Cervical Cancer: Epidemiological, Clinical and Therapeutic Aspects at Pointe Noire (Congo Brazzaville)
Author'(s): Ngatali Christian F.S1, Boumba A.L.M2, Mabiala A.Y3, Dougaka Moussavou R.A4, Moukassa D5 and Nkoua Mbon J.B6
1Department of Oncology and Internal Medicine, Loandjili General Hospital, Congo.
2Pathology Anatomy laboratory, Loandjili General Hospital,Pointe Noire, Congo.
3,6Department of Oncology, CHU Brazzaville, Congo.
4Department of Gynecology Tié-Tié Basic Hospital, Congo.
5General Hospital of Edith Lucie Bongo, Congo.
*Correspondence:
Dr. Ngatali Christian, Faculty of Health Sciences Brazzaville and Loandjili General Hospital.
Received: 17 December 2019; Accepted: 03 January 2020
Citation: Ngatali Christian F.S, Boumba A.L.M, Mabiala A.Y, et al. Cervical Cancer: Epidemiological, Clinical and Therapeutic Aspectsat Pointe Noire (Congo Brazzaville). Cancer Sci Res. 2020; 3(1); 1-5.
Abstract
Objective: To determine epidemiological, clinical and therapeutic aspect of cervical cancer in Pointe Noire.
Patients and Methods: This was a cross-sectional descriptive study that took place in the oncology department of loandjili General Hospital in Pointe Noire in the period from 1st January 2012 to 31st December 2018. All patients old more than 20 years, all patients having a complete file that is to say comprising a histological diagnosis. The variables studied were: age, level of education, parity; Clinical parameters revealing sign, stage of extension ;Histological type,The type of treatment. The multivariate analysis was done between age, parity and stage of extension. The statistical analysis and the data processing were carried out by the Excel 2016 software and the graphpad prism version 5 software. The statistical test used was the chi-square test.
Results: Of the 200 files, 57 files had met the inclusion criteria of our study, so the frequency of cervical cancer in our study in women was 22.8 %. The average age was 58,12 ± 13,31 years old with extrems of 28 years and 82 years. The most represented age group was the group age from 58 to 67 years old in 37% of cases, followed by the group age from 48 to 57 years old in 26% of cases.The study level the most commonly represented was the primary study in 70% of cases, followed by the secondary level study in 18 % of cases and the superior level study in 12% of cases. Only two women had a oral contraception. The average of parity was 3.32 ± 2 children with the extrems of 1 and 10 children. The revealing sign most represented was genital bleeding in 100% of cases. Almost all patient presented with an cervix ulcerate bourgeonnat. The most represented histological type was squamous cell carcinoma in 95% of cases and adenocarcinoma was represented by two cases (3%). The stage of extension most represented was locoregional stage in 70% of cases. The most represented treatment was chemotherapy in 56% of cases followed by radiochemotherapy in 31 % of cases. The bivariate analysis allowed to note that there was no relationship between age and cervical There was a relationship between parity and stage of extension of cervical cancer.
Conclusion: Cervical cancer is second cancer after breast cancer in women at Pointe Noire, patients arrived in late stage (locoregional and metastatic). The most represented treatment is chemetherapy alone. Late-stage diagnosed condition needs implementation of screening programme on the national level and to enhance the public health education to save the lives of Congolese women and make possible the access to radiotherapy in our countru in context of low incomes countries.
Keywords
Introduction
Despite considerable advances in diagnosis, treatment and prevention, cancer remains a major worldwide burden as it is the first cause of death in developed countries and the second in developing countries [1]. Cervical cancer With an estimated 570,000 cases and 311,000 deaths in 2018 worldwide, this disease ranks as the fourth most frequently diagnosed cancer and the fourth leading cause of cancer death in women [2]. Cervical cancer ranks second in incidence and mortality behind breast cancer in lower HDI settings; however, it is the most commonly diagnosed cancer in 28 countries and the leading cause of cancer death in 42 countries, the vast majority of which are in Sub-Saharan Africa and SouthEastern Asia.
The highest regional incidence and mortality rates are seen in Africa , with rates elevated in Southern Africa (eg, Swaziland, with the highest incidence rate), Eastern Africa (Malawi, with the highest mortality rate; and Zimbabwe), and Western Africa (Guinea, Burkina Faso, and Mali) [2]. In relative terms, the rates are 7 to 10 times lower in North America, Australia/ New Zealand, and Western Asia (Saudi Arabia and Iraq). Human papillomavirus (HPV) is the virtually necessary (but not sufficient) cause of cervical cancer [3] with 12 oncogenic types classified as group 1 carcinogens by the IARC Monographs [4].
Other important cofactors include immunosuppression (particularly human immunodeficiency virus), smoking, parity (a higher number of full-term pregnancies increases risk), and oral contraceptive use [5]. Over the last few decades, cervical cancer incidence and mortality rates reportedly have been in decline in many populations worldwide. Aside from screening (where available), these declines have been ascribed to factors linked either to increasing average socioeconomic levels or a diminishing risk of persistent infection with high-risk HPV, resulting from improvements in genital hygiene, reduced parity, and a diminishing prevalence of sexually transmitted disease [6].
The WHO recognizes three categories of epithelial tumors of the cervix: squamous, glandular (adenocarcinoma), and other epithelial tumors including neuroendocrine tumors and undifferentiated carcinoma [7]. Depending on stage, primary treatment consists of surgery, radiotherapy, or a combination of radiotherapy and chemotherapy [7]. To our knowledge few studies about this subject in our country were curry out, therefore our study aimed to determine the epidemiological, clinical and therapeutic aspects of Cervical Cancer in Pointe in the context of low income country.
Patients and Methods
This was a cross-sectional descriptive study that took place in the oncology department of loandjili General Hospital in Pointe Noire in the period from 1st January 2012 to 31st December 2018, a period of 8 years. Were included in our study: all patients old more than 21 years, all patients having a complete file that is to say comprising a histological diagnosis and an extension assessment performed using an abdominal CT scan and or abdominal sonography. Were excluded from our study all patients with no histological diagnosis. The variables studied were:
- Sociodemographic parameters: age, level of education, parity;
- Clinical parameters: revealing sign, stage of extension;
- Histological type;
- The type of treatment.
The stage of extension was made by the FIGO (international Federation of Gynecology and obstetrics) staging which was grouped in local (stage IA, IB and II), locoregional or advanced (stage IIB, III and IVA) and metastatic for stage IVB. The treatment was done by,surgery, radiotherapy associated with chemotherapy; chemotherapy was composed by platine drug at the dosis of 50 mg/m2. The collection of data was made from a previously written survey sheet, containing the different variables studied. The multivariate analysis was done between age, parity and stage of extension. Data entry was done using the Excel version 2016 software. Qualitative variables were represented in terms of number and percentage. Quantitative variables were represented effective and on average. The statistical analysis and the data processing were carried out by the Excel 2016 software and the graphpad prism version 5 software. The statistical test used was the chi-square test.
Results
During this study we collected 200 women cancer patients’ records. Of the 200 files, 57 files had met the inclusion criteria of our study, so the frequency of cervical cancer in our study in women was 28.5%. The average age was 58,12 ± 13,31 years with extrems of 28 years and 82 years.The most represented age group was the group age from 58 to 67 years in 37% of cases followed by the group age from 48 to 57 years in 26% of cases and the age group from 68 to 77 years in18% of cases (Table 1).

Table 1: Distribution according to age groups.
The study level the most commonly represented was the primary study in 70% of cases followed by the secondary level study in 18% of cases and the superior study level in 12% of cases. The average of parity was 3.32 ± 2 children with the extrems of 1 and 10 children. Most of patient had less than 3 children in 67% cases in one side, in another side women had more than 3 children in 23% of cases (Table 2). The telltate sign most represented was genital bleeding in 100% of cases. All patient presented with an cervix ulcerate budding and causing spantaneous bleeding by contact (Figure 1).
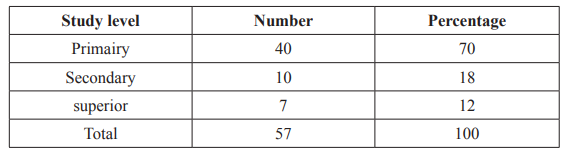
Table 2: Distribution according to study level.

Figure 1: Ulcerate, budding and bleeding on contact cervical cancer.
The most represented histological type was squamous cell carcinoma in 95% of cases and adenocarcinoma was represented by two cases (3%) and 1 cases of sarcoma (2%) (Figure 2). The stage of extension most represented was locoregional stage in 70% of cases followed respectivelly by the local stage and metastatic stage in 16% of cases and in 14% of cases (Table 3). To the patients that received treament (47%), the most represented treatment was chemotherapy in 56% of cases followed by radiochemotherapy in 37% of cases, followed by the association of radiotherapy+chemotherapie+surgery in 7% of cases. No patients received surgery or radiotherapy alone (Table 4).
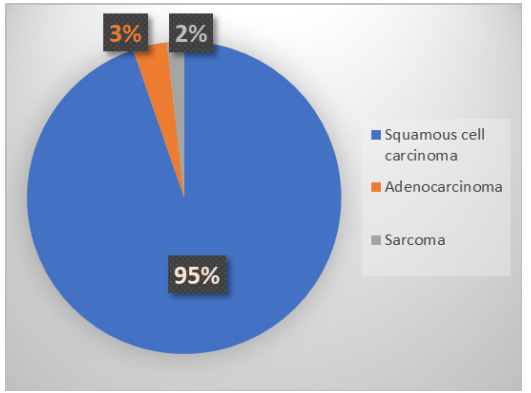
Figure 2: Representation of patients according to histological type.
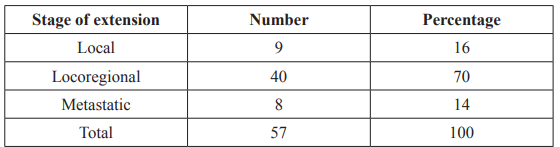
Table 3: Distribution according to the stage of extension.
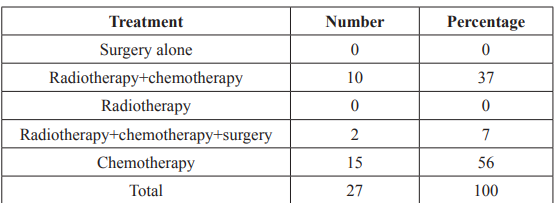
Table 4: Distribution of patient according to treatment.
In one side the majority of cervical cancer was found in women aged more than 50 years in 56 cases, in another side women aged of less than 50 years were represented in 11 cases. The bivariate analysis allowed to note that there was no relationship between age and cervical cancer (Table 5).
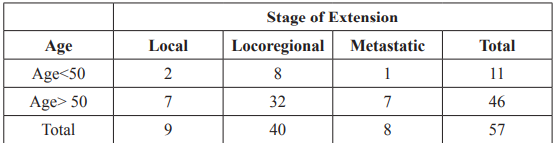
Table 5: Distribution according to age and stage of extension stage of extension. P>5% result non significant.
There was a relationship between parity and stage of extension of cervical cancer; women with parity less than 3 had more local stage than women with more than 3 parity, locoregional stage was more represented in women with less than 3 parity in 30 of cases; metastatic stage was most represented in women with more than 3 parity.
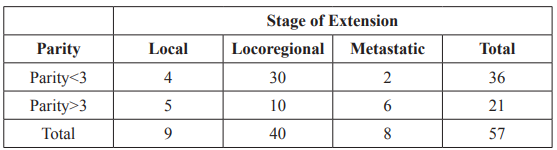
Table 6: Distribution according to parity and stage of extension stage of extension. PË?5% result significant.
Discussion
Our study presented some limitations. Indeed, despite of the small sample of our hospital study and the lack of grading stage that should determine the prognostic factors of cervical cancer, this study has described some epidemiological, clinical and therapeutic aspects of cervical cancer in Pointe Noire which is a city of about one million inhabitants. During our study, which took place at the General Hospital of Loandjili in the Oncology Department, we received a total of 200 women cancer patients. Of the 200 patients, 57 patients had cervical cancer and met all the inclusion criteria of our study. Thus, the incidence of cervical cancer in women during our study was 28.5%. Cervical cancer was the second cancer in our study. The results of the study conducted on the incidence of cancer in Yaoundé in 2012, shows that cervical cancer was the second cancer after breast cancer [8], and represented 13.8% of all cancers irrespective of gender. There is actually many diversities about the ranks of cervical cancer in women wotldwild. Cervical cancer is the fourth most common cancer among women [9].
However, 85% of cervical cancer diagnoses and related deaths occur in women living in LMICs (low and middle incomes countries) [9]. Cervical Cancer ranks second in incidence and mortality behind breast cancer in lower Human developpment indice settings; however, it is the most commonly diagnosed cancer in 28 countries and the leading cause of cancer death in 42 countries, the vast majority of which are in Subâ?Saharan Africa and Southâ?Eastern Asia.
The highest regional incidence and mortality rates are seen in Africa, with elevated rates in Southern Africa (eg, Swaziland, with the highest incidence rate), Eastern Africa (Malawi, with the highest mortality rate; and Zimbabwe), and Western Africa (Guinea, Burkina Faso, and Mali) [2,10]. In the majority of developping countries cervical cancer is the leading cancer. Cervical Cancer is currently the 11th most common cancer among women in the United States, with an incidence of 7.5 per 100 000 women and a mortality of 2.3 per 100 000 nationally between 2009 and 2013 [11]. The average age in our study was 58.12 ± 13,31years old. This age was higher than those found in Yaoundé by Sando et al. (52.73 ± 3.82 years), Engbang et al. in Douala (51.22 ± 11.93 years old), and Elmajjawi et al. Morocco, in his series of 696 cases that had an average age of 50 years [12-14].
Literature mentioned 47.36 years old in ivory coast and the 49.5 years old indicated by Hasiniatsy et al. in Madagascar [15,16]. The higher age in our study could be explaine by the fact that aging is a risk factor for persistent infection. The rate of persistent high-risk infection for women older than age 55 is 50%, while the persistent rate of women younger than 25 years old is 20% [17]. The age group most represented in our study was the age group from 58 to 67 years old in 37% of cases. In the N’Dah’s series the age group most represented was the age group from 45 to 54 years made up the majority of cases [15]. Most of patient had than 2 children in.
It has been demonstrated in literature that there is an association among increased risk of Cervical Cancer and higher parity [18- 20]. In our study the party was higer in 63% of cases.
The level of study was primary in 70% of cases in our study, this can be one of the causes of lack of knowlege about prevention of cervical cancer, that can lead to human papillomavirus infection by using the unprotected intercourse relationship. According to some studies, Human papillomavirus (HPV) types 16, 18, 31, 33, 35,39, 45, 51, 52, 56, 58, and 59 are classified as causes of Cervical Cancer [15] Also in low incomes countries the programm against cancer is often not available.
Only two patient received oral contraception in our study. of oestrogen-progestagen contraceptives are also a risk factor of Cervical Cancer [21]. In most of low incomes countries particularly in subsaharian Africa, patients come late and at that time disease are not limited in cervix, therefore the most revealing sign or clinical presentation was ulcerate budding cervix in 100% bleeding in our study. This result was simular to those of literarature [22,15].
The histological type most represented by squamous cell carcinome in 95% of cases in our study. This predominance of squamous was also the same in literature [16,23,24]. Other authors found the predominance of adenocarcinome [25]. The most represented stage of extension in our study was locoregional or advanced stage in 70% of cases. This was also found in literature [6,28]. This could be explained by the lack of knowledge about cervical cancer due to the primary level study in our study and the lack of policies about cancer prevention in general and particularly in cervical cancer.
Ouf of 57 patients only 27 received specific treatment soit 47.36% in our study so the most represented treatment was chemotherapy in 56% of cases followwed by radiochemotherapy in 37% of cases. No patient received surgery alone because they were in locoregional or advanced stage and the treatment at that stage is radiochemothrapy. Surgery is indicated in a local stage for the treatment of cervical cancer [27].
The comparison of the two groups (age<50 and age >50 years old) allowed to note that there was more cervical cancer (56 cases) in the the group of women with the age of more than 50 years old in our study. This result was not significant but could be explaine by the fact that getting aging is a risk factor for persistent infection. The rate of persistent high-risk infection for women older than age 55 is 50%, while the persistent rate of women younger than 25 years old is 20% [17]. There was relationship between parity and cervical cancer in our study. This results was stastiscally significant and was corroborate with the literature [18-20].
Conclusion
Cervical cancer is second cancer after breast cancer in women at Pointe Noire, patients arrived in late stage (locoregional and metastatic). The most represented treatment at Pointe Noire is chemetherapie alone. Radiotherapy is not avalable in our context of low incomes countries. The increasing trend of Cervical Cancer, its identification at advanced stage, increasing cost of treatment and poor knowledge about screening have increased the burden of cervical cancer. Although the incidence of Cervical Cancer in Pointe Noire is lower than other western countries, but Late-stage diagnosed condition rate is high due to scarcity of awareness, unavailability of Pap smear test, lack of follow-up and late presentation of cervical cancers. Late-stage diagnosed condition needs implementation of screening programme on the national level and to enhance the public health education to save the lives of Congolese women.
References
- Garcia M, Jemal A, Ward EM, et al. Global Cancer Facts & Figures 2007. Atlanta, GA. American Cancer 2007.
- Bray F, Ferlay J, Soerjomataram I, et Global Cancer Statistics GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer Journal for Clinicians. 2018; 68: 394-424.
- Walboomers JM, Jacobs MV, Manos MM, et Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999; 189: 12-19.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. 1997; 69: 1-631.
- Herrero R, Murillo R, Thun MJ, et Cervical cancer. Cancer Epidemiology and Prevention. 4th ed. New York: Oxford University Press. 2018; 925-946.
- International Agency for Research on Cancer (IARC). IARC Handbooks of Cancer Prevention: Volume 10-Cervix Cancer Lyon: IARC Press; 2005.
- Colombo N, Carinelli S, Colombo A, et al. Cervical Cancer: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Annals of 2012; 23: vii27-vii32.
- Enow OGE, Ndom P, Doh Current Cancer Incidence and trends in Yaounde, Cameroon. Oncology, Gastroenterology and Hepatology Reports. 2012; 1: 58-63.
- Cancer fact sheet no. 297. 2015.
- Ginsburg O, Bray F, Coleman MP, et The global burden of women’s cancers: A grand challenge in global health. Lancet. 2016; 16: 31392-31397.
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2013. Bethesda, MD: National Cancer Institute. 2016.
- Sando Z, Fouogue TJ, Fouelifack YF, et al. Profildes cancers gynécologique et mammaire à Yaoundé-Cameroun. Pan African Medical 2014; 17: 28.
- Engbang NJP, Mve KV, Tchente NC, et al. Aspects histo- épidémiologiques des cancers génitaux de la femme dans la région du Littoral, Cameroun. Pan African Medical Journal. 2015; 21: 116.
- Elmajjaoui S, Ismaili N, Kharmoum S, et Cancer du colutérin expérience du Maroc à propos de 696 cas. Cancer/ Radiothérapie. 2010; 14: 640-641.
- N’Dah KJ, Doukoure B, Troh E, et al. Epidemiological and Histological Aspects of Women Genital Cancers in Cote d’Ivoire. Open Journal of Obstetrics and Gynecology. 2014; 4: 516-523.
- Hasiniatsy NRE, Ernestho-ghoud IM, Ralamboson SA, et al. Prise en charge et suivi des cancers du col utérin la réalité à Antananarivo Madagascar. Journal Africain du Cancer. 2014; 6: 40-46.
- Wright JD. Cervical intraepithelial neoplasia: Terminology, incidence, pathogenesis, and prevention. 2014.
- Yoshikawa H, Negata C, Noda K, et al. Human papilloma virus infection with other risk factors for cervical neoplasma. Br J 1999; 80: 621-624.
- 1993 revised classification system for HIV infection and expanded surveillance definition for AIDS adolescents and MMWR Morb Mortal Rep. 1992; 41: 1-19.
- Bosch FX, Munoz N, de Sanjose S, et al. Human papilloma virus and cervical intraepithelial neoplasia grade III/carcinoma in situ a case control study in spain and Colombia. Cancer Epidemiol Biomarkers 1994; 23: 42-49.
- La Vecchia C, Boccia Oral Contraceptives Human Papillomavirus and Cervical Cancer (Link Is External). European Journal of Cancer Prevention. 2014; 23: 110-112.
- Engbang Ndamba Jean Paul, Tchente Nguefack Charlotte, Owona Manga Léon Jules, et Epidemiological and Histological Profile of Cervical Cancer in Cameroon: About 2078 Cases. Open Journal of Obstetrics and Gynecology. 2016; 6: 232-239.
- Nayama M, Nouhou H, Madougou-Sunna K, et Breast and Gynecological Cancers Epidemiological and Histological Aspects Made from the Record of Pathology Laboratory of the Faculty of Science and Heath Niamey Niger. Medical Journal of Mali. 2006; 31: 43-49.
- Elmajjaoui S, Ismaili N, Kharmoum S, et Cancer du colutérin expérience du Maroc, à propos de 696 cas. Cancer/ Radiothérapie. 2010; 14: 640-641.
- Mubiayi N, Bogaert E, Boman F, et al. Histoire du suivi cytologique de 148 femmes atteintes d’un cancer invasif du col utérin. Gynécologie Obstétrique & Fertilité. 2012; 30: 210-217.
- Bhurgri Y. Karachi cancer registry data-implications for the National Cancer Control Program in Pakistan. Asian Pac J Cancer 2004; 5: 77-82.
- Anuja Jhingran, Ana Rodriguez. Neoplasm of cervix. Cancer Medicine edition. 2018; 1280-1303.