Cirrhosis and Its Complications at the Donka National Hospital of Conakry
Author'(s): Diallo Mamadou Sarifou1,2*, Youssouf Oumarou3, Pare Stella Line Emmanuella7, Diallo Ahmed Tidiane1,2, Diallo Kadiatou1,2, Diallo Djenabou1,2, Wann Thierno Amadou5,2, Bah Mamadou Lamine Yaya5,2, Diakhaby Mamadou5, Kanté Mamadou Aliou5, Sylla Djibril5,2, Soro Dramane4, Diallo Abdourahmane N'Djouria6
1Hepato-Gastroenterology Department of the Donka National Hospital, Conakry, Guinea.
2Faculty of Health Sciences and Techniques, Gamal Abdel Nasser University, Conakry, Guinea.
3Bangui Community University Hospital Center, Internal Medicine Department, Central African Republic.
4Hepato-Gastroenterology Department, Cocody University Hospital, Abidjan, Ivory Coast.
5Department of Internal Medicine, Donka National Hospital, Conakry, Guinea.
6SOS Hepatitis Guinea.
7Hepato-Gastroenterology Department of the Regional Hospital Center of Fada N'Gourma, Burkina Faso.
*Correspondence:
Dr. Mamadou Sarifou DIALLO, Hepato-Gastroenterology Department, Donka National Hospital CHU Conakry, Guinea, Tel: 00224628690551.
Received: 24 Apr 2024 Accepted: 05 Jun 2024
Citation: Diallo M Sarifou, Youssouf Oumarou, Pare Stella Line E, et al. Cirrhosis and Its Complications at the Donka National Hospital of Conakry. Gastroint Hepatol Dig Dis. 2024; 7(3): 1-7.
Abstract
Introduction: Patients with liver cirrhosis have a very high risk of complications.
Method: This was a descriptive and analytical cross-sectional study covering all cirrhotic patients hospitalized in our department during the study period. It was carried out from January 1, 2022 to March 30, 2023, i.e. 13 months in hospitalization in the hepato-gastroenterology department of the Donka national hospital of the Conakry University Hospital.
The aim of this work was to study cirrhosis and its complications based on clinical and paraclinical data collected in cirrhotic patients followed in our department.
Results: The prevalence of cirrhosis in our department was 28.28%. There were 110 men (55%) and 90 women (45%); i.e. a M/F sex ratio of 1.22. The average age of our patients was 43 years with extremes of 22 and 72 years. The main reasons for hospitalization were: edemato-ascitic syndrome 60.71%, abdominal pain 21.43%, digestive bleeding 18.28%, hepatomegaly 7.14%, jaundice 3.57%, disorders of consciousness (hepatic encephalopathy) 3.57%. The main complications of cirrhosis were: ascites associated with edema in 60.71%, hepatic encephalopathy in 23%, digestive hemorrhage 18.28%, infection of ascitic fluid (13.03 %), hepatocellular carcinoma (10%), hepatorenal syndrome (3.20%). The etiologies of cirrhosis were: viral B (57.14%), viral C (10.71%), mixed alcohol + HBV (10.71%), alcoholic (7.86%), HBV + HCV co-infection (3.57%), HBV+HDV co-infection (1%), autoimmune (3%) and of undetermined cause (6%). Esophagogastroduodenal endoscopy showed esophageal varices in 67% of cases. The main circumstances of death were: digestive hemorrhage (25.32%), infectious shock (26.58%), encephalopathy hepatic (25.32%), hepatorenal syndrome (12.66%) and hepatocellular carcinoma (10.12%).
Conclusion: Cirrhosis is the ultimate consequence of most chronic liver diseases, most often linked to chronic viral hepatitis B and C, excessive alcohol consumption or non-alcoholic steatohepatitis (NASH). It is a real public health problem with increasing incidence worldwide and one of the leading causes of death. Complications of cirrhosis are the consequences of hepatocellular insufficiency and/or portal hypertension and/or hepatocellular carcinoma. The difficult-to-access curative treatment which is liver transplantation; hence the interest in prevention based on the fight against the etiological factors of cirrhosis; in particular the promotion of vaccination against viral hepatitis B
Keywords
Introduction
Cirrhosis is defined histologically as diffuse damage to the liver parenchyma with hepatocyte necrosis and especially annular fibrosis delimiting regeneration nodules which disrupt the normal lobular architecture of the liver [1]. Cirrhosis is the major stage in the development of hepatic fibrosis induced by most chronic liver diseases [2].
This pathology poses, due to its frequency, a real public health problem in the world and particularly in Africa. In fact, it is one of the main causes of death from disease and thousands of people die from it every year. However, the prevalence of cirrhosis in the population is not exactly known [3]. The prevalence of cirrhosis was estimated at 0.15% or 400,000 in the United States where it caused 25,000 deaths in 1998 [4,5].
This may be an underestimate as we recognize the high prevalence of undiagnosed cirrhosis in nonalcoholic steatohepatitis (NASH) and hepatitis C. Similar figures have been reported in Europe, and are even higher in most countries. Asian and African countries where viral hepatitis B and C are common. As compensated cirrhosis often remains undetected for long periods, it can be reasonably estimated that up to 1% of populations may have histological cirrhosis [6].
The progression of cirrhosis leads to liver failure and portal hypertension responsible for clinical signs in addition to disturbances in biological parameters. The main clinical complications are ascites with its attendant complications, digestive hemorrhage and, increasingly, hepatocellular carcinoma (HCC) [7]. Cirrhosis must be considered a serious illness, because 50% of patients die within 5 years of diagnosis and two out of three cirrhotic patients die of a hepatic cause [3]. The etiologies of cirrhosis are numerous and varied depending on the region of the globe. In the United States, the most common causes of cirrhosis are chronic liver disease, hepatitis C virus (HCV), and alcoholic liver disease [8]. In Europe, cirrhosis accounts for 1.8% of all deaths, representing 170,000 deaths per year. In Europe, the main causes are alcoholic liver disease, NASH and HCV [9]. The most common causes of cirrhosis worldwide are chronic viral hepatitis B (HBV), HCV, alcoholic liver disease, NASH, hemochromatosis, autoimmune diseases [10].
The natural history of cirrhosis is characterized by an asymptomatic phase called “compensated cirrhosis” followed by a progressive phase marked by the development of complications of portal hypertension (PH) and/or hepatic dysfunction, called “decompensated cirrhosis”. In the compensated phase, portal pressure may be normal or below the threshold level identified for the development of varicose veins or ascites [11]. As the disease progresses, portal pressure increases and liver function decreases, leading to the development of ascites, PH-related gastrointestinal hemorrhage, hepatic encephalopathy (HE), and jaundice. The development of one of these complications marks the transition from a compensated phase to a decompensated phase. Progression can be accelerated by the development of other complications such as rebleeding, renal failure (refractory ascites, hepatorenal syndrome), hepatopulmonary syndrome and sepsis (spontaneous bacterial peritonitis) and hepatocellular carcinoma [11].
In Guinea, although decompensated cirrhotic patients are frequently hospitalized in our department, publications enrolling a large sample of cirrhotic patients are not available. It is in view of this state of affairs that we undertook this work, the aim of which was to study cirrhosis and its complications based on clinical and paraclinical data collected in cirrhotic patients followed in our department.
Material and Methods
We carried out a descriptive and analytical cross-sectional study covering all patients hospitalized in our department during the study period. It was carried out from January 1, 2022 to March 30, 2023, i.e. 13 months in hospitalization in the hepato- gastroenterology department of the Donka national hospital of the Conakry University Hospital.
Included were patients of all ages, genders and origins hospitalized in the department during the study period and who agreed to participate in the study by oral consent in whom the diagnosis of liver cirrhosis was made, on a following set of arguments:
- Dysmorphic liver on ultrasound or CT scan
- Clinical signs of portal hypertension (superficial epigastric cutaneous venous circulation, ascites).
- Clinical and biological signs of hepatocellular insufficiency (jaundice, ascites, clubbing, hepatic encephalopathy, decreased libido, secondary amenorrhea, diamond-shaped pubic hair disorder in men, gynecomastia, testicular atrophy, stellate angioma, hypoalbuminemia, ascitic fluid low in protein, hypertransaminaseemia).
- Presence of signs of portal hypertension on liver ultrasound (portal vein diameter greater than 12 mm, splenomegaly).
- Hepatomegaly with a sharp lower edge
- Presence of endoscopic signs of hypertension (esophageal varices, gastric varices, antral vascular ectasia, ulcer)
The criteria for non-inclusion of patients were:
- Patients with cirrhosis for whom no additional examination is carried out
- Non-cirrhotic patients
- Cirrhotic patients who refused to participate in the study
Sociodemographic parameters
- Age
- Sex
Clinical parameters
− Reason for consultation
− The patient's personal history
− The clinical data collected on admission were vital signs, abdominal pain, diarrhea, vomiting, jaundice, digestive hemorrhage, hepatic encephalopathy, alteration of general condition (AEG), macroscopic appearance of ascitic fluid: citrine, cloudy or hematic.
Biological parameters
− Blood Count (FBC)
− Prothrombin level (PT)
− Transaminases
− Total bilirubinemia
− Serum creatinine
− The protodogram: total proteins, albumin and presence or absence of a beta-gamma block
− Viral markers: HBV, HCV, HDV
− Autoimmune markers: anti-nuclear antibodies (Ab), anti- smooth muscle Ab, anti-cytosol LC1 Ab, anti-LKM1 Ab (Liver Kidney Microsome), anti-SLA Ab (Specific Liver Antigen), anti-mitochondria M2 Ab
− Bilharzial serology was investigated
− Alpha 1 anti-trypsin deficiency, Wilson's disease and hemochromatosis have not been investigated.
− The biopsy of the liver was not carried out and the diagnosis of cirrhosis was retained on the basis of clinical arguments (presence of signs of hepatocellular insufficiency, portal hypertension, hepatomegaly with a sharp lower edge), paraclinical by the presence of hepatic dysmorphism on ultrasound and/or CT scan, the presence of endoscopic signs of PH.
− The analysis of ascites fluid includes, the macroscopic aspect, a cytological examination (leukocyte count: PNN and lymphocytes), chemical (dosage of protein levels).
Radiological parameters
Abdominal ultrasound or abdominal scanner: to assess the intra-abdominal organs; especially look for hepatic dysmorphia, signs of portal hypertension (PH), a nodule suspicious for hepatocellular carcinoma (HCC) and/or the kinetics of HCC “Wash out”; appreciate the abundance of ascites.
Esophagogastroduodenal fibroscopy: looking for esophageal varices, gastric varices; portal hypertension gastropathy; Antral vascular ectasias.
- Prognosis: assessed by the CHILD-PUGH score
- Evolution: favorable with improvement of clinical signs and unfavorable with death of the patient
Data Collection, Entry and Analysis
− Data collection was carried out using a survey form established for this purpose (see appendices)
− Data entry was done in EPI-INFO VERSION 7
− The tests used for data analysis were Pearson's Chi-square test; corrected Chi square and Fisher's exact test
− The alpha threshold was set at 5%
Results
A total of 707 hospitalized patient files were recorded including 233 cirrhotic cases, thirty-three of whom refused to participate in the survey. Two hundred patients retained. The prevalence of cirrhosis in our department was 28.28%. There were 110 men (55%) and 90 women (45%); i.e. a M/F sex ratio of 1.22.
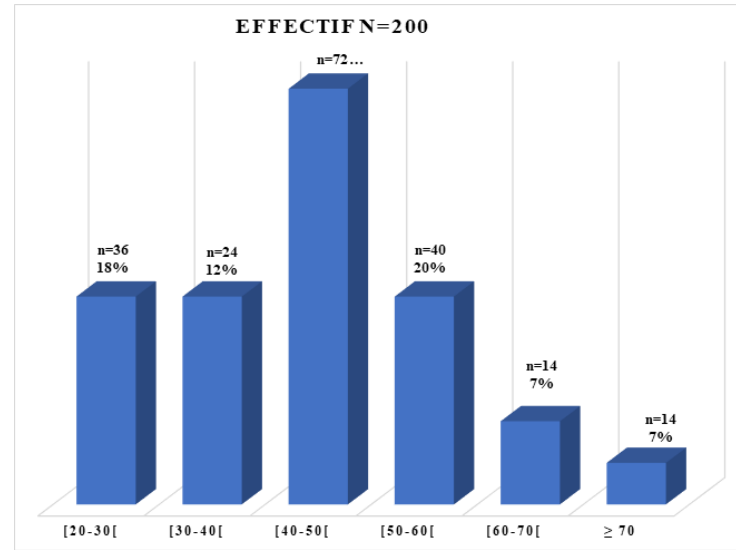
Figure 1: Distribution of patients according to age groups.
The average age of our patients was 43 years with extremes of 22 and 72 years. The age group of 40-50 was the most affected followed by that of 50-60 years with respective frequencies of 36% and 20%.
The main reasons for hospitalization were: edemato-ascitic syndrome 60.71%, abdominal pain 21.43%, digestive bleeding 18.28%, hepatomegaly 7.14%, jaundice 3.57%, disturbances of consciousness (hepatic encephalopathy) 3.57%, fever 3%, alteration of general condition (AEG) 2.09%, splenomegaly 2%, diarrhea 1.09%, vomiting 1%, constipation 0.8%.
The history of our patients was: jaundice 35.71%, scarification 28.57%, surgery 15.02%, blood transfusion 12.67%, dental care 10%, tattoo 8%, alcohol 7% and digestive bleeding 5%.
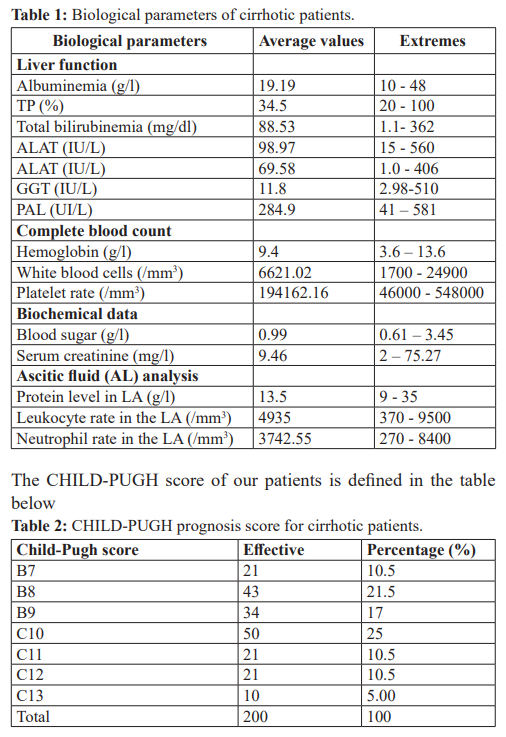
On physical examination, signs of hepatocellular insufficiency were found in 60.21%, signs of portal hypertension in 72%, hepatomegaly with a sharp lower edge in 40.60% of cases. The biological parameters are presented in the table below.
The main complications of cirrhosis were: ascites associated with edema in 60.71%, hepatic encephalopathy in 23%, digestive hemorrhage 18.28%, infection of ascitic fluid (13.03 %), hepatocellular carcinoma (10%), hepatorenal syndrome (3.20%).
The etiology of cirrhosis was: viral B (57.14%), viral C (10.71%), mixed alcohol + HBV (10.71%), alcoholic (7.86%), HBV + HCV co-infection (3.57%), HBV+HDV co-infection (1%), autoimmune (3%) and of undetermined cause (6%).
Esophagogastroduodenal endoscopy showed esophageal varices in 67% of cases, including (17%) with red signs, portal hypertension gastropathy in 40.45%, gastric varices in 9%, antral ectasias in 1.5% of cases.
On abdominal ultrasound and/or CT: heterogeneous liver in 60% of cases, hypertrophy in 50% of cases, dysmorphia (30%), atrophy in 25% of cases, splenomegaly (60%), dilatation of the trunk carries in 45% of cases. Nodules suspicious for hepatocellular carcinoma (HCC) and having the kinetics of HCC on CT in 10% of cases. The appearance of the ascites fluid was citrine yellow in 80% of cases, cloudy in 15% of cases and hematic in 5% of cases. There is a significant association between cloudy ascitic fluid and spontaneous ascitic fluid infection (p=0.00).
There is a significant link between abdominal pain and spontaneous ascitic fluid infection (p = 0.01).
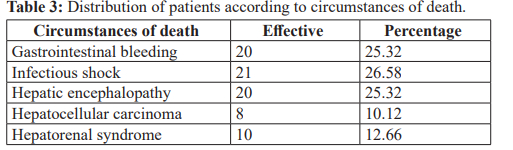
According to the evolution, 121 patients or 60.5% were favorable and 79 patients or 39.5% died. The average length of hospitalization was 14 days. The outcome was favorable in 60.5% of our patients and unfavorable with patient death in 39.5% of cases. Death occurred in 79 patients (39.5%).
The causes or circumstances of death were:
Discussion
The main limitations of this study were: the single-center nature of the study, the large number of incomplete files, the high cost of examinations, the absence of subsidy and/or health insurance. But nevertheless, this study made it possible to determine the prevalence of cirrhosis, the clinical and paraclinical aspects as well as its complications in our department.
The prevalence of cirrhosis in our department was 28.28%. This prevalence would be underestimated due to the fact that many patient files were incomplete. Our results are slightly better than those reported by Sehonou J et al. [12] in Benin and close to those of Camengo-Police SM et al. [13] in the Central African Republic of 19.7% and 22.6% respectively.
The average age of 43 years is comparable to those found by DIA et al. [14], Maiga et al. [15], Camengo-Police SM et al. [13] and Attia et al. [16] which were respectively 42 years; 43 years ; 44 years old and 48 years old. The age group of 40-50 was the most affected followed by that of 50-60 years with respective frequencies of 36% and 20% (Figure 1). We notice that our cirrhotic patients are young. Young people are more exposed to the risk of infection by HBV and HCV in Sub-Saharan Africa; this viral infection appears much earlier (around 40 years), which could explain this predominance in this age group [14,17]. The sex ratio is 1.22. This male predominance is also found in the vast majority of studies with a sex ratio often between 1 and 5 [14,17,18]. Series with a female predominance are rare, such as that of Ouakaa-Kchaou et al. [19] in Tunisia, which reported a sex ratio of 0.66. The main reasons for hospitalization were represented by edemato- ascitic syndrome 60, 71%, abdominal pain 21.43%, digestive
hemorrhage 18.28%, hepatomegaly 7.14%, jaundice 3.57%, impaired consciousness (hepatic encephalopathy) 3.57%. In Mali, MAIGA et al. [15] found edematous-ascitic syndrome (70.2%); jaundice (54.4%) and hematemesis (14%). In Ivory Coast, ATTIA et al. [16] found edematous-ascitic syndrome in 68.6%; jaundice (25.2%) and digestive hemorrhages (15.1%). Their results are superimposable to ours. The clinical manifestations are diverse but generally represented at variable frequencies by abdominal distention, abdominal pain, fever, jaundice and digestive bleeding [18,20]. In our series, hepatocellular insufficiency syndrome was found in 60.21%, portal hypertension syndrome in 72%. As for Wallerstedt et al. [21] in Sweden, they found on admission of patients stellate angiomas (52%), abdominal pain (33.6%) and fever (6%). In the United States, Chinnock et al. [22] reported nausea and/or vomiting (26.44%), fever (20.8%) and digestive bleeding (11.2%) as symptoms appearing in the last 24 hours before patients' hospitalization, they found abdominal distention or pain (86%) and impairment of higher functions (5.5%) on physical examination.
In our study, the history of our patients was: jaundice 35.71%, scarification 28.57%, surgery 15.02%, blood transfusion 12.67%, dental care 10%, tattoo 8 %, alcohol 7%. These antecedents constitute the risk factors for viral contagion in our context. As for Ouavene JO et al. [23], jaundice (63.5%), alcohol (34%), viral hepatitis B (28%) were the main antecedents of their patients.
Thebiological abnormalities found are: anemia, hyperbilirubinemia, hypoprothrombinemia, hypoalbuminemia, hepatic cytolysis (Table 1). In Tunisia, Ouakaa-Kchaou et al. [19] noted as biological abnormalities in their patients: hypoalbuminemia, hypoprothrombinemia, thrombocytopenia, hyperbilirubinemia, hyponatremia and hypercreatininemia. These biological abnormalities are observed in all series of cirrhotic patients, they often contribute to establishing the diagnosis of cirrhosis (in the absence of a liver biopsy as in our series); but also help above all to determine the prognosis of cirrhosis by establishing the CHILG- PUGH score for the severity of cirrhosis.
In our patients, the progressive stage of cirrhosis was severe Child B (50%) and Child C (50%) and 25% had Child C10 (Table 2). In Ivory Coast, Attia et al. [16] found in their series of cirrhotic patients decompensated in the edematous-ascitic mode the following distribution: 59.1% Child C, 36.4% Child B.
The main complications of cirrhosis in our series were: ascites 60.71%, hepatic encephalopathy in 23%, digestive hemorrhage 18.28%, ascitic fluid infection (13.03%)., hepatocellular carcinoma (10%), hepatorenal syndrome (3.20%).
In the Central African Republic, Camengo-Police SM et al. [13] noted: ascites associated or not with edema of the lower limbs (74.9%), digestive hemorrhage (22.3%), hepatocellular carcinoma (20.2%), hepatorenal syndrome (2.2%). This observation is identical to that of Diarra M et al. [24] in Mali who reported as complications of cirrhosis, digestive bleeding, hepatic encephalopathy and hepatocellular carcinoma with respective frequencies of 39%; 38% and 23%. The absence of specific symptoms meant that most patients were admitted late after the onset of complications. In Guinea, there is often a delay in diagnosis of cirrhosis like most other diseases. This delay in diagnosis could be explained on the one hand by the primary recourse to traditional medicine and on the other hand by a limited technical platform. Diallo MS et al. [25] reported in their study that 17.64% of their patients took traditional self-medication made from a combination of several decoctions which could thus explain hepatic cytolysis as well as the elevation of GGT, ALP and bilirubin in our study context. The etiology of cirrhosis was mainly viral B (57.14%), viral C (10.71%), mixed alcohol + HBV (10.71%), alcoholic (7.86%), co-infection HBV+HCV (3.57%), HBV+HDV co-infection (1%), autoimmune (3%) and of undetermined cause (6%).
Our results are superimposable to those reported by Dia et al. [14] who found 67% of viral B etiology; 2% of alcoholic origin and 31% of undetermined cause and Attia et al. [17] who noted 45.3% viral B etiologies, 10% viral C etiologies; 20.9% of undetermined cause. In Mali, Diarra M et al. [24] found 33.3% of viral cause B, 10.5% of cases related to alcohol poisoning and 31.57% of cases of non-causes determined.
In Tunisia, in the study by Ouakaa-Kchaou A et al. [19] viral C causes are predominant (49%), followed by viral B causes (19%), alcoholic (3.6%) and undetermined causes represented 20% of cases. In the study by Camengo -Police SM et al. [13] the etiology of cirrhosis was post-hepatitic B (62.5%), post B and alcoholic (3.3%), alcoholic (17.9%), post hepatitic C (8.7%), post B and D (3.8%) and indeterminate (3.8%). We found esophageal varices in 67% of cases including (17%) with signs red, portal hypertension gastropathy in 40.45%, gastric varices in 9%. This result is superimposable to that of Maiga et al. [26] in Mali who found esophageal varices in 82.4% of cases. Abdominal ultrasound revealed a heterogeneous liver in 60% of cases, an enlarged liver in 50% of cases., dysmorphia (30%), splenomegaly (60%), dilatation of the trunk in 45% of cases. Nodules suspicious for hepatocellular carcinoma (HCC) and having the kinetics of HCC on CT in 10% of cases. These results agree with those in the literature which have shown the reliability of ultrasound in the diagnosis of liver cirrhosis [3,27]. The appearance of the ascites fluid was citrine yellow in 80% of cases, cloudy in 15% of cases and hematic in 5% of cases. There is a significant association between cloudy ascitic fluid and spontaneous ascitic fluid infection (p= 0.00) as well as abdominal pain and spontaneous ascitic fluid infection (p= 0.01). As for Dia et al. [14] and Attia et al. [16] who respectively reported cloudy ascitic fluid in 53.3% and 66.7% of cases. The cloudy appearance of the ascites fluid is very suggestive of ISLA but also the clear or citrine yellow appearances do not exclude it [20]. The outcome was favorable in 60.5% of our patients and unfavorable with patient death in 39.5% of cases. Death occurred in 79 patients (39.5%). This death rate is in the interval between 15% and 65% of several African series [12,13,18,24]. This mortality is comparable to that reported by Rimiola A et al. who found a mortality between 10% and 46% [28].
For Sheer TA et al. [29], this mortality increased from 100% in 1960 to 60-70% between the years 1970-1980 to 30% over the last ten years. The main circumstances of death were: digestive hemorrhage (25.32%), infectious shock (26.58%), hepatic
encephalopathy (25.32%), hepatorenal syndrome (12.66%) and hepatocellular carcinoma (10.12%). This high mortality in our series could be explained on the one hand by the late consultation of patients due to the absence of specific symptoms of cirrhosis, the harmful role of traditional treatment, aggravating the liver disease and on the other hand our weak technical platform. For Karoui S et al. [30], hepatic encephalopathy, digestive bleeding and hepatocellular carcinoma are the most likely factors in the death of cirrhotic patients.
Conclusion
Cirrhosis is a real public health problem with increasing incidence worldwide and one of the leading causes of death. Any chronic attack on the liver can lead to cirrhosis. The etiologies are dominated in our country by viral causes (HVB, HCV and VHD). Hence the need to promote vaccination against viral hepatitis B. We must not overlook the current emergence of metabolic causes. The occurrence of a complication marks a decisive turning point in the evolution of patients suffering from cirrhosis with heavy morbidity and significant mortality.
Declaration for Human Rights
The hospital has consented to the use of data from patients who have been consulted in the department. This study was approved by the hospital ethics committee and the principles of the Declaration of Helsinki were followed.
References
- Martin Pathological anatomy of cirrhosis and pre-cirrhotic lesions. Encycl Med Chir. Paris, Liver –Pancreas. 1983; 5: 7034.
- Friedman Liver fibrosis from bench to bedside. J Hepataol. 2003; 38: S38-53.
- Calès P. Can cirrhosis be diagnosed early? The medical competition: 117-137.
- Bethesda N. Digestive diseases in the United States: Epidemiology and 1994. NIH Publication No. 94-1447.
- National Center for Health Statistics: US Department of Health and Human Services, Centers for Disease Control and Prevention. Hyattsville, MD: 2005.
- Detlef S. Liver cirrhosis. Lancet. 2008; 371: 838-
- Voitot H. Biology and cirrhosis. Francophonrd Laboratories Review. 2006; 387: 65-671.
- Wong RJ, Maria A, Ramsey Cheung, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015; 148: 547-555.
- Blachier M, Henri Leleu, Markus Peck-Radosavljevic, et al. The burden of liver disease in Europe: a review of available epidemiological data. J Hepatol. 2013; 58: 593-608.
- Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. AM Fam Physician. 2006; 74: 756-762.
- D’Amico G, Garcia-Tsao G, Calès P, et al. Diagnosis of portal hypertension: how and In: R De Franchis (Ed). Hypertension Portal III. Proceedings of the third Baveno international consensus Workshop on definitions, methodology and therapeutic strategies. Blackwell Science, Oxford. 2001: 36-64.
- Sehonou J, Kodjoh N, Sake K, et Liver cirrhosis in Cotonou (Republic of Benin): clinical aspects and factors linked to death. Med Trop. 2010; 70: 375-378.
- Camengo-Police SM, Koffi B, Boua-Akelo N, et al. Complications of cirrhosis at the Friendship University Hospital of Bangui. Black African Medicine. 2014; 61: 537-542.
- Dia D, Serme YK, Bassene ML, et al. Spontaneous ascitic fluid infection in Dakar, Senegal: Study of fifty-five cirrhotic patients. Med sante Trop. 2014; 24: 55-57.
- Maiga MY, Traoré HA, Dembélé M, et al. Ascites fluid infection in the medical departments at the Point “G” National Hospital. Digestive surgical medicine. 1996; 25: 219-222.
- Attia KA, N’Dri Yoman AT, Sawadogo A, et Spontaneous infection of ascitic fluid in African cirrhotics. Descriptive study about 12 cases. Bull Soc PatholExot. 2001; 94: 319-321.
- Attia KA, Ackooudou N’Guessan KC, N’Dri Yoamn AT, et al. Child-PughTurcott versus MELD score for predicting survival in retrospective cohort of black Africancirrhotic patients. World J Gastroenterol. 2008; 14: 286-291.
- Diallo MS, Wann TA, Diallo K, et al. Prevalence and risk factors for the occurrence of spontaneous ascitic fluid infection (SLAI) in cirrhosis. Jaccr Africa. 2023; 7: 214-222.
- Ouakaa-Kchaou A, Belhadji N, Abdelli N, et al. Survival in Tunisian cirrhotic patients. Tunisia Med. 2010; 88: 804-808.
- EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. Journal of Hepatology. 2010; 53: 397- 417.
- Wallerstedt S, Olsson R, Simren Abdominal tenderness in ascites patients indicates spontaneous bacterial peritinitis. Eur I Internal Med. 2007; 18: 44-47.
- Chinnock B, Afarian H, Minnigan H, et Physician clinical impression does not rule out spontaneous bacterial peritonitis in patients undergoing emergency department paracentesis. Ann Emerg Med. 2008; 52: 268-273.
- Ouavene JO, Koffi B, Mobima T, et Liver cirrhosis at the Bangui Friendship Hospital: epidemiological, clinical, ultrasound aspects and diagnostic problems. African Journal of Medical Imaging. 2014; 5: 1-12.
- Diarra M, Konaté A, Soukho A, et Evolutionary aspects of cirrhotic disease in a Hepato-Gastro-Enterology department in Mali. Mali Medical. 2010; 25: 42-46.
- Diallo MS, Youssouf O, Yaogo A, et al. Evaluation of Hepatic Fibrosis and Hepatic Steatosis by Pulse Elastography (FIBROSCAN/CAP) in Asymptomatic Patients about 170 Cases at the Donka CHU National Hospital in Open Journal of Gastroenterology. 2024; 14: 125-138.
- Maiga MY, Dembelé M, Diallo F, et al. Diagnostic value of upper digestive endoscopy in cirrhosis. Acta Endoscopica. 2002; 32: 211-215.
- N’ko Profile of liver pathology. Diagnostic by ultrasound in Yaoundé (Cameroon) Ann Radiol. 199; 34: 172-175.
- Rimola A, Garcia Tsao G, Navasa M, et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus International Ascites Club. J Hepatol. 2000; 32: 142-53.
- Sheer TA, Runyon Spontaneous bacterial Peritonitis. Dig Dis. 2005; 23: 39-46.
- Karoui S, Hamzaoui S, Sahli F, et al. Mortality in cirrhosis: prevalence, causes and predictive factors. Tunis Med. 2002; 80: 21-25.