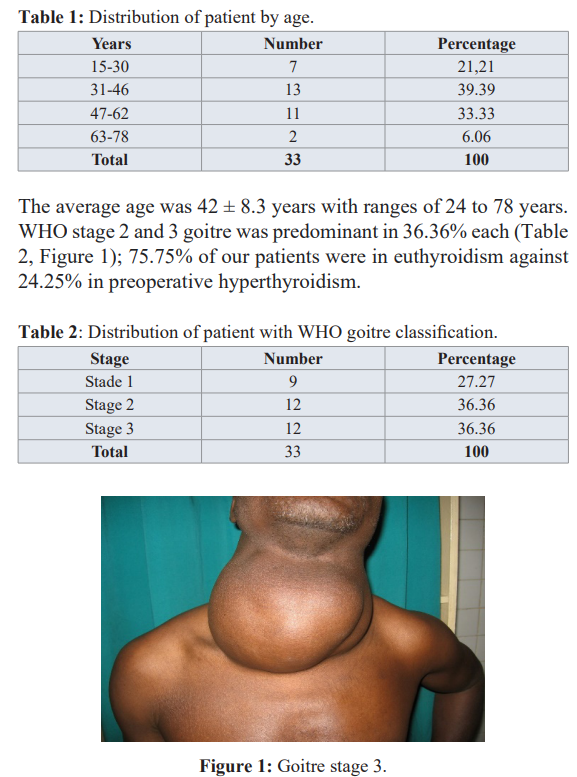
During the study period, we collected 33 patients operated for thyroidectomy out of 529 patients; 6.23%. The female sex predominated with 84.84% (sex ratio of 0.17). The 31-46 years group represented 39.39% (Table 1).
General anesthesia was the only technique used, the thiopental + sufentanyl + atracurium anesthetic protocol was used at induction in 51.51%, 57.57% and 66.66%, respectively; propofol was used in 27.27%. Halothane was used for maintenance 90.33% of the time. Difficult intubation affected 18.20% of patients, there was a correlation between the Mallampati class and difficult intubation. Adverse events occurred in 21.21% of patients dominated by low blood pressure, bradycardia and hemorrhage. Total thyroidectomy was performed in 72.72%, subtotal thyroidectomy and lobo- isthmectomy in respectively 12.12% each. Surgery average duration of 80 minutes with extremes of 36 to 120 minutes. Anesthesia lasted between 1 hour and 2 hours in 51.5% of patients (mean duration 2.4 hours with extremes of 1 hour to 4.83 hours). Postoperative analgesia was multimodal (paracetamol + tramadol) in 66.60% of patients, (paracetamol + nefopam) in 18.2% of patients. The duration of stay for patients admitted to intensive care was 24 hours. The postoperative outcome was favorable in 97% of patients, only one case of compressive hematoma was recorded. The death rate was zero. The average length of hospitalization was 7 days with extremes of 3 to 14 days.
Discussion
We collected 33 cases in 6 months represented 6.2% of the operated patients. Touré A. et al. and Koumaré S. et al. reported an average of 3.13% and 6.2% respectively. But lower than those found by Illé S. et al 8.51% [7-9]. The average age was 42 years± 8.3. This result is similar to those obtained by Koumaré S. et al. and Sani R et al., who found an average age of 41.99 years ± 13.5 years and 41 years respectively. Ablaye L. et al. and Ouzzad O. et al. who were respectively 37.25 years old, 38.82 years old and 46 years old [8,10-12].
In our study, we have a female predominance with 84.84%, other series reported a female predominance [9-12]. Mallampati class 1 accounted for 51.51%; 33.33% were Mallampati 2. This classification is important because it makes it possible to predict difficult intubation and therefore what to do before surgery. A severely enlarged thyroid can affect intubation [13].
`In our study the ASA II class was predominant with 54.54%. This result is different from those found by Koumaré S. et al. [8]. General anesthesia with orotracheal intubation was the only anesthetic technique used although locoregional anesthesia could be used for this type of surgery, as reported by some authors Nandrianina R. et al., Musa AA. et al. and Shukla VK. et al. reported the practice of regional or local anesthesia in thyroidectomy. These two techniques according to these authors constitute alternatives because they are simple, fast and less expensive while shortening the duration of hospitalization [14-16]. The drugs used were thiopental, propofol, fentanyl and halothane, this is related to the fact that these are the anesthetic drugs available as found in other series. [17]
We recorded 21.21% of intraoperative adverse events with a predominance of arterial hypotension followed by bradycardia and hemorrhage. In Koumaré's series, bleeding occurred in 12% of patients [8]. Total thyroidectomy was the most performed surgical procedure followed by subtotal thyroidectomy and lobo- isthmectomy in 72.7%, 12.2% and 12.1% of cases, respectively. Our results are different from those of Sani R. et al., Illé S. et al. and Touré A. which found a predominance of lobo-isthmectomy in respectively 49.67%, 40.25% and 66.14% of cases. [7, 9.10]. All of our patients had benefited from a postoperative multimodal analgesic protocol, in accordance with the postoperative pain management regimen in our hospitals [17]. In our series, the length of stay of patients admitted to intensive care was 24 hours, indeed all patients with Basedow’s disease or enormous thyroids are systematically admitted to intensive care during the first 24 hours. The postoperative evolution was simple in 97% of cases, only one case of compressive hematoma was recorded. Our result is similar to those of Illé S. et al., Koumaré S. et al. and Touré A et al. which found respectively 96.18%, 94.17 and 93.5% of cases. this is linked to the precaution taken by the teams in the preparation and the precautions to avoid lesions of the recurrent nerve. (Figure 3) Our result is superior to that found by Sani R. et al. with 86.7% [6.8.9]. The mortality rate was zero in our series, which makes thyroid surgery one of the safest surgeries in our hospital as general surgery mortality was 1% in our country. [18]
Conclusion
Thyroid disease can occur at any age, but it seems to be the preserve of young adults with a clear predominance of women. Anesthesia for thyroidectomy in our context is done exclusively under general anesthesia and seems to have been well mastered despite everything, efforts must be made for the development of locoregional anesthesia very well suited to our context.
References
1.Bougnères P, Chanson P, Young J. Prévalence des maladies thyroïdiennes. Médecine Thérapeutique Endocrinologie Reproduction. 2000; 2: 526-534.
2.Dubose J, Barnett R, Ragstedt J. Honest and sensible surgeon. Current surgery. 2004; 61: 213-219.
3.Kania R, Vérrilaud B, le Clerc N, et al. Thyroïdectomies par cervicotomie. Encyclopédie médico-chirurgicale (EMC), Techniques chirurgicales-tête cou. 2004; 46: 1-15.
4.Conessa CI, Sissoko B, Faye M. Les complications de la chirurgie de la thyroïde à l’hôpital principal de Dakar à propos de 155 interventions. Méd Afr Noire. 2000; 43: 157-160.
5.Koumaré AK, Sissoko F, Ongoiba N et al. Goitres bénins en chirurgie au Mali (à propos de 815 cas) e-mémoires de l’académie nationale de chirurgie. 2002; 1: 1-6.
6.Sani R, Adehossi E, Ada A, et al. Evaluation du traitement chirurgical des hyperthyroïdies, étude prospective sur 37 cas opérés à l’hôpital national de Niamey. Méd Afr Noire. 2006; 53: 581-586.
7.Touré A, Diallo AT, Camara LM, et al. La chirurgie thyroïdienne : expérience du service de chirurgie générale du CHU Ignace Deen de Conakry. Mali Med. 2006; 21: 23-27.
8.Koumaré S, Soumaré L, Sacko L, et al. Prise en charge des goitres en chirurgie A du CHU point G. Mali Medical. 2016; 31: 3-17.
9.Illé S, James Didier L, Timi N, et al. Résultats de 5 ans de thyroïdectomie au service d’ORL et Chirurgie Cervico- Faciale de l’Hôpital National de Niamey. European Scientific Journal. 2017; 7: 31.
10.Sani R, Hassanaly A, James Didier L, et al. Les thyroïdectomies à l’Hôpital National de Niamey (HNN). Résultats d’une étude prospective de 105 cas pendant 12 mois. Annales de l’Université Abdou Moumouni. 2009; 121-124.
11.Ablaye L, Ndiaye N, Lèye YM, et al. Les thyroïdectomies au centre hospitalier national de Pikine-Dakar (CHNP) : indications et résultats chez 417 patients. Révue Afr de Méd Interne. 2016; 3: 36-40.
12.Ouzzad O, Zoubir M. Anesthésie pour la chirurgie du goitre: étude rétrospective portant sur une durée de 2 ans à l’Hôpital Militaire Avicenne de Marrakech. Journal marocain des sciences médicales. 2016; 113: 58-63.
13.Lebuffe G, Caiazzo R, Andrieu G. Anesthésie dans la chirurgie de la glande thyroïde Ency med. Chir Anesth-Réa. 2015; 36; 9.
14.Nandrianina R, Herimanalalaniaina A, Mahamad R, et al. Thyroidectomies pratiquées sous anesthésie locale au centre hospitalier universitaire d’Antananarivo. Pan Afr Med J. 2005; 21: 278.
15.Musa AA, Lasisi OA, Fatungase OM, et al. General and regional anaesthesia for thyroidectomy in rural/semi urban Nigerian centres. East Afr Med J. 2009; 86: 287-290.
16.Shukla VK, Narayan S, Chauhan VS, et al. Thyroid surgery under local anaesthesia: an alternative to general anaesthesia. Indian J Surg. 2005; 67: 316-319.
17.Chaibou MS., Daddy H., Hassane ML et al. Anesthesia practice in low-income country. A multicentric study. Int J Clin Anesthesiol 9(1): 1110.
18.Biccard BM, Madiba TE, Kluyts H-L, et al. Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. Lancet. 2018; 391: 1589-1598.