Can the Use of Cardiology Medical Record to Deliver Educational Intervention Improve Care? On Behalf of TAPP Program: Thinking Approach Towards Physician Support in Patient Management
Author(s): Langer A*, Tan M, Goldin L and Langer G
Canadian Heart Research Centre, Toronto, Canada.
*Correspondence:
Anatoly Langer, Canadian Heart Research Centre, Toronto,Canada.
Received: 11 Aug 2023; Accepted: 20 Sep 2023; Published: 27 Sep 2023
Citation: Langer A, Tan M, Goldin L, et al. Can the Use of Cardiology Medical Record to Deliver Educational Intervention Improve Care? On Behalf of TAPP Program: Thinking Approach Towards Physician Support in Patient Management. Cardiol Vasc Res. 2023; 7(4): 1-4.
Abstract
Background: Despite clear and concise practice guidelines, strategies for lowering LDL-C are often poorly adopted in clinical practice, and many patients fail to reach guideline-recommended levels despite physician education and quality improvement programs. We studied whether physician focussed, guideline-based practice level educational intervention can improve lipid lowering management.
Methods: Cardiologists or internal medicine specialists from the province of Ontario, Canada who were using a cardiology specific EMR (CEREBRUM, WELL Health Technologies Corporation) were invited to participate. Practice level data of patients with history of acute coronary syndromes (ACS) and lipid profile were studied. Physicians were alerted when patients in their practice were not treated according to recommendations. The primary endpoint was proportion of patients achieving the recommended LDL-C level of below 1.8 mmol/L.
Results: Of the invited 378 specialists, 178 agreed to participate and shared their practice involving 7,683 ACS patients who were 70.4 ± 10.3 years of age and 27.2% were women. Overall, 57.7% of patients had LDL-C < 1.8 mmol/L at the start of the program (1.84 ± 0.87 mmol/L) and 63.0% (1.75 ± 0.79 mmol/L) at the end of the program (p<0.0001). With respect to the lipid lowering therapy, statin therapy was used in 52.9% of patients at the start of the program and increased to 72.1% at the end (p<0.0001). The use of ezetimibe increased from 12.6% to 19.0% (p<0.0001) and the use of PCSK9i from 1.2% to 2.4% (p<0.0001).
Conclusion: The results indicate the feasibility of using EMR as a platform to deliver educational intervention and overcoming treatment inertia and improving LDL-C lowering.
Keywords
Introduction
Low-density lipoprotein cholesterol (LDL-C) is a well- established risk factor for cardiovascular (CV) disease and there is considerable evidence that lowering LDL-C reduces the risk of both cardiovascular events and mortality in patients with CV disease [1]. Despite clear and concise guidelines [2], strategies for lowering LDL-C are often poorly adopted in clinical practice, and many patients fail to reach guideline-recommended levels despite physician education and quality improvement programs [3]. This care gap or treatment inertia, defined as the difference between evidence-based approach and real life, results in a significant burden [4] of atherosclerotic cardiovascular disease (ASCVD). Current guidelines recommend the use of high intensity statins as the first step [2,5,6]. Although statins remain the mainstay of dyslipidemia management, attainment of the recommended low density (LDL-C) or non-high density (non-HDL-C) lipoprotein cholesterol goals can be difficult even with the use of the highest doses of high intensity statin therapy [7,8]. To address this challenge, clinical practice guidelines (CPG) now recommend addition of either ezetimibe or proprotein convertase subtilisin/ kexin type 9 inhibitor (PCSK9i) or both based on clinical trial evidence [9-11].
Recent experience [12-14] indicates absence of cholesterol panel results on the chart in approximately 50% of patients, use of guideline recommended lipid-lowering therapy in only a minority of patients and lowering of the LDL-C or non-HDL-C to recommended levels in approximately a third of patients with ASCVD. We have recently studied the use of electronic medical records (EMR) in primary care physicians and found that the educational intervention did not significantly improve care, in part because of the lack of universal access to the cholesterol panel results and concern about additional lipid lowering therapy [12]. We, therefore, studied whether cardiology focussed, guideline- based patient level educational intervention can improve lipid lowering management,
Methods
Cardiologists or internal medicine specialists from the province of Ontario, Canada who were using a cardiology specific EMR (CEREBRUM, WELL Health Technologies Corporation) were invited to participate. Invitations to participate were sent to 378 Ontario specialists registered as full-time or part-time users of the CEREBRUM EMR. The program was supported by Amgen Canada and coordinated by the Canadian Heart Research Centre, an academic research and education physician organization. Only patients with history of acute coronary syndromes (ACS as in OHIP codes 410, 412, and 413) and lipid profile data available in the last 24 months. The program start was December 2021 and ended on December 31st, 2022. It should be noted that the start of the program was timed closely in relation to the release of the Canadian Cardiovascular Society Recommendations on the Management of Dyslipidemia [5].
Data cuts were provided to the Canadian Heart Research Centre quarterly limited to practice level cholesterol panel and lipid lowering medications data and no patient level data or any personal health or identifying data was disclosed or shared.
Participating physicians were asked to share their practice level data (dashboard) to ascertain the care gap based on CPG recommended LDL-C levels and management [5]. Physicians were alerted regarding groups of patients in their practice that were not treated according to recommendations [5] and were asked to review recommendations and optimize therapy as they thought fit. The primary endpoint was proportion of patients achieving the recommended LDL-C level of below 1.8 mmol/L and the secondary endpoint was proportion of patients treated with statin, ezetimibe and PCSK9i as per recommendations [5].
Statistical Analysis
Continuous data are shown as means with standard deviation and categorical data as frequencies and percentages. Group compari- sons were made using the chi squared test or McNemar’s test and t-test or Kruskal-Wallis test for discrete and continuous variables, respectively, where appropriate. A value of p <0.05 was considered significant for all tests. All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC).
Results
Of the invited specialists, 178 agreed to participate and shared their practice involving 7,683 patients meeting the inclusion criteria and who were 70.4 ± 10.3 years of age and 27.2% were women. The LDL-C at the start of the program was 1.84 ± 0.87 mmol and the end of the program 1.75 ± 0.79 mmol/L (p<0.0001). Overall, 57.7% of patients had LDL-C < 1.8 mmol/L at the start of the program and 63.0% at the end of the program (p<0.0001). Conversely, the LDL-C above 2.2 mmol/L was recorded in 23.3% at the start and in 18.6% mmol/L (p<0.0001) at the end of the program.
Among 4,838 patients with LDL-C < 1.8 mmol/L at the end of the program, 75.4% already had LDL-C <1.8 mmol/L at the start (Figure 1) as compared to 24.6% who started out with LDL-C >1.8 mmol/L (p=0.0002). Conversely, among 2,845 patients with LDL-C > 1.8 mmol/L at the end of the program 72.4% had LDL-C >1.8 mmol/L (Figure 1) at the start while 27.6% started out with LDL-C < 1.8 mmol/L (p<0.0001).
With respect to the lipid lowering therapy, statin therapy was used in 52.9% of patients at the start of the program and increased to 72.1% at the end (p<0.0001). The use of ezetimibe increased from 12.6% to 19.0% (p<0.0001) and the use of PCSK9i from 1.2% to 2.4% (p<0.0001). In 1789 patients with LDL-C >2.2 mmol at the program start, the LDL-C remained above 2.2 mmol/L in 51.3%, lowered to 1.8-2.2 mmol/L in 19.2% and was reduced to below 1.8 mmol/L in 29.6%. Comparison of lipid lowering therapy in those patients with LDL>2.2 mmol/L vs those with LDL-C <1.8 mmol/L revealed use of any statin in 55.3% vs 75.6% (p<0.0001), any ezetimibe in 26.7% vs 26.5% (p=0.92) and any PCSK9i in 4.5% vs 7.0% (p=0.041).
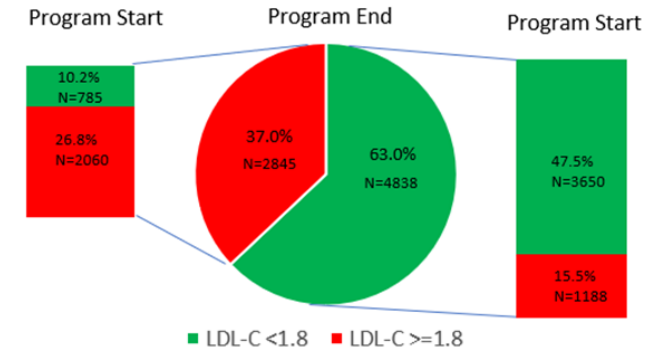
Figure 1: Change in primary endpoint (proportion of patients achieving LDL-C <1.8 mmol/L) at program end overall (middle chart) broken down by their LDL at program start (left side those who ended up with LDL >1.8 mmol/L and the right side for those who achieved LDL < 1.8 mmol/L at the end.
In 785 patients (10.2% of all patients) the LDL-C was below 1.8 mmol/L (1.52 ± 0.24) at the program start and >1.8 mmol/L (2.19 ± 0.55) at the end of the program, i.e. these patients experienced an increase in their LDL-C level during the program period of observation. Of these patients, 53.9% were on statin at the program start and 76.4% at the program end (p<0.0001). Similarly, the use of ezetimibe and PCSK9i increased from 10.1 to 16.9% (p<0.0001) and from 0.3% to 1.8% (p=0.0005) respectively.
Discussion
In patients with established cardiovascular disease, LDL-C lowering is one of the safest and most efficient ways of lowering the risk of future cardiovascular events including cardiovascular and total mortality and myocardial infarction and stroke. Lowering of LDL-C by 1 mmol/L results in 20% reduction in cardiovascular mortality and 12% reduction in total mortality as well as 22% reduction in other cardiovascular events over five years [1]. We have previously documented the benefit of an algorithmic approach towards LDL-C lowering with the addition of ezetimibe [13] and more recently with the patient level improvement in the care gap based on CPG recommendations [14].
The results of our program indicate presence of a significant treatment inertia in high-risk patients as part of the secondary prevention in the hands of the cardiovascular specialists; specifically less than 60% of patients with ACS had LDL-C at or below the recommended LDL-C level. This indicates that over 40% of ACS patients in the hands of Canadian specialists experienced treatment inertia. As opportunities for treatment optimization were highlighted, there was a significant improvement in patient management as reflected by the significant increase in the primary endpoint. This improvement in the care gap was a result of a significant increase in the use of all three recommended lipid lowering therapies. Given the relative novelty of the Canadian Guidelines [5] at the time of the program start, it is possible that a more robust improvement may have been observed.
Canadian Guidelines [5] recommend the use of PCSK9i in patients with LDL-C > 2.2 mmol/L. Our assessment of management in these patients disclosed minimal use of PCSK9i (<10%) and the use of ezetimibe in only a quarter of these patients despite a clear and strong recommendation for using these additional lipid lowering therapies and particularly PCSK9i in patients post-ACS and with LDL-C above 2.2 mmol/L [5].
We and others [16-18] have demonstrated that treatment inertia is associated with unfavorable outcome. The etiology of treatment inertia is multi-factorial including several patient and physician associated factors [15]. The worsening of dyslipidemia in 785 patients despite an increase in all of the recommended therapies is likely related to patient factors such as non-compliance. On the other hand, 37% of all patients with LDL-C above recommended level and despite educational intervention is likely related, at least in part, to treatment inertia in the hands of the specialists.
In summary, significant care gap exists among cardiovascular specialists with respect to lipid lowering management in patients with prior ACS history. Programs designed to overcome treatment inertia are needed to improve LDL-C control and achieve reduction in cardiovascular morbidity and mortality of high-risk patients.
Limitations
This study provided descriptive analysis of practice level data from participating physicians who were not chosen randomly and this selection bias limits generalizability of our findings. Furthermore, the use of a single EMR platform may have contributed not only to the bias in physician selection but also in the care gap findings with respect to LDL-C reporting and its management. Finally, a lack of a control arm makes it difficult to ascertain if the changes in treatment were triggered by the intervention or may have occurred anyway.
Conclusion
The results of TAPP program indicate the feasibility of delivering an educational intervention using the EMR as a platform and as a result overcoming treatment inertia in many patients and improving LDL-C lowering.
Acknowledgements
Study was supported by Amgen Canada. The funding organization did not participate in study design, data collection or data analysis.
Disclosures
Dr. Anatoly Langer received implementation science research grants in the therapeutic area of dyslipidemia from Amgen, Novartis, and AstraZeneca. Dr. Anatoly Langer is not a member of an advisory board or a speaker bureau for any pharmaceutical company.
References
- Baigent C, Keech A, Kearney PM, et al. Cholesterol Treatment Trialists (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005; 366: 1267-1278.
- Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidemias: lipid modification to reduce cardiovascular risk. European Heart Journal. 2019; 00: 1-78.
- Langer A, Tan M, Goodman SG, et al. GOAL Canada: Physician Education and Support Can Improve Patient Management. Can J Cardiol Open. 2020; 2: 49-54.
- Grima DT, Leiter LA, Goodman SG, et al. How many cardiovascular events can be prevented with optimal management of high-risk Canadians?. Can J Cardiol. 2008; 24: 363-368.
- Pearson GJ, Thanassoulis G, Anderson TA, et al. 2021 CCS Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can J Cardiol. 2021; 37: 1129-1150.
- Scott M Grundy, Neil J Stone, Alison L Bailey, et al. AHA/ ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019; 73: 3168-3209.
- Martineau P, Gaw A, de Teresa E, et al. Effect of individualizing starting doses of a statin according to baseline LDL-cholesterol levels on achieving cholesterol targets: the Achieve Cholesterol Targets Fast with Atorvastatin Stratified Titration (ACTFAST) Atherosclerosis. 2007; 191: 135-146.
- Wiviott SD, Cannon CP, Morrow DA, et al. Can Low- Density Lipoprotein Be Too Low? The Safety and Efficacy of Achieving Very Low Low-Density Lipoprotein With Intensive Statin Therapy: A PROVE IT-TIMI 22 Substudy. J Am Coll Cardiol. 2005; 46: 1411-1416.
- Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015; 372: 2387-2397.
- Sabatine MS, Giugliano RP, Keech AC, et Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med. 2017; 376: 1713-1722.
- Schwartz GG, Szarek M, Bhatt DL, et al. The ODYSSEY OUTCOMES Trial: Topline Results. Alirocumab in Patients After Acute Coronary Syndrome. Presented at the American College of Cardiology Annual Scientific Sessions. 2018.
- Langer A, Tan M, Bell A, et Can Physician Education and Support Improve Patient Management. Cardiol Vasc Res. 2020; 4: 1-5.
- Katz PM, Mendelsohn AA, Goodman SG, et al. Use of a Treatment Optimization Algorithm Involving Statin-Ezetimibe Combination Aids in Achievement of Guideline-Based Low- Density Lipoprotein Targets in Patients With Dyslipidemia at High Vascular Risk Guideline-Based Undertaking to Improve Dyslipidemia Management in Canada (GUIDANC). Can J of Cardiol. 2011: 138-145.
- Langer A, Tan M, Goodman SG, et al. Leiter LA GOAL Canada: Physician Education and Support Can Improve Patient Management CJC Open. 2020; 2: 49-54.
- Tsang JLY, Mendelsohn A, Tan M, et Discordance between physicians’ estimation of patient cardiovascular risk and use of evidence-based medical therapy. Am J Cardiol. 2008; 102: 1142-1145.
- Grima DT, Leiter LA, Goodman SG, et al. How Many Cardiovascular Events Can Be Prevented With Optimal Management of High-Risk Canadians?. Can J Cardiol. 2008; 24: 363-368.
- Rogers AM, Ramanath VS, Grzybowski M, et al. The association between guideline-based treatment instructions at the point of discharge and lower 1-year mortality in Medicare patients after acute myocardial infarction: the American College of Cardiology's Guidelines Applied in Practice (GAP) initiative in Michigan. Am Heart J. 2007; 154: 461-469.
- Arnold SV, Spertus JA, Masoudi FA, et Beyond Medication Prescription as Performance Measures. J Am Coll Cardiol. 2013; 62: 1791-1801.