Assessment of the Inter-Individual Concordance of ASA PS Score versus ABCK: A Survey Carried Out Among Anaesthetists of Kinshasa City
Author'(s): Bula-Bula IM1,2*, Mvuama N3, Bwaka A4, Lokomba V5, Kimpanga P6, Lepira F7 and Kilembe M1
1Department of Anaesthesia and Resuscitation, University of Kinshasa Teaching Hospital, Congo.
2Reference General Hospital of N’Djili, Congo.
3Maternal and Child Health Centre Barumbu, Congo.
4WHO Intercountry-Support Team Office for West Africa,Ouagadougou, Congo.
5Department of Gynaecology-Obstetrics, University of Kinshasa Teaching Hospital, Congo.
6Kinshasa School of Public Health, University of Kinshasa, Congo.
7Department of Internal Medicine, University of Kinshasa Teaching Hospital, Congo.
*Correspondence:
Bula-Bula IM, Department of Anaesthesia and Resuscitation,University of Kinshasa Teaching Hospital, Congo, E-mail:drmebula@gmail.com.
Received: 14 November 2018; Accepted: 20 December 2018
Citation: Bula-Bula IM, Mvuama N, Bwaka A, et al. Assessment of the Inter-Individual Concordance of ASA PS Score versus ABCK: A Survey Carried Out Among Anaesthetists of Kinshasa City. Anesth Pain Res. 2018; 2(2): 1-5.
Abstract
Background: The ASA PS is a score which evaluates the physical state of a preoperative patient. It is largely used throughout the world. However, it is subjective and presents inconsistencies among anaesthetists.
Because of these disagreements, some medical institutions established their own methods of evaluation. One of them is the Altered general status - Breathing - Circulation – K scores (ABCK). The question which this study raised was to know whether, in terms of inter individual consistency, the ABCK, a new score which has presented an excellent agreement with the ASA PS, could not be more effective than the ASA PS?
Methods: A survey of the ASA PS and ABCK classes of ten hypothetical cases from the Aronson study (2) and the reasons for their choice, was carried out among anesthetists in Kinshasa. The sampling was of the exhaustive type. The data were collected using a self-administered questionnaire technique.
Results: This study showed that the agreement between the two scores varied from a weak agreement (kappa de Cohen = 0.2; p = 0.001) to a moderate agreement (Kappa de Cohen = 0.59; p = 0.001).
Furthermore, the ABCK had an interindividual interclass variance weaker than the ASA PS (IC 95 %; P< 0.005).
Conclusion: The ABCK score proves to be much more objective than the ASA PS. Indeed, it has an interclass variability weaker than that of the ASA PS. And because of its good agreement with the ASA PS, it could be used as an alternative or complement to it.
Keywords
Introduction
The assessment of the physical state is part of the pre-operative examination of the patient. ASA PS is an essentially subjective evaluation of operative risks, independent of the age of the patient and the type of surgery [1]. Only, it has a weak interindividual concordance [2,3].
In order to solve the problem of the subjectivity and the weak interindividual concordance of the ASA PS, several classifications have been proposed [4-7]. But none of these classifications has the same level of use as the ASA PS [8].
Most recently, a new score, the ABCK was proposed as a way to solve the problem of subjectivity and poor concordance of ASA PS [9]. It is based on the rating of three elements: the alteration of the general state of the patient, the damage of the respiratory system and the damage of the cardio-circulatory system.
The aim of this study was to find out whether in addition to the good agreement with ASA PS, the ABCK score would show a lower interindividual variability than the 'ASA PS. This would then imply that ABCK score presents less subjectivity than ASA PS. The objective of this study was to show that; compared to the ASA PS the ABCK has a better interindividual agreement.
Methods
The study is a survey on the ASA PS and ABCK classes of ten hypothetical cases from the Aronson study [2] and the reasons for their choice. The new score is represented in Table I below.
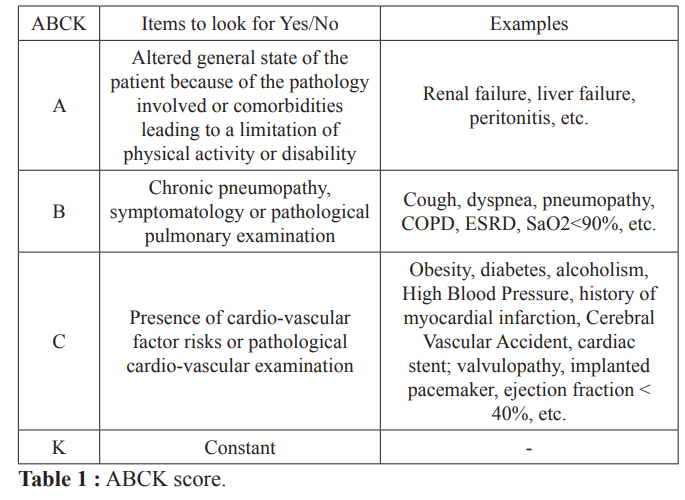
Each item on the look is marked one if the answer is yes and zero if it is no. Then, we add up the marks and, to the sum found, in order to match the classes ABCK with those of the ASA, we add the number one which is the value of the constant K. As for the ASA, the moribund patient is considered ABCK 5 and the decerebrated, ABCK 6.
The study was conducted with anesthesia-resuscitation physicians and fellows in anesthesia working in different hospitals in Kinshasa. The sampling was of the exhaustive type.
Data were collected using a self-administered questionnaire technique with half-opened questions that were given to the participants in hard copy format.
Ten hypothetical cases listed below were submitted to the participants for classification according to the ASA PS score and the new score, the ABCK. These ten hypothetical cases were taken from the study by Aronson et al. [11].
Their responses, collected two weeks after the questionnaire was submitted to them, were analyzed with a view to drawing conclusions. Several visits to hospitals were necessary to get some respondents to complete the data collection sheets. The pre-test was conducted at the Hopital de l’Amitié Sino-Congolaise (HASC).
The results of this study were presented as averages and percentage. The comparison of the ABCK score with ASA PS was performed using the Kappa’ Cohen test.
The Epi Info software program, version 3.5.3 enabled the statistical analysis of the results. The exact Fisher test and the Chi-square test were used for the analyzes. For the interpretation of the results, a p-value <0.05 was considered statistically significant.
Below are the ten cases of the survey.
Scenario 1
A 19 years old patient, victim of a road traffic accident 10 hours ago who requires a fixation of a fracture of tibia. Unconscious at the scene of the accident; in the emergency room, he responded to the pain with incomprehensible sounds. He now obeys the command and opens his eyes when he is spoken to. Computerized tomography showed significant frontal contusion but no evidence of intracranial hypertension.
Scenario 2
66 years old is admitted for an earlier resection of rectal cancer. He smoked 2 to 3 packs of cigarettes a day for 50 years and had a productive cough for 15 years. He has received antibiotics twice in the past 6 months for a lung infection. Now his sputum is clear. He has shortness of breath when climbing the stairs but easily plays golf twice a week.
Physical examination: clear lungs
No signs or symptoms of cardiovascular disease; irregular drug intake; hemoglobin = 13.6 g / l; blood urea and normal electrolyte; chest x-ray shows a slight hyperinflation of the pulmonary fields; electrocardiogram (ECG) normal; forced expiratory volume in 1 second (FEV1), 2.3l and forced vital capacity (CVF), 3.5l.
Scenario 3
72 years old is admitted for an elective repair of the aneurysm of the abdominal aorta. History of myocardial infarction 2 years ago; stable angor for the last 5 years, treated with Nifedipine and sublingual nitroglycerin (once a week).
Physical examination: stronger systolic murmur on the aorta area; blood pressure, 170/80 mm Hg. ECG, Q waves in the II, III and AVF, with slight left ventricular hypertrophy; chest x-ray and normal blood cell counts; urea, 30 mg / dl; creatinine, 2.0 mg / dl; the electrolyte levels in normal values.
Scenario 4
69 years old, 80 kg, is admitted for transurethral prostatectomy. Smoked throughout his adult life; decreased exercise tolerance, shortness of breath on walking on inclined ground, symptomatic relief with ipratropium (Atrovent) and beclomethasone used for prophylactic treatment (Beconase); small amount daily clear sputum.
Physical examination: slight intercostal retraction and expiratory rales dispersed in the lungs. FEV1 = 2.21; FVC = 3.9L.Blood cell count, blood urea and electrolyte levels, ECG and normal chest x-ray.
Scenario 5
65 years with oesophageal carcinoma. Regimen limited to liquids. Expected for esophagectomy (upper abdominal incision and thoracotomy on right side). History of angina for 1 year. No symptoms after treatment with atenolol; but when he became unable to swallow tablets, symptoms of angina during exercise came back. ECG, chest x-ray, liver tests, blood urea and electrolytes are normal; hemoglobin = 10.1 g / dl with microcytic photo; FEV1 and FVC, 90% of the predicted value for age and weight (before the onset of dysphagia)
Scenario 6
42 years old man, previously healthy, with subarachnoid hemorrhage 36 hours ago; continues to complain of severe headaches, but conscience is not compromised. The neurological examination shows a paralysis of the right oculomotor nerve. Cerebral angiography identifies an anterior aneurysm of the communicating artery without any sign of arterial spasm. He is been scheduled for a craniotomy for correction of the aneurysm.
Scenario 7
57 years old with Type I (insulin-dependent) diabetes is admitted for right knee arthroplasty due to osteoarthritis related to an injury 20 years ago; no significant arthritis in other joints; on the other hand, healthy with a normal blood glucose around 130 mg / dl. History and physical examination: nothing special; no cardiovascular abnormalities or ophthalmic; creatinine at 2.0 mg / dl; results of all other routine laboratory routine tests were normal.
Scenario 8
23-year-old woman (60 kg) is admitted for arthroscopy of the left knee; smoked a pack of cigarettes a day for 3 years. No important health history except for a left knee injury 2 months ago. Stress tolerance before the accident, running 3 miles 3 times a week. Physical examination: nothing special; human chorionic gonadotrophin, negative. (note: mile = 1609 meters).
Scenario 9
25 years old woman (65 and 80 kg) Pregnancy 1, Parity 0 is allowed in active labor, dilated to 5 cm; she is seeking for an epidural analgesia. The development of pregnancy is usual; hematocrit = 38%; hemoglobin = 12.4 g / dl; normal electrolyte level. History and physical examination, normal term pregnancy.
Scenario 10
26 years is admitted for bilateral tubal reanastomosis; history and physical examination banal; excellent health; small mouth, small chin and limitation of opening of the mouth; history of trauma of the face, no bone lesions but temporomandibular joint dysfunction; has never received general anesthesia.
Results
A total of 65 respondents, including 19 physicians in anesthesia and resuscitation and 46 fellow anesthetists working in public, private and university teaching hospitals were enrolled in this study. The male sex was predominant with a sex ratio of 1.37. The average age was 37 ± 14 years. The majority of respondents (50.8%) were in public hospitals.
In terms of their qualification, fellows in anesthesia were the most numerous and taking into account the seniority of all qualifications, the majority of respondents (40%), had less than four years of professional experience.
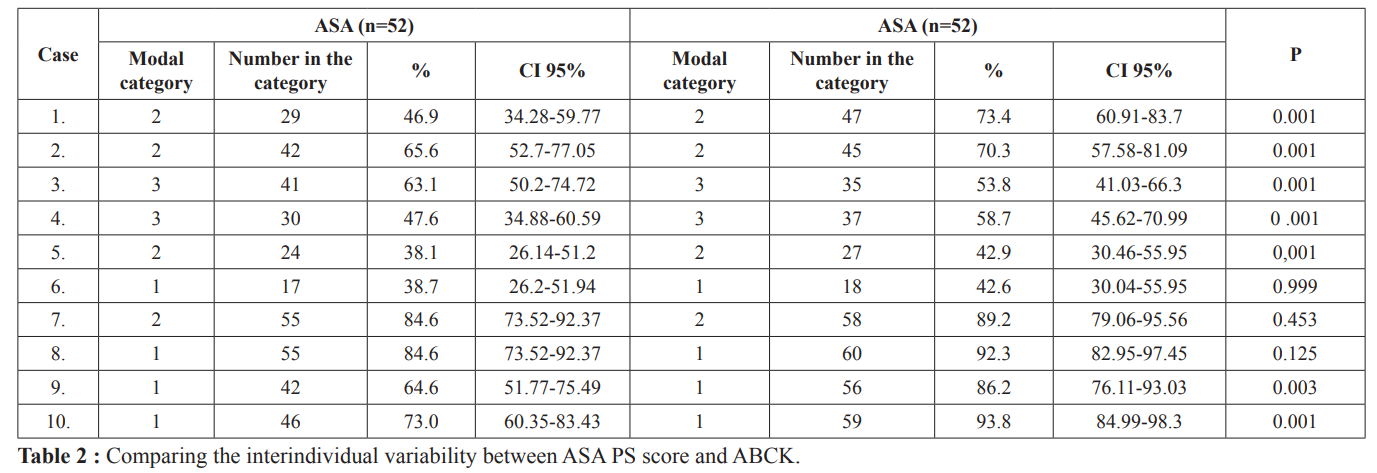
The percentage of respondents who placed the ten hypothetical cases in the modal category was larger in the ABCK than in the ASA PS. This, statistically significant for cases 1, 9 and 10 (p<0.05).
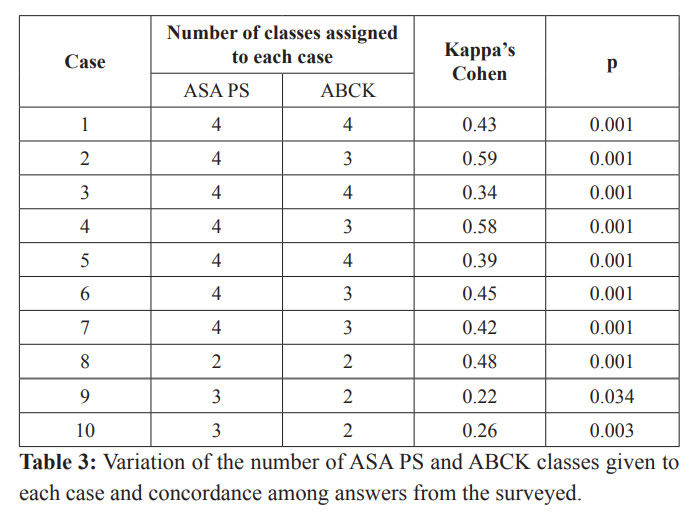
Apart from cases 1, 3, 5 and 8 where the class range was the same in both classifications, the number of classes assigned to each case was larger in ASA PS than in ABCK. In addition, the agreement between the two scores for the ten hypothetical cases ranged from a weak agreement (k = 0.26) to a moderate agreement (0.59).
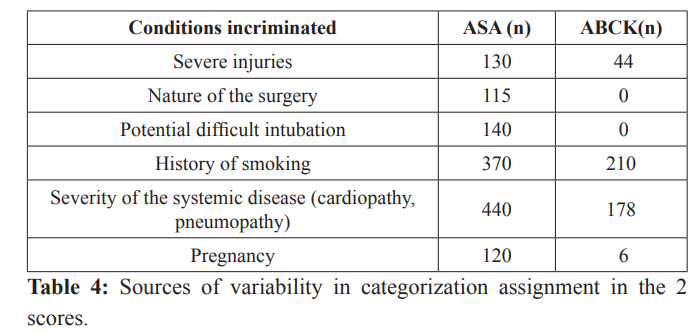
The severity of the systemic condition and the history of smoking were the main sources of variability in class assignment in both scores.
Discussion
In this study, a concordance ranging from low agreement (Kappa’ Cohen = 0.22) to moderate agreement (Kappa’ Cohen = 0.58) was found between the ASA PS and ABCK scores. In an earlier study [9], an excellent agreement (Kappa’ Cohen = 0.86) was found between the two scores. The much lower agreement found in this study was probably related to the choice of the variables. Indeed, this study relied on hypothetical cases from the Aronson study [11] which was designed to demonstrate the variability of ASA PS. It is these deliberately chosen variables that could explain this weak link. Moreover, the respondents were not given the opportunity to ask questions of understanding in order to be able to find the appropriate class of the case.
Sabour (2015), criticizing an article by Sankar (2014) who found a weak concordance in the assignment of ASA PS classes [12], states that "The value of Kappa’ Cohen depends, among other things, on the number of categories of responses: the fewer the categories, the higher the K “[13]. In this study, the number of categories varied from 4 to 16. This high number of categories could also explain the low concordance rates found in this study.
The ASA PS score is known to exhibit great inter-individual variability [3,14-16]. In this study, compared to the ABCK, the percentage of respondents who placed the ten hypothetical cases in the modal category was larger in the ABCK than in the ASA PS. This was statistically significant for cases 1, 9 and 10.
There were no statistically significant cases of higher choice for the modal class in ASA PS than in ABCK. This shows that the ABCK has a lower interindividual variability than the ASA PS.
Reliability in the assignment of ASA PS and ABCK scores was not demonstrated in the 10 cases. As in the Aronson study [11], none of these 10 cases had a full agreement in both scores. The classes assigned to the different cases varied between 1 and 4. It was only in one case, the eighth, that the range of variations was limited to 2 classes: 1 and 2. This applied for both ASA PS score and ABCK score. But, on the whole, apart from cases 1, 3, 5 and 8, the number of classes assigned to each case was greater in ASA PS than in ABCK.
The scattering elements found in this study were also found to be explanatory factors for interindividual variability in other studies, including those of Aronson et al [11] and Aplin et al. [16]. Smoking, a risk factor and not pathology per se, the severity of the systemic disease (heart disease, pulmonary disease, etc.) and serious injuries were cited as factors explaining this variability in the two classifications. On the other hand, the nature of the surgery, the potential difficult intubation and the pregnancy, for almost all the respondents, were the sources of variability found only in the ASA PS.
In a singular way, the severity of the systemic disorder was the predominant explanatory element of variability in class assignment, mainly in ASA PS. One of the weaknesses of the ASA PS would be to seek to classify systemic conditions in terms of mild, moderate or severe. And this classification does not respond to all systemic conditions.
ASA PS may be easier to use in cases of high blood pressure or asthma, because these conditions can be classified in terms of mild, moderate or severe. However, conditions such as diabetes, heart failure, kidney or liver failure, etc do not apply themselves to this classification. Categorizing them in terms of their severity exposes them to a significant risk of subjectivity. This may be perhaps the reason why the nature of the surgery, the potentially difficult intubation, the history of smoking, and other conditions that do not respond to the classification as mild, moderate and severe, were the main sources of variability.
The high number of factors explaining the variability found in the ASA PS is likely to explain this greater variability. This high number could in turn be explained by the dimensions of the concepts used to define its classes. Indeed, the more a concept has a large extension the more its understanding is weak. The extension of the terms used to define ASA PS classes (systemic condition, degree of disability, etc.) could explain their poor understanding, and thus the greater variability of this score.
Finally, even if the ASA PS classification would be decried by several authors for its subjectivity [1,11], it finds a slight interest. This insofar as, by this same subjectivity, it expresses to a certain extent the own assessment of the anesthetist [15].
Conclusion
This study made it possible to show that the ABCK score showed an interindividual. Concordance greater than that of ASA PS. And because of its simplicity and its concordance. With ASA PS, the ABCK could be used as an alternative, especially in countries with limited. Qualified service providers. A study on a different population for its external validity will be desirable before its widespread use.
References
1.Daabiss M. American Society of Anaesthesiologists physical status classification. Indian J Anaesth. 2011; 55: 111-115.
2.Fitz-Henry J. The ASA classification and peri-operative risk.Ann R Coll Surg Engl. 2011; 93: 185-187.
3.Cuvillon P, Nouvellon E, Marret E, et al. American Society of Anesthesiologists’ physical status system: a multicentre Francophone study to analyse reasons for classification disagreement. Eur J Anaesthesiol. 2011; 28: 742-747.
4.Nouvellon E, Ripart J. Faut-il encore croire au score ASA ? Lepraticien en anesthésie. 2007; 11: 212-216.
5.Glance LG, Lustik SJ, Hannan EL, et al. The surgical mortality probability model: derivation and validation of a simple risk prediction rule for noncardiac surgery. Ann Surg. 2012; 255: 696-702.
6.Dalton JE, Kurz A, Turan A, et al. Development and validation of a risk quantification index for 30-day postoperative mortality and morbidity in noncardiac surgical patients. Anesthesiology. 2011; 114: 1336-1344.
7.Scott S, Lund JN, Gold S, et al. An evaluation of POSSUM and P-POSSUM scoring in predicting post-operative mortality in a level 1 critical care setting. BMC Anesthesiol. 2014; 14: 104.
8.Atilio B, Holly M. Use of a modifier reduces inconsistency in the American Society of Anesthesiologists physical status classification in parturients. Anesth Analg. 2006; 102: 1231-1233.
9.Bula-Bula IM, Kabuni P, Kimbien J, et al. Assessment of the preoperative health status base on ASA PS versus ABCK: A descriptive Study. Int J Clin Anesthesiol. 2016; 4 : 1060-1064.
10.https//www.asahq.org/resources/clinical-information/asa-physical-status-classification-system
11.Aronson WL, MCAulife MS, Miller K. Variability in American Society of Anesthesiologists physical status classification scale. AANA Journal. 2003; 71: 265-274.
12.Sankar A, Johnson SR, Beattie WS, et al. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth. 2014; 113: 424-432.
13.Sabour S. Reliability of the ASA physical status scale in clinical practice: methodological issues. BJA. 2015; 114: 162-163.
14.Aplin S, Baines D, De Lima J. Use of the ASA physical status grading system in pediatric practice. Pediatr Anaesth. 2007; 17: 216-222.
15.Zampieri FG. Categorical measurements of subjectiveness: is there still a role for the ASA classification? Rev. bras. ter. Intensiva. 2015; 27.
16.Hurwitz EE, Simon M, Vinta SR, et al. Using examples best when classifying ASA. Clinical Anesthesiology. 2016.