Case Report: Successful Treatment of COVID-19 ARDS with Transcutaneous Vagus Nerve Stimulation
Author'(s): Patrick Nemechek DO1* and Ivan Evlogiev MD2
1Nemechek Autonomic Medicine, Buckeye Arizona.
2MPATH Rahila Angelova, Pernik, Bulgaria.
*Correspondence:
Patrick Nemechek DO, Nemechek Autonomic Medicine, Buckeye Arizona.
Received: 08 October 2021; Accepted: 04 November 2021
Citation: Nemechek P, Evlogiev I. Case Report: Successful Treatment of COVID-19 ARDS with Transcutaneous Vagus Nerve Stimulation. Clin Immunol Res. 2021; 5(2): 1-6.
Abstract
We report two individuals who successfully recovered from COVID-19-induced ARDS after being treated with transcutaneous auricular vagus nerve stimulation (taVNS). In the first case, taVNS was started after eleven hospital days of continual deterioration despite mechanical ventilation along with supportive therapy of steroids, antibiotics, and immunoglobulins. On the twelfth day of hospitalization, taVNS was begun four times daily, resulting in sudden improvement in oxygenation. There was a concomitant reduction of c-reactive protein from 109.6 μg/mL to 10 μg/mL. After nine days of taVNS therapy, the patient's improved respiratory function improved enough that she was able to be extubated. No additional treatments had been added or changed during this time. After twenty-seven days of hospitalization, the patient was discharged to home without supplemental oxygen. The second case involves taVNS therapy in the home setting. After nineteen days of progressive deterioration, the patient's oxygen saturation declined to 90% on room air before taVNS treatment was instituted. After tens days of taVNS treatment three times daily, his oxygen saturation had climbed to 97%, and by day 25 of VNS therapy, the patient felt he was fully recovered.
taVNS is capable of improving regulation of the inflammatory response in other clinical conditions such as autoimmune disorders in humans and septic shock in animal models. We suggest that transcutaneous auricular vagus nerve stimulation is potent enough to improve the clinical course of COVID-19 associated ARDS because of its potential to minimize the clinical deterioration associated with the immunological surge known as the cytokine storm. taVNS is a safe and potentially efficacious treatment for COVID-19 ARDS.
Keywords
Abbreviations
ARDS: Acute Respiratory Distress Syndrome; CAP: Cholinergic Anti-inflammatory Pathway; CRS: Cytokine Release Syndrome; CRP: C-Reactive Protein; IL: Interleukin; TNF: Tumor Necrosis Factor; VNS: Vagus Nerve Stimulation.
Introduction
As the severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2) pandemic continues and thousands of individuals die daily from COVID-19 worldwide, a more effective therapeutic option is essential. A dramatic cytokine storm characterizes infection with SARS-CoV-2 in some patients with COVID-19 [1]. Often referred to as Cytokine Release Syndrome (CRS), this storm is due to the release of high levels of pro-inflammatory cytokines such as interleukin (IL)-1 β, IL-6, tumor necrosis factor (TNF), chemokines by respiratory epithelial, dendritic cells, and macrophages. The surge of pro-inflammatory cytokines has the potential to contribute to the multitude of pathological changes seen in severe COVID-19 patients (Figure 1).
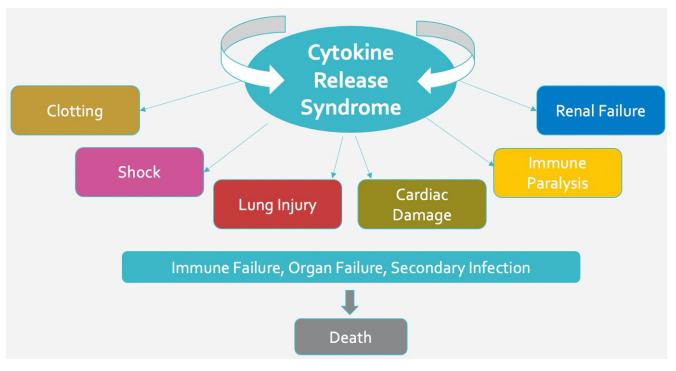
Figure 1: Potential negative impact of cytokine release syndrome.
Several drug therapies are being studied to target the surge of inflammatory cytokine with attention towards non-drug therapeutic strategies targeting inflammatory and immunological processes that may be useful for reducing COVID-19-induced complications and improving patient outcomes (Figure 2) [9,10].
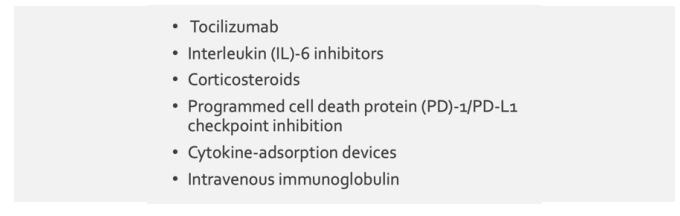
Figure 2: Drugs used to suppress cytokines in COVID-19.
We hypothesize that CRS can be lessened with a subsequent improvement in the patient's clinical outcome by activating the vagal-driven cholinergic anti-inflammatory pathway (CAP). Boezaart et al. published a case report of two individuals with COVID-19 who experienced significant reductions in IL-6 and CRP levels using 60 minutes of taVNS per day. Both individuals had COVID-19 pneumonia and were essentially free of respiratory symptoms by the end of the treatment course (16 and 18 days) with taVNS [11]. Additionally, Staats et al. reported on the clinical improvement in two individuals with SARS-CoV-2 respiratory symptoms [12].
We conducted an uncontrolled trial of taVNS in which hospitalized COVID-19 patients requiring supplemental oxygenation were treated with taVNS four times daily. The treatments with taVNS were well tolerated, and when compared to other hospitalized COVID-19 cohorts, the use of taVNS was associated with decreased mechanical ventilation requirements and low mortality rates [13].
First described by Borovikova and Tracey, the CAP controls cytokine release via afferent vagal signaling into the dorsal vagal complex (DVC) [14,15]. The DVC is responsible for receiving and processing that vagal afferent signaling [14-16]. After the impulse is analyzed by the DVC, efferent impulses via sympathetic (spinal cord) and parasympatheitic (vagus nerve) pathways result in the release of acetylcholine (ACh) secretion at the site of injury that terminates the release of pro-inflammatory cytokines.
Individuals may have suppressed vagus nerve functionality partially reflected in low heart rate variability (HRV). Depressed vagal tone leads to functional impairment of CAP, resulting in excessive cytokine distribution (cytokine storm) followed by tissue injury, pulmonary dysfunction, ARDS, and immune suppression. Suppressed HRV has been associated with the severity of COVID-19. Hospitalized patients whose HRV parameters did not improve required more time to clear the virus and recover clinically [17].
The CAP is a neural reflex capable of decreasing the release of pro-inflammatory cytokines and is modulated by the vagus nerve. Electric neuromodulation of the vagus nerve inhibits TNF synthesis during endotoxemia, ischemia/reperfusion injury, hemorrhagic shock, septic peritonitis, and other excessive cytokine disorder modulation during endotoxemia ischemia/reperfusion injury, hemorrhagic shock, septic peritonitis, and other excessive cytokine disorders [18].
Vagus nerve stimulation (VNS) can play an essential role in managing patients with SARS-CoV-2 infection [18]. The vagus nerve widely innervates multiple organs, especially the lungs and gastrointestinal tract. When the electrical stimulation is applied transcutaneously at the ear (taVNS), afferent fibers are stimulated, thereby activating the central autonomic network and resulting in activation of the efferent fibers of both the right and left vagus nerves as well as sympathetic fibers within the spinal cord and potential activation of the HPA axis [19]. The cumulative effect of taVNS is the improvement of the inflammatory modulation [18]. taVNS therapy is uncomplicated, safe, inexpensive, and treatment might suppress the CRS enough to improve the clinical course in COVID-19 patients requiring hospitalization (Figure 3).
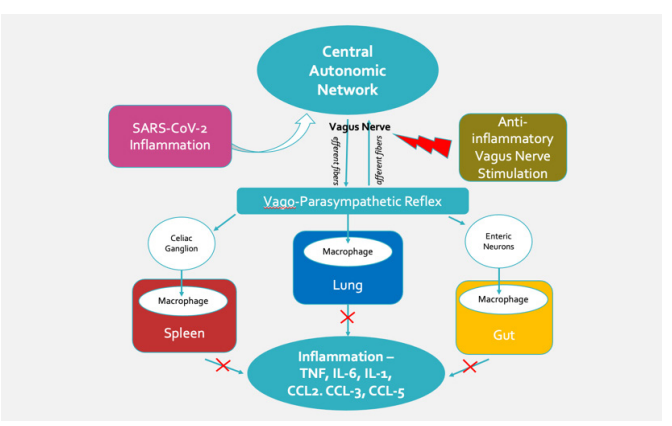
Figure 3: Potential beneficial effect of vagus nerve stimulation in COVID-19 patients. (Modified from Bonaz) [24].
We present two case reports of individuals whose clinical deterioration was reversed with the use of taVNS. The first case is a woman hospitalized with COVID-19 pneumonia and ARDS whose clinical condition had deteriorated to the extent that the managing physician told the patient's family that she had "zero chance of survival." The second case is a gentleman who refused to be taken to the hospital although his respiratory function from SARS-CoV-2 infection was rapidly deteriorating.
Case Report #1
The patient is a 66-year-old Caucasian woman living in Bulgaria. She received her first AstraZeneca vaccinations against SARS- CoV-2 on February 25th. But within one week, she began having symptoms of dry cough, fever, shortness of breath, faintness, fatigue, bedridden, abdominal pain, diffuse muscle and joint pain. On March 7th, she was taken to the emergency room. Her blood pressure was 90/60, pulse rate was 110, spO2 was 80%, and her chest x-ray showed bilateral pulmonary infiltrates. She was hospitalized with a presumptive diagnosis of COVID-19 pneumonia. The following day she tested positive for SARS-CoV-2 (PCR).
The patient's daughter was familiar with publications discussing the potential benefit of taVNS in COVID-19 [13,19-21] and had access to a taVNS device (Nemechek Technologies LLC) used at home on her son with autism as part of an anti-inflammatory treatment regimen [22]. After discussion with her mother's managing physician, the physician agreed to start her on a course of taVNS therapy four times daily which the physician himself would administer. The following is an outline of her clinical course before and after the initiation of taVNS. Data was compiled from the hospital discharge report, family testimony, and photographs of the bedside vital sign monitoring and mechanical ventilator display screens.
Respiratory Function Deteriorates Before the Use of Vagus Nerve Stimulation
The patient's condition continued to deteriorate, and within two more days, she was placed on mechanical ventilation. Despite aggressive medical therapy, her respiratory function declined even further over the following ten days.
By hospital day 12, she required high concentrations of inspired oxygen (FiO2 = 89%) along with high ventilator pressures (PEEP = 5 mmHg) to keep her oxygen saturation level (SaO2) at 92%. (Figure 4). Further increases in the intensity of mechanical ventilation would start to damage her lungs further and only worsen her condition. Because of her steady deterioration despite aggressive medical treatment that her managing physician informed her family that the patient, their mother, had "zero chance of survival".
Clinical and Laboratory Improvements after Starting Vagus Nerve Stimulation
On the 12th day of hospitalization, transcutaneous auricular taVNS (10 Hz, 800 uS with voltage below perceptive threshold) was begun for 5 minutes, four times per day, and was administered by a physician overseeing her care in the critical care unit.
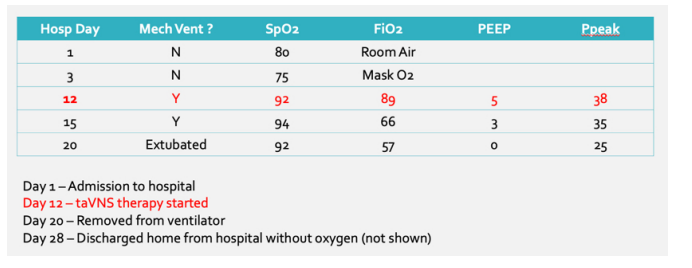
Figure 4: Case #1 - Oxygenation and mechanical ventilation indices.
Within 24 hours of initiating taVNS, the patient's c-reactive protein (CRP) dramatically declined from 109.6 μg/mL to 10.1 μg/ mL. After three days of taVNS, the patients' SpO2 had increased from 92% to 94%, while fiO2 levels declined from 89 to 66%, and PEEP declined from 5 to 3 mmHg. Lung compliance steadily improved, with Ppeak values declining from a high of 38 mmHg down to 25 mmHg at the time of extubation (Image 1). Her chest x-ray findings were improving as well (Figure 5). After eight days of taVNS therapy, she was extubated and placed on a high-flow oxygen mask.
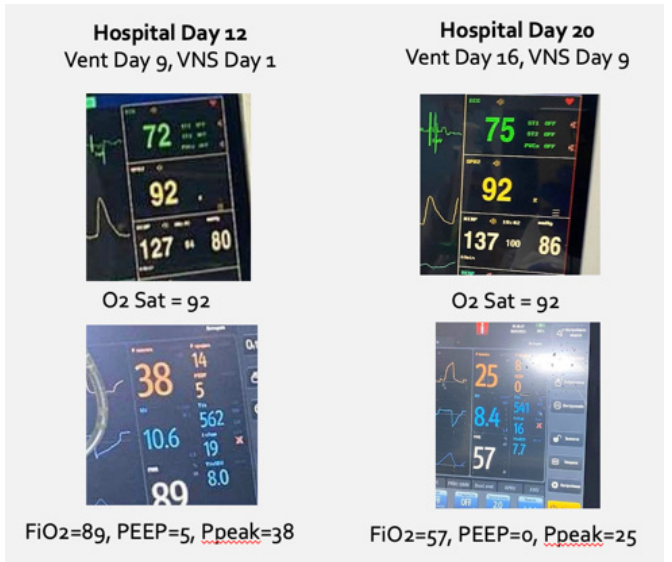
Image 1: Improvements in Respiratory Function with taVNS.
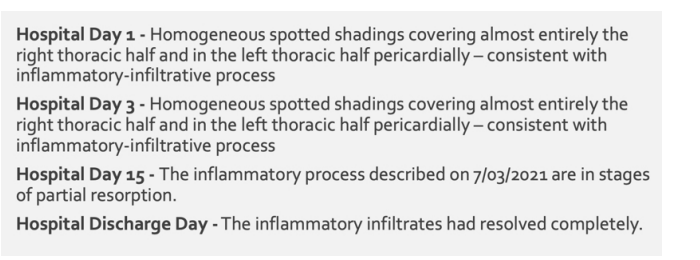
Figure 5: Chest radiograph findings.
At the time of discharge (hospital day 28), the patient was afebrile, her laboratory markers for inflammation had normalized, and her chest x-ray showed resolution of her pulmonary infiltrates (Figure 5). She was discharged home on oral antibiotics but without the requirement of home oxygen.
CRP improves with Initiation of taVNS
The patient's C-reactive protein (CRP) level was highly elevated during the first ten days of her hospitalization. After the first day of treatment with taVNS, the patient's CRP level dramatically dropped by 90% (Figure 6).
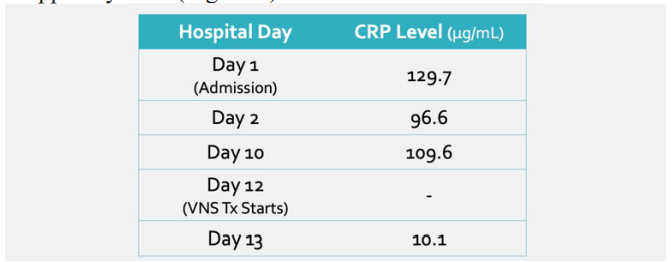
Figure 6: C-Reactive Protein measurements.
Relapse After Discharge from the Hospital
From a respiratory standpoint, the patient felt reasonably well after being discharged, and taVNS was discontinued ten days later. According to the family, within 24 hours of stopping taVNS at home, the patient developed a mild fever. Two days later, her oxygen saturation had declined to 50% (SpO2). Cefuroxime and home O2 were started, but the taVNS was not for some inexplicable reason. The patient generally struggled from a respiratory standpoint and refused to be re-hospitalized. After fourteen days of not improving with antibiotics and home oxygen, taVNS therapy was restarted, and within two weeks, her fever subsided,And her oxygen saturation levels had improved to 93% without supplemental oxygen.
She is now being maintained on a 5-minute, twice-daily regimen of taVNS as maintenance for the near future (Image 2).

Image 2: Patient using taVNS.
Method of Transcutaneous Auricular Vagus Nerve Stimulation
The patient received 5 minutes of transcutaneous vagus nerve stimulation (tVNS) four-time daily with an electronic neuromodulation device (Nemechek Technologies LLC). The taVNS device delivers stimulation at 10 Hz, 800uS, biphasic pulse wave with the voltage supplied at 10v below the perception threshold over 5-minute intervals.
The electrical stimulation was delivered through a small clip that makes contact within the concha and the back of the ear (Image 3). The ear and the clip contact points are cleaned with an alcohol swab before each treatment. After the placement of the clip, the voltage was slowly increased until the subject can perceive the current. The voltage was set just below the level of perception by gradually reducing the current until it was no longer detectable by the subject.

Image 3: Concha Clip Placement.
Case Report #2
The patient is a 69-year-old Caucasian male (#160, 5'9") from the United States with a history of myocardial infarction (coronary bypass at age 65), severe migraine headaches, and gastroesophageal reflux. He is on a chronic medication regimen of atorvastatin, amlodipine, famotidine, clopidogrel and propranolol.
The patient began feeling ill with a dry cough, myalgia on Day 1 (August 18th). On day 4 of his illness, the cough and myalgia had not resolved, and the patient tested positive for SARS-CoV-2 via rapid antigen testing.
On day 15 of his illness, his coughing began worsening and was now accompanied by other symptoms such as chills and generalized weakness. Examination revealed clear breath sounds, and his vitals were unremarkable (130/70 with a pulse rate of 73 bpm), and oxygen saturation was 97% at rest (Figure 7). By day 17 of his illness, audible wheezing was now present, and the patient was experiencing significant shortness of breath when ambulating short distances. He refused to seek any medical care outside of the home.
On day 19 of his illness, his oxygen saturation had declined to 90% while at rest. Breath sounds were greatly diminished. Cough,
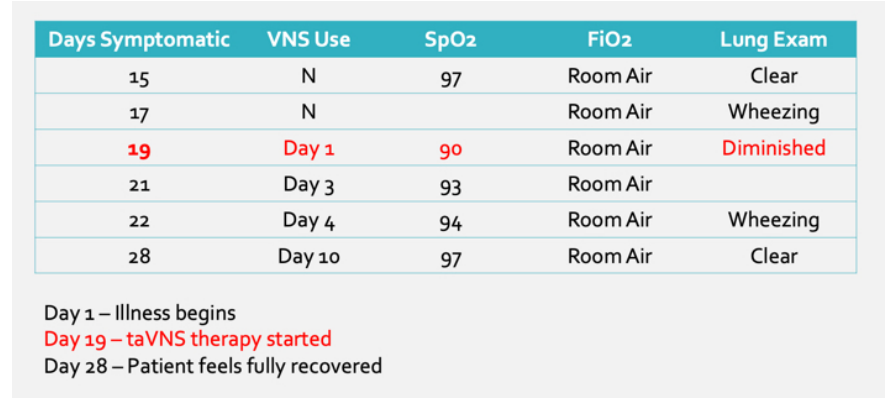
Figure 7: Case #2 - Oxygenation and mechanical ventilation indices.
Fatigue, and shortness of breath continued to worsen. His blood pressure and heart rate were 130/70 and 70 bpm, respectively.
After again refusing to be taken to the nearby emergency room, he was willing to try transcutaneous auricular vagus nerve stimulation (taVNS). His daughter was aware of our study report from Argentina and had a taVNS device at home for her son with autism.
He used the taVNS device three times per day, and the stimulation parameters were 10 Hz, 500 uS, and voltage adjusted to a level just below the perception threshold. The electrical contact consisted of a clip with two electrodes that rested over the concha and the back of the ear.
After starting taVNS, the patient's breath sounds and lung function steadily improved. Within two days of starting taVNS therapy, his oxygen saturation had increased from 90% to 93% at rest. The wheezing in his lungs had resolved, and breath sounds were clear.
By the 4th day of taVNS therapy, the patient's oxygen saturation had increased further to 94 %, and he felt well enough to go bowling but was disappointed that his scores were lower than his average.
By the 10th day of taVNS therapy, his oxygen saturation was at 97% at rest, but he still feels exhausted after minimal exertion but admits to feeling stronger every day. At this point, the taVNS was reduced to once daily. By the 25th day of cumulative taVNS therapy, he reported his energy levels being back to normal. No other medical treatments were used during his illness.
Discussion
While vaccination against SARS-CoV-2 improves hospitalization and mortality rates in wealthier countries, shortages of SARS- CoV-2 vaccines and basic medical supplies such as oxygen contribute to widespread death from COVID-19 [23]. The use of a vagus nerve stimulator offers a treatment option that, combined with the best current medical strategies, holds the potential to alter the clinical course in hospitalized individuals infected with SARS- CoV-2.
These two case studies demonstrate the rapid ability of taVNS to improve respiratory function in individuals infected with SARS-CoV-2 quickly. Both subjects showed severe declines in oxygenation that quickly reversed within a few days of initiating taVNS for 5 minutes three to four times per day.
Implementation of taVNS as a treatment option can be instituted quickly within any hospital or home setting. Technicians can be trained very quickly, taVNS is safe, the devices are inexpensive, and can be run off an inexpensive smartphone or tablet. Like a fingertip pulse oximeter, a single device can be easily decontaminated and used among multiple patients.
Electrical stimulation of the vagus nerve can modulate the working point of the inflammatory response in a wide variety of potentially lethal medical conditions (endotoxemia, ischemia/reperfusion injury, hemorrhagic shock, septic peritonitis) [18]. A growing number of publications agree with our position that taVNS can blunt the surge of inflammatory cytokines found in COVID-19 pneumonia and could favorably alter the course of the illness [11- 13,20,21].
Treatment of patients with taVNS offers them a potentially beneficial, safe, and inexpensive therapy when faced often with little to no other options in many resource-limited healthcare systems.
Conclusion
This case report shows the dramatic potential benefit transcutaneous auricular vagus nerve stimulation (taVNS) can have on a patient in respiratory failure from SARS-CoV-2 infection.
The development of non-invasive vagal nerve stimulation (taVNS), a non-pharmacological adjuvant, may help reduce the burden of COVID-19 on healthcare systems and deserve to be investigated. The aim of this paper is to promote further studies assessing non- invasive VNS as an adjuvant treatment for the management of COVID-19.
References
- Ye Q, Wang B, Mao J. The pathogenesis and treatment of the Cytokine Storm' in COVID-19. J Infect. 2020; 80: 607-613.
- Chitturi KR, Thacker S, Al-Saadi MA, et al. Successful treatment of acute heart failure in COVID-19-induced cytokine storm with tocilizumab: a case report. Eur Heart J Case Rep. 2020; 4: 1-6.
- Mustafa MI, Abdelmoneim AH, Mahmoud EM, et al. Cytokine storm in COVID-19 patients, its impact on organs and potential treatment by QTY code-designed detergent-free chemokine receptors. Mediators Inflamm. 2020; 23: 8198963. doi: 10.21467/preprints.139.
- Bradshaw PC, Seeds WA, Miller AC, et al. COVID-19: proposing a ketone-based metabolic therapy as a treatment to blunt the cytokine storm. Oxid Med Cell Longev. 2020; 6401341. doi: 10.1155/2020/6401341.
- Langer-Gould A, Smith JB, Gonzales EG, et al. Early identification of COVID-19 cytokine storm and treatment with anakinra or tocilizumab. Int J Infect Dis. 2020; 99: 291-
- doi: 10.1016/j.ijid.2020.07.081.
- Yessayan L, Szamosfalvi B, Napolitano L, et al. Treatment of cytokine storm in COVID19 patients with immunomodulatory therapy. ASAIO J. 2020; 66: 1079-1083. doi: 10.1097/ MAT.0000000000001239.
- Farooqi F, Dhawan N, Morgan R, et al. Treatment of severe COVID-19 with tocilizumab mitigates cytokine storm and averts mechanical ventilation during acute respiratory distress: a case report and literature review. Trop Med Infect Dis. 2020; 5: 112. doi: 10.3390/tropicalmed5030112.
- Dalamaga M, Karampela I, Mantzoros CS. Commentary: Phosphodiesterase 4 inhibitors as potential adjunct treatment targeting the cytokine storm in COVID-19. Metabolism. 2020; 109: 154282. doi: 10.1016/j.metabol.2020.154282.
- Saha A, Sharma AR, Bhattacharya M, et al. Tocilizumab: a therapeutic option for the treatment of cytokine storm syndrome in COVID-19. Arch Med Res. 2020; 51: 595-597. doi: 10.1016/j.arcmed.2020.05.009.
- Gonzalez-Nicolas MA, Gonzalez-Guerrero C, Perez- Fernandez VA, et al. Cilastatin: a potential treatment strategy against COVID-19 that may decrease viral replication and protect from the cytokine storm. Clin Kidney J. 2020; 13: 903- 905. doi: 10.1093/ckj/sfaa193.
- Boezaart AP, Botha DA. Treatment of Stage 3 COVID-19 With Transcutaneous Auricular Vagus Nerve Stimulation Drastically Reduces Interleukin-6 Blood Levels: A Report on Two Cases. Neuromodulation. 2021; 24: 166-167. doi: 10.1111/ner.13293.
- Staats P, Giannakopoulos G, Blake J, et al. The Use of Non- invasive Vagus Nerve Stimulation to Treat Respiratory Symptoms Associated With COVID-19: A Theoretical Hypothesis and Early Clinical Experience. Neuromodulation. 2020; 23: 784-788. doi: 10.1111/ner.13172.
- Antonelli G, Braida A, Nemechek P. Transcutaneous Vagus Nerve Stimulation is Associated with Lower Mechanical Ventilation and Mortality in COVID-19 Patients: An interim Safety Analysis. J Clin Exp Immunol. 2020; 5: 252-257.
- Borovikova L, Ivanova S, Zhang M, et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature. 2000; 405: 458-462. https://doi.org/10.1038/35013070.
- Tracey K. The inflammatory reflex. Nature. 2020; 420: 853- 859. https://doi.org/10.1038/nature01321.
- Tracey KJ. Physiology and immunology of the cholinergic anti-inflammatory pathway. J Clin Invest. 2007; 117: 289-doi:10.1172/JCI30555.
- Pan Y, Yu Z, Yuan Y, et al. Alteration of Autonomic Nervous System Is Associated With Severity and Outcomes in Patients With COVID-19. Front Physiol. 2021; 12: 630038. doi: 10.3389/fphys.2021.630038.
- Kaniusas E, Kampusch S, Tittgemeyer M, et al. Current Directions in the Auricular Vagus Nerve Stimulation I-A Physiological Perspective. Front Neurosci. 2019; 13: 854.
- Liu CH, Yang MH, Zhang GZ, et al. Neural networks and the anti-inflammatory effect of transcutaneous auricular vagus nerve stimulation in depression. J Neuroinflammation. 2020; 17: 54. https://doi.org/10.1186/s12974-020-01732-5.
- Nemechek Patrick. Vagus Nerve Stimulation is an Ideal Therapeutic Candidate for COVID-19 Infection. J Emerg Dis Virol. 2020; 5. dx.doi.org/10.16966/2473-1846.152.
- Nemechek Patrick. Transcutaneous Auricular Vagus Nerve Stimulation Holds Potential to Suppress COVID-19 Cytokine Storm. Integr Clin Med. 2020; 4: 1-6. doi: 10.15761/ ICM.1000179.
- Patrick Nemechek, Kathryn Moore. Autism spectrum disorder symptoms improve with combination therapy directed at improving gut microbiota and reducing inflammation. Applied Psychiatry. 2020; 1: 1-7.
- Richard Pérez-Peña. Some hospitals don't have enough oxygen to keep patients alive. Here's why. https://www.nytimes.com/2021/05/05/world/some-hospitals-dont-have- enough-oxygen-to-keep-patients-alive-heres-why.html.
- Bonaz B, Sinniger V, Pellissier S. Targeting the cholinergic anti-inflammatory pathway with vagus nerve stimulation in patients with Covid-19? Bioelectron Med. 2020; 6: 15. doi: 10.1186/s42234-020-00051-7.