Black Esophagus: About A Case with Review of the Literature
Author'(s): Alioune Badara FALL1*, Abdou NIASS2, Evelyne Sourou Aminata KOUKOUI1, Birane NGOM1, Ahmadou GAYE1 and Abdoulaye NDIAYE2
1Department of Gastroenterology, Hospital Cheikhoul Khadim, Diourbel, Senegal.
2Department of Surgery, Hospital Cheikhoul Khadim, Diourbel, Senegal.
*Correspondence:
Alioune Badara FALL, Department of Gastroenterology, Hospital Cheikhoul Khadim, Diourbel, Senegal.
Received: 16 Feb 2024 Accepted: 25 Mar 2024 Published: 03 Apr 2024
Citation: Alioune Badara F, Abdou N, Evelyne Sourou Aminata K, et al. Black Esophagus: About A Case with Review of the Literature. Gastroint Hepatol Dig Dis. 2024; 7(1): 1-3.
Abstract
Introduction: Black esophagus or acute esophageal necrosis is a disease of poorly understood etiology. Our goal is to carry out a literature review on this condition by reporting a case treated in our structure.
Observation: A 69-year-old female patient, hypertensive, who underwent concomitant radiochemotherapy followed by abdominoperineal amputation for lower rectum adenocarcinoma with sphincter involvement, suddenly presented on the 15th postoperative day with moderate abundance hematemesis. Upper gastrointestinal endoscoy revealed extensive necrosis of the middle and lower thirds of the esophagus without gastric or duodenal involvement. There was no caustic ingestion or esophagogastric reflux. The cervical-thoracic-abdominal CT scan showed no transmural necrosis. She was fasted for 7 days and received parenteral nutrition, double dose proton pump inhibitor and blood transfusion. The evolution was favorable with almost total disappearance of the necrosis on upper GI endoscopy control one week later.
Conclusion: Black esophagus or acute esophageal necrosis is a rare condition, most often discovered in postoperative context. Proton pump inhibitors and gut rest remain effective means in their management.
Keywords
Introduction
Acute esophageal necrosis or black esophagus is characterized by circumferential necrosis without an interval of healthy mucosa in the esophagus [1,2]. It is a rare condition arising from several etiological factors [3,4]. Its occurrence on fragile ground and the risk of esophageal perforation makes it very serious. The evolution remains favorable under well-conducted medical treatment [1,5]. We report the case of an elderly patient, operated on for cancer of the lower rectum and presenting upper digestive bleeding related to a black esophagus having evolved well under medical treatment by PPI and parenteral nutrition.
Observation
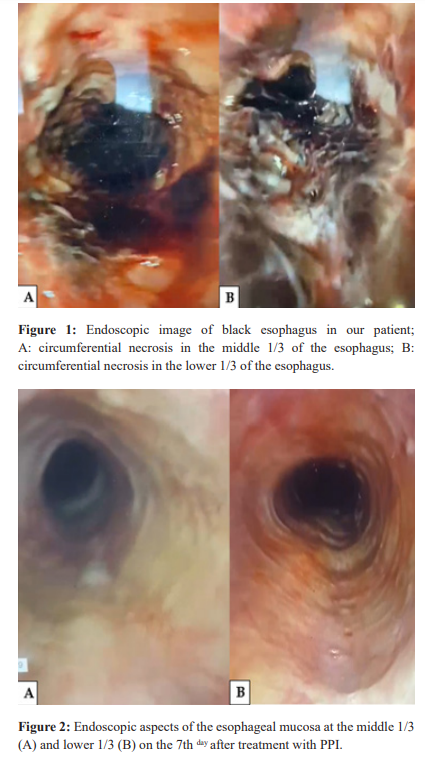
It was a 69-year-old hypertensive patient followed. She was referred by the medical oncology department of the Cheikh Ahmadoul Khadim hospital in TOUBA (Diourbel-Senegal) for surgical management of a tubular adenocarcinoma of the lower rectum infiltrating the internal sphincter with pulmonary metastases having progressed well under concurrent radiochemotherapy with disappearance of metastases and reduction in tumor size. She underwent an abdominoperineal amputation followed by a 5-day stay in intensive care for oligo-anuria which had progressed well under vascular filling. The patient was bedridden and obese with a body mass index or BMI of 31.5 kg/m2). On the 15th postoperative day, she suddenly presented repetitive hematemesis of moderate abundance motivating emergency upper GI endoscopy. It revealed a range of circumferential necrosis of the esophageal mucosa in the middle and lower 1/3 with a clear stop at the esophagogastric junction without gastric or duodenal involvement (figure 1). Biology showed normochromic microcytic anemia at 7.8 g/d. There was no caustic ingestion during the interview nor a history of gastroesophageal reflux disease (GERD). She was fasted and put on parenteral nutrition associated with blood transfusion and treatment with proton pump inhibitor (PPI) with omeprazole at a dose of 40 mg morning and evening. The evolution was marked by a disappearance of hematemesis. The control upper GI endoscopy performed 7 days after the start of treatment showed disappearance of the esophageal necrosis (figure 2). Herpes and cytomegalovirus serologies were not performed. In addition, she had a simple malaria attack and parietal suppuration with multi- resistant Escherichia Coli treated respectively with antimalarial and imipenem. The follow-up was simple, allowing discharge on the 35th postoperative day.
Discussion
The prevalence of black esophagus is estimated at 0.2%. As noted in our patient, it most often affects subjects over the age of 60 [6]. In descending order, several factors are implicated in its etiopathogenesis. These are the post-operative period, immunosuppression, acute or chronic renal failure, cirrhosis, hypertension, neoplasia and diabetes [1,7,8]. In our patient, the prolonged stay in intensive care linked to hypovolemia-induced renal insufficiency, rectal neoplasia, advanced age, and arterial hypertension could be the main factors favoring the occurrence of black esophagus. Pathologically, acute esophageal necrosis is multifactorial. Indeed, there is fragile esophageal mucosa (role of the pathological terrain) associated with tissue ischemia and impaired gastric acid reflux barrier mechanisms [2,9]. Bedrest in our obese patient could promote acid reflux causing peptic esophagitis that probably evolved into acute necrosis of the esophagus. The location in the middle and lower 1/3 of the esophagus is an element in favor of the hypothesis of a possible GERD with peptic esophagitis. Thus, Yasuda et al plead on the ischemic origin of esophageal necrosis in view of the typical topographic characteristics and the presence of gastroesophageal reflux, which is found in 40% of cases [10]. Indeed, the brutal nature, the frequently involvement of the lower 1/3 of the esophagus (less vascularized), the absence of gastric lesions (as noted in our patient) and the frequent association with duodenal lesions confirm this ischemic hypothesis found in 75% of observations [2,3,5,11].
Other factors are also mentioned in the literature such as viral infections with cytomegalovirus and herpes simplex virus; bacterial infections with Klebsiella pneumoniae and fungal infections with Candida [4,7,12]. EGD allows the diagnosis. It must be carefully driven to avoid iatrogenic perforation. It shows a circumferential black mucosa, sitting with predilection at the lower 1/3 (97% of cases) and stopping abruptly at the Z line [2]. Biopsies are recommended but not mandatory. Their interest lies in suspected bacterial, viral, or fungal infections or secondary infections and in immunocompromised patients [4,11]. Pathological examination finds severe mucosal and submucosal necrosis, but necrosis is rarely transmural (unlike caustic causes) [5]. An inflammatory infiltrate and partial destruction of the adjacent muscularis may occasionally be observed. These biopsies also enable ruling out certain differential diagnoses such as primary melanoma of the esophagus, esophageal melanosis and Acanthosis nigricans [10,13,14]. Caustic ingestion should be sought [1,13,14]. Fasting and proton pump inhibitors are the basic treatment for black esophagus [1,7]. Indeed, the evolution is usually favorable under PPI. However, esophageal perforation is the main acute complication to be feared. It is rapidly life- threatening by promoting septic mediastinitis [14,15]. As noted in our patient, the complete resolution of the lesions is often early, between the 7th and 12th day [15]. Nevertheless, there is a risk of esophageal stenosis, found in 10.2% of cases, which can appear from the 1st to the 4th week of evolution [1,11]. Hence the interest of performing of upper GI endoscopy remotely (1 to 2 months after the acute episode).
References
- Mohamed Hichem Loghmari, Wafa Ben Mansour, Arwa Guediche, et al. The black esophagus: about a case. Medical 2018; 96: 229-232.
- Gurvits GE, Shapsis A, Lau N, et Acute esophageal necrosis: a rare syndrome. J Gastroenterol. 2007; 42: 29-38.
- Sako A, Kitayama J, Inoue T, et al. Black esophagus- cause? 2005; 54: 192-227.
- Ben Soussan E, Savoye G, Hochain P, et al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc. 2002; 56: 213-217.
- Grudell AB, Mueller PS, Viggiano TR. Black esophagus: report of six cases and review of the literature, 1963-2003. Say 2006; 19: 105-110.
- Shafa S, Sharma N, Keshishian J, et The Black Esophagus: A Rare but Deadly Disease. ACG Case Reports Journal. 2016; 3: 88-91.
- Trappe R, Pohl H, Forberger A, Schindler R, et al. Acute esophageal necrosis (black esophagus) in the renal transplant recipient: manifestation of primary cytomegalovirus Transpl Infect Dis. 2007; 9: 42-45.
- Arthur A. Keresztesi, Gabriela Asofie, Laura Chinezu, et al. Acute esophageal necrosis (“black esophagus”): Case series in forensicbautopsies casuistry. Rom J Leg Med. 2016; 24: 87-91.
- Gurvits GE, Shapsis A, Lau N, et acute esophageal necrosis: a rare syndrome. J Gastroenterol. 2007; 42: 29-38.
- Yasuda H, Yamada M, Endo Y, et Acute necrotizing esophagitis: role of nonsteroidal anti-inflammatory drugs. J Gastroenterol. 2006; 41: 193-197.
- Kim YH, Choi Black esophagus with concomitant candidiasis developed after diabetic ketoacidosis. World J Gastroenterol. 2007; 13: 5662-5663.
- Liu YH, Lin YS, Chen HJ, et al. Klebsiella pneumoniae deep neck infection with acute necrotizing esophagitis. South Med 2009; 102: 219.
- Raven RW, Dawson Malignant melanoma of the esophagus. Br J Surg. 1964; 51: 551-555.
- Kozlowski LM, Nigra Esophageal acanthosis nigricans in association with adenocarcinoma from an unknown primary site. J Am Acad Dermatol. 1992; 26: 348-351.
- Augusto F, Fernandes V, Cremers MI, et al. Acute necrotizing esophagitis: a large retrospective case series. Endoscopy. 2004; 36: 411-415.