Colonoscopy in Ido-Ekiti, Nigeria: A Four-Year Review
Author'(s): Oguntoye Oluwatosin Oluwagbenga1, Yusuf Musah1, Olowoyo Paul1, Erinomo Olagoke2, Omoseebi Oladipo2, Soje Michael Osisiogu1, Oguntoye Oluwafunmilayo Adenike3, Oguntade Hameed Banjo3, Ariyo Olumuyiwa Elijah3 and Atolani Segun Alex3
1Department of Internal Medicine, Federal Teaching Hospital Ido-Ekiti and Afe Babalola University Ado-Ekiti, Nigeria.
2Department of Morbid Anatomy, Federal Teaching Hospital Ido-Ekiti and Afe Babalola University Ado-Ekiti, Nigeria.
3Department of Internal Medicine, Federal Teaching Hospital Ido-Ekiti, Nigeria.
*Correspondence:
Dr. Oguntoye Oluwatosin Oluwagbenga, MBBS (Ibadan), FWACP (Gastroenterol), Lecturer and Consultant Physician / Gastroenterologist and Hepatologist, Department of Internal Medicine, Federal Teaching Hospital Ido-Ekiti and Afe Babalola University Ado-Ekiti, Ekiti State, Nigeria, Tel: +2348086638538.
Received: 30 March 2020 Accepted: 21 April 2020
Citation: Oguntoye Oluwatosin Oluwagbenga, Yusuf Musah, Olowoyo Paul, et al. Colonoscopy in Ido-Ekiti, Nigeria: A Four-Year Review. Gastroint Hepatol Dig Dis. 2020; 3(1): 1-8.
Abstract
Background: Lower gastrointestinal complaints are common, and the underlying diseases varies widely. Colonoscopy is the gold standard investigation for lower gastrointestinal symptoms. It helps in the proper diagnosis and the appropriate management of the underlying lesions.
Aim: To determine the characteristics of the patients undergoing colonoscopy in a rural community in southwestern Nigeria.
Methods: This was a retrospective cohort study of all patients who had colonoscopy between February 2016 and February 2020 (a period of 4 years). The Age, Gender, Indication and the Endoscopy findings were obtained from the Endoscopy Register. A total of 35 colonoscopies had been performed over the period. The data obtained was analyzed using the Statistical Package for the Social Sciences (SPSS) version 21.0. Descriptive statistics used
included frequency tables, means and standard deviations.
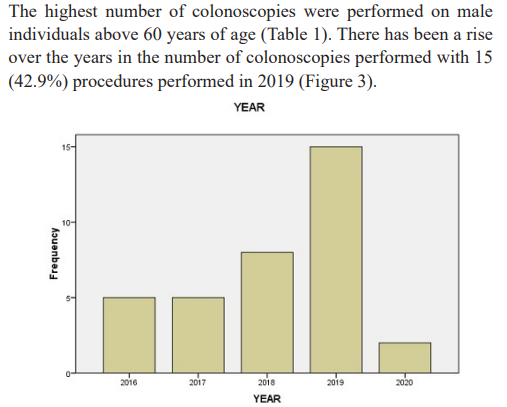
Results: A total number of 35 colonoscopies were performed during the period under review, out of which 25 (71.4%) were males and 10 (28.6%) were females with a male to female ratio of 2.5 to 1. The age range of the patients was 35 to 86 years with a mean (±SD) of 62.6 (±15.07) and median of 63.0 years. The highest number of colonoscopies were performed on male individuals above 60 years of age. Symptoms of lower gastrointestinal
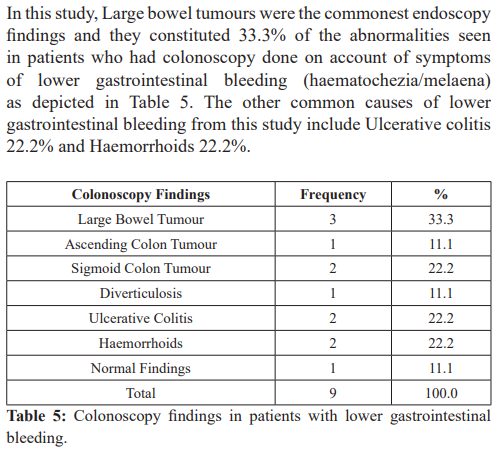
bleeding (haematochezia/melaena) constitute the commonest indication for colonoscopy (25.7%), followed by a clinical suspicion of a rectal tumour 14.3% and documented abnormality on an imaging study 11.4%. The caecal intubation rate from this study is 88.6%.
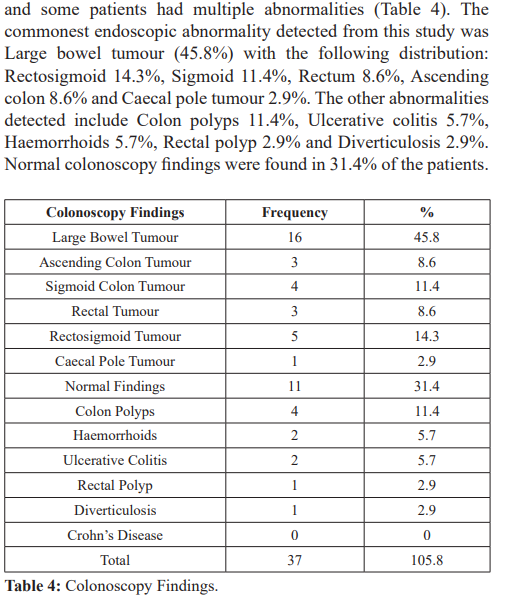
The commonest endoscopic abnormality detected from this study was Large bowel tumour (45.8%) with the following distribution: Rectosigmoid 14.3%, Sigmoid 11.4%, Rectum 8.6%, Ascending colon 8.6% and Caecal pole tumour 2.9%. The other abnormalities detected include Colon polyps 11.4%, Ulcerative colitis 5.7%, Haemorrhoids 5.7%, Rectal polyp 2.9% and Diverticulosis 2.9%. Normal colonoscopy findings were found in 31.4% of the patients.
Conclusion: The commonest indication for colonoscopy in this study was lower gastrointestinal bleeding while the commonest endoscopic diagnosis was colorectal cancer. Colon cancers were the most commonly seen endoscopic abnormality in the patients with lower gastrointestinal bleeding. From this study, large bowel tumours therefore were the commonest underlying gastrointestinal pathology of patients’ symptomatology necessitating colonoscopic
evaluation. The findings from this study conducted in a rural community in Nigeria were similar to those conducted in urban communities in the country. Therefore, a national guideline on the endoscopic evaluation of lower gastrointestinal disorders can be universally applied irrespective of the location of practice in Nigeria.
Keywords
Introduction
Colonoscopy is an endoscopic procedure in which a flexible endoscope is introduced through the anus for visual inspection of the entire large bowel; it is advanced through the rectum, sigmoid colon, descending colon, transverse colon, ascending colon and the caecum [1]. Colonoscopy is the gold standard investigation for lower gastrointestinal symptoms [2]. It has the added benefit of enabling mucosal biopsy sampling and brush cytology for histopathologic diagnosis and therapeutic interventions can also be carried out [3].
Indications for colonoscopy include: Screening at risk individuals for colorectal cancer [4,5]; Diagnostic evaluation for signs or symptoms suggestive of lower gastrointestinal (GI) disease (such as constipation, diarrhea, abdominal pain, altered bowel habit, haematochezia or melaena); Surveillance, evaluation, and follow- up of colorectal cancer (such as family history of colorectal cancer, familial adenomatous polyposis or hereditary non-polyposis colorectal cancer); Biopsy for suspected lower GI disease (such as in inflammatory bowel disease); and Therapeutic intervention (such as control of hemorrhage, dilatation or stenting of stricture, ablation of neoplasms or removal of polyps) [6,7].
The symptoms of lower gastrointestinal diseases are common and accurate diagnosis is usually made after clinical, laboratory and imaging assessment [1]. In resource poor countries such as in Nigeria, diagnosis is often based on clinical assessment [8,9]. Accurate localization and diagnosis of gastrointestinal pathologies is necessary for proper evaluation, treatment and follow-up of patients. The importance of colonoscopy in patient management thus cannot be overemphasized.
Many studies have been published in the literature internationally on the findings at colonoscopy in patients presenting with symptoms of lower gastrointestinal diseases [10-13]. Some of the findings include colorectal cancers, colitis, proctitis, colon polyps, rectal polyps, diverticular disease, ulcerative colitis, crohn’s disease, vascular malformations and haemorrhoids with varying prevalences in different study populations [10-13]. Many studies have also reported Normal findings at colonoscopy despite the patients having lower gastrointestinal symptoms [10,11,13].
Studies conducted in Nigeria have also shown similar findings with varying prevalences [8,9,14,15,16]. There is however paucity of data on the pattern of endoscopy findings in patients undergoing colonoscopy in the rural environments in Nigeria. This is because colonoscopy services are not available in most rural communities in Nigeria and the few published studies were conducted in urban communities where colonoscopy is available. This is sadly the trend across the country and also in other developing countries [8,17,18].
The aim of this study is to determine the characteristics of the patients undergoing colonoscopy in a rural community in south- western Nigeria. The objective of this study is to determine the indications for and the findings at colonoscopy in our institution which is a government-owned tertiary hospital in Ido-Ekiti, Ekiti state, Nigeria. This study is an audit of our colonoscopic practice, which is taking place for the first time, since February 2016 when we first started offering colonoscopy services.
This study will provide much needed scientific data on the subject among rural dwellers and it will contribute to the pool of the already available data which can be used to build a national database on colonoscopy findings across the different communities in Nigeria. This can then form a template upon which more extensive research can be carried out in our population and can also be used for the development of a national colonoscopy guideline. Knowledge of the common indications for and findings at colonoscopy in our environment can also be useful for institutional policy making and health planning; improvement in the reporting of colonoscopy findings and overall colonoscopy service delivery; as well as improvement in patient management and outcome.
Methods
Study design
This was a retrospective cohort study of all patients who had colonoscopy between February 2016 and February 2020 (a period of 4 years) at the Federal Teaching Hospital, Ido-Ekiti, Ekiti state in south-western Nigeria.
Study location
The study was conducted at the Federal Teaching Hospital, Ido- Ekiti, Ekiti state in south-western Nigeria. Ido-Ekiti is one of the rural communities located in Ido-Osi local government area of Ekiti state which has an estimated population of 159,114 people. The Federal Teaching Hospital, Ido-Ekiti is a tertiary health institution that started providing endoscopy services for patients since February 2016 till date.
The colonoscopy procedures were carried out in the endoscopy suite which is located within the Operating Theatre complex of the Federal Teaching Hospital, Ido-Ekiti. The Gastroenterology unit of Internal Medicine Department is in charge of all gastrointestinal endoscopies in the institution and all such procedures are performed by us. There are two gastroenterologists in the hospital and four endoscopy nurses.
Patient population
The Gastroenterology unit receives referrals for endoscopies from the hospital’s outpatient clinics, wards, emergency department, other various specialized units within Internal medicine department as well as from other departments in the hospital such as Obstetrics and Gynaecology and General Surgery. The hospital runs an “open access” endoscopy policy whereby the patients are directly referred to the endoscopy room by their physicians based on their perceived need without prior review by a gastroenterologist. Nevertheless, the patients would be properly prepared for the procedure following standard protocols.
Procedure
The patients presenting for colonoscopy would have been booked and undergone adequate bowel preparation which commences usually 3 days before the procedure. A combination of dietary modifications, liberal fluid intake, two laxatives (Castor oil 15mls and Bisacodyl 20mg twice daily) and a bowel cleansing agent (such as MOVICOL®, PICOLAX®) were used for the bowel preparation. The patients were also fasted for a minimum of 8hours before the procedure. The procedure was explained to them and a written informed consent obtained before the procedure. The patients’ socio-demographics and indication for OGD were documented in the endoscopy register.
Patients were placed on a dextrose containing intravenous fluid and an anti-motility agent (Hyoscine butyl bromide 20 - 40mg) administered before the procedure. Patients were also administered a combination of Pentazocine 30mg and Diazepam 10mg with the doses titrated for optimal conscious sedation. No general anaesthesia was done for any of our patients. Continuous monitoring of the patient was done by a nurse throughout the procedure.
Patient was placed in the left lateral decubitus position. A systematic examination was done by an endoscopists (a Gastroenterologist). The colonoscopy was done using a forward viewing Olympus CV- 170 series video scope (Olympus America Incorporated) according to standard procedures. Endoscopic images of important views were taken for documentation and for further review after the procedure. Mucosal biopsies were taken as indicated and the specimens were transported in a formalin solution for histopathological evaluation. There was observation of the patient for a minimum period of 30minutes after the procedure and subsequently discharged home or taken to the wards once the vital signs were satisfactory. The colonoscopy findings were documented in the endoscopy register and an endoscopy report was issued to the patients.
Data collection
The endoscopy room register was used to obtain the data for a four-year period; February 2016 to February 2020. The following information was obtained from the register: Age, Gender, Indication and the Colonoscopy findings. A total of 35 colonoscopies had been performed over this period.
Ethical Approval
Ethical approval was obtained from the Ethics and Research Committee of the institution.
Data Analysis
The data obtained was analyzed using the Statistical Package for the Social Sciences (SPSS) version 21.0 computer software package (SPSS Chicago Inc. IL U.S.A). Descriptive statistics used included frequency tables, means and standard deviations.
Results
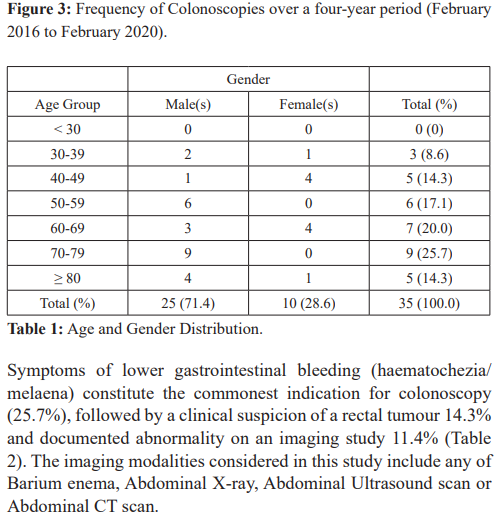
A total number of 35 colonoscopies were performed during the period under review (February 2016 to February 2020 – a four- year period), out of which 25 (71.4%) were males and 10 (28.6%) were females with a male to female ratio of 2.5 to 1 (Figure 1). The age range of the patients was 35 to 86 years with a mean (±SD) of 62.6 (±15.07) and median of 63.0 years (Figure 2).
Discussion
The symptoms of lower gastrointestinal disorders are common and colonoscopy plays a major role in the diagnosis of the underlying pathology [2,3]. It is therefore expected that a large number of colonoscopies would be performed as a result. In this study, the total number of colonoscopy procedures performed over a 4-year period was quite low when compared with similar studies in Nigeria but which were conducted in urban communities [8,9,14- 16].
Although there was an increase in the number of colonoscopy procedures performed from 5 (14.3%) in 2016 to 15 (42.9%) in 2020, the number is still too small. This is due to a number of factors which include the fact that our hospital is located in a rural environment which has a small population compared to an urban community. Also, the low educational status of the populace and their preference of traditional remedies to orthodox treatment are contributory. The poor socio-economic status of the residents, whom are mostly retirees and elderly, also prevents them from patronizing the hospital considering the cost of services and treatment which they cannot afford. Majority of the residents are self-employed; artisans, farmers and traders and they are not registered under the National Health Insurance Scheme which could have considerably reduced the cost of accessing colonoscopy service in the hospital.
This study found a male: female ratio of 2.5:1 among patients who had colonoscopy. This is similar to the findings of Ismaila et al.
[8] in Jos, Olokoba et al. [15] in Ilorin, Alatise et al. [14] in Ile- Ife, Osinowo et al. [19] in Lagos and Ray-Offor et al. [20] in Port Harcourt. The conservative nature of women might explain the gender difference.
In this study, the mean (± SD) age of the patients was 62.6 (± 15.07) years which is higher than what was reported by Ismaila et al. [8] (43.5 years), Osinowo et al. [19] (46.9 years) and Olokoba et al. [15] (53.4 years). The mean age reported by Ray-Offor et al.
[20] (54.8 years) and Akere et al. [16] in Ibadan (57.9 years) was also less compared with our study. Sixty percent of the patients in our study were above 60 years of age; reflecting the age when majority of our population would likely require a colonoscopy. The age difference may be because the setting of this study is a rural community with a lot of retirees and elderly individuals unlike the other studies which were conducted in urban communities with much younger population.
The commonest indication for colonoscopy from this study was lower gastrointestinal bleeding (25.7%) followed by suspected rectal tumour (14.3%). Olokoba et al. [15] also reported that the commonest indications for colonoscopy in their study were rectal bleeding, suspected colorectal cancer and an unexplained change in bowel habit. A similar study by Alatise et al. [14] in Ile-Ife also reported lower gastrointestinal bleeding as the commonest indication for colonoscopy followed by change in bowel habit. Studies across the world also showed that lower gastrointestinal bleeding is the commonest indication for colonoscopy in the works carried out by Berkowitz and Kaplan [21] in South Africa, Sahu et al. [22] in India and Kassa [17] in Ethiopia.
Screening colonoscopy was the indication for colonoscopy in 2.9% of the patients in our study which is quite low. Similarly, Akere et al. [16] and Osinowo et al. [19] reported that 3.2% and 4% respectively of the patients in their study had screening colonoscopy. This low screening rates is a reflection of a weak national colorectal screening programme and poor public awareness about colorectal cancer and its prevention. It will therefore not be surprising if the incidence of colorectal cancer in the populace continues to rise.
The commonest endoscopic abnormality in this study was colorectal tumour (45.8%) and majority of them presented for colonoscopy on account of lower gastrointestinal bleeding. Olokoba et al. [15] in Ilorin and Lee et al. [23] in Jamaica also reported colorectal cancers as the most common pathology at colonoscopy. In contrast to our finding, Akere et al. [16] in Ibadan, Ray-Offor et al. [20] in Port Harcourt and Mahomed et al. [12] in South Africa all reported colonic polyps as the most common pathology at colonoscopy while Ismaila et al. [8] in Jos and Alatise et al. [14] in Ile-Ife, reported hemorrhoids as the most common pathology at colonoscopy. Alatise et al. [14] however also reported in addition that the second most commonly found colonoscopic abnormality in their study was colorectal cancer. In other parts of the world, Dakubo et al. [13] in Ghana, Cahyono et al. [10] in Indonesia, and Al-Shamali et al. [11] in Saudi Arabia, reported hemorrhoids, colorectal cancer, and inflammatory bowel disease, respectively as the most common diagnosis at colonoscopy. Reasons for varying findings at colonoscopy may be explained by differences in lifestyle, race, geographic locations, diets, behavioral, and environmental factors as well as the experience of the colonoscopist.
Colorectal cancer is a major cause of morbidity and mortality all over the world and it is the most common type of gastrointestinal cancer [24]. Studies have shown that colorectal cancer accounts for 10-56% of all gastrointestinal malignancies in Nigeria [25-27]. and the lifetime incidence for patients at average risk is 5%, with 90% of cases occurring after the age of 50 years [28]. In our study, 75% of the patients with colorectal cancer were above 50 years.
Symptoms of colorectal cancer include haematochezia, melaena, unexplained weight loss, fatigue, constipation and change in bowel habits among others. These symptoms were observed in our study population necessitating their presentation for colonoscopy. Individuals presenting with any of these symptoms should undergo a thorough medical evaluation including a colonoscopy as they may be the features of colorectal cancer. Colorectal cancer survival is highly dependent upon stage of disease at diagnosis, the earlier the stage at diagnosis, the higher the chance of survival. It is estimated that 394,000 deaths from colorectal cancer still occur worldwide annually [24]. Invasive colorectal cancer is a preventable disease which can be achieved through early cancer detection by widely applied screening programs such as colonoscopy for at risk individuals and surgical removal if the cancer is detected early [29-31].
In this study, the prevalence of ulcerative colitis is 5.7% and there was no patient with crohn’s disease. Ulcerative colitis is reportedly rare in Black Africans [32,33] and indeed Nigerians [34,35] compared to Western populations [36,7]. There is no national data on the prevalence of ulcerative colitis in Nigeria; only few reports are available, mainly as case reports and case series [38,39]. Even though ulcerative colitis is rare in our environment, it is important for physicians to have a high index of suspicion for this condition particularly in young individuals presenting with recurrent haematochezia such as in our patients.
Our study showed a polyp detection rate of 14.3% which is similar to what was reported by Olokoba et al. [15] (15.5%) but less than what was reported by Akere et al. [16] (23.2%) and Ray-Offor et al. [20] (53.7%). Alatise et al., [14] Osinowo et al. [19] and Ismaila et al. [8] reported lower values of 10.3%, 7.4% and 6.9% respectively.
The caecal intubation rate from our study was 88.6% which is lower than the recommended minimum of 90% [2]. This can be explained by few instances of sub-optimal bowel preparation and poor patients’ tolerance of the procedure; since the procedures were performed under conscious sedation. Osinowo et al. [19], Akere et al. [40] and Ray-offor et al. [40] reported caecal intubation rates of 80.2%, 89.2% and 98.5% respectively. Studies have shown that some of the factors that affect caecal intubation rates are age, gender, quality of bowel preparation, experience of the colonoscopist, procedure volume, and certain diseases of the colon such as diverticular disease and inflammatory bowel disease [41,42].
Our study has shown an overall diagnostic yield of 68.6% with 31.4% having normal colonoscopic findings. The diagnostic yield from our study was higher than that of Osinowo et al. [19] who reported 55.9% but lower than that of Alatise et al., [14] Akere et al., [16] Ismaila et al. [8] and Olokoba et al. [15] who reported diagnostic yields of 70.9%, 74%, 79% and 79.6% respectively. Differences in indications, as well as the spectrum of colonic diseases, inclusion criteria and sample size are some of the factors that can determine the diagnostic yield following colonoscopy. Studies have shown that the highest diagnostic yield is found in patients having lower GI bleeding, mass lesions and polyps as demonstrated by Morini et al., [43] Kassa [17], Lee et al., [23] and Rex [44] in their work.
Limitations of the study
- The total number of the colonoscopies performed over the 4-year period under review is relatively very small, a larger volume of the procedure would have been better.
- The report of the histological findings of mucosal sampling was not documented in the Endoscopy register and thus was not included in this study. The hospital does not have Electronic Medical Record and such reports can only be retrieved by searching through the individual case files of the patients which is outside the scope of this study.
Conclusion
The commonest indication for colonoscopy in this study was lower gastrointestinal bleeding while the commonest endoscopic diagnosis was colorectal cancer. Colon cancers were the most commonly seen endoscopic abnormality in patients with lower gastrointestinal bleeding. From this study, Large bowel tumours therefore were the commonest underlying gastrointestinal pathology of patients’ symptomatology necessitating colonoscopic evaluation. The findings from this study conducted in a rural community in Nigeria were similar to those conducted in urban communities in the country; suggesting that place of domicile or environmental factors does not affect the pattern of symptomatology, clinical presentation or the colonoscopy findings of individuals, which further suggests that the other risk factors or aetiology of the underlying gastrointestinal pathologies are similar in both rural and urban communities. Therefore, a national guideline on the endoscopic evaluation of lower gastrointestinal disorders can be universally applied irrespective of the location of practice in Nigeria.
Recommendations
- Health education and public enlightenment about avoidance of the risk factors for colorectal cancers is important in reducing its incidence in the general population thereby reducing the morbidity and mortality associated with it. Such risk factors include obesity, cigarette smoking, excessive alcohol consumption, consumption of smoked food items and consumption of red Consumption of vegetables and fruits should be encouraged since they reduce the risk of colorectal cancers.
- There is a need to have and implement a national guideline in Nigeria for colorectal cancer screening in order to aid early cancer detection and early removal of pre-malignant lesions identified during routine screening Early detection and prompt intervention remain the only ways the morbidity and mortality associated with this debilitating condition can be reduced since colorectal cancer is curable when detected early.
- Government should ensure universal health insurance coverage for the populace, which should cover the cost of lower gastrointestinal endoscopy procedures so that more patients with the indications can benefit from the procedure. This would improve overall patient care, there would be increase in the volume of procedures performed, which would improve the skills of the endoscopists and enhance better training of Resident doctors.
- Government should also make colonoscopy services available in more health institutions across the country including rural communities to facilitate patients’ access to care. Facilities for Therapeutic colonoscopy should also be provided in the various institutions.
- The benefits of Electronic Medical Records (EMR) cannot be overemphasized; this should be ensured in our hospital and other health institutions for easy access to patients’ medical records, safe and durable data storage, easy follow-up of cases, easy referral of cases and for easy data acquisition which would greatly enhance medical research.
- Regular Clinical Audit should be performed by each specialized unit and compare practice with international standards; this would greatly improve overall performance and patient care.
Acknowledgement
Special thanks to the Endoscopy Nurses, House Officers and Resident Doctors in the Gastroenterology unit of the Department of Internal Medicine for their support in making this publication a reality.
References
- https://emedicine.medscape.com/article/1819350-overview#a2. Updated: June 07, 2018. Assessed: April 06,
- Rex DK, Bond JH, Winawer S, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: Recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J 2002; 97: 1296-1308.
- Grassini M, Verna C, Niola P, et Appropriateness of colonoscopy: Diagnostic yield and safety in guidelines. World J Gastroenterol. 2007; 13: 1816-1819.
- Davila RE, Rajan E, Baron TH, et ASGE guideline: Colorectal cancer screening and surveillance. Gastrointest Endosc. 2006; 63: 546-557.
- Rex DK, Johnson DA, Lieberman DA, et Colorectal Cancer Prevention 2000: Screening recommendations of the American College of Gastroenterology. American College of Gastroenterology. Am J Gastroenterol. 2000; 95: 868-877.
- Lieberman DA, De Garmo PL, Fleischer DE, et Patterns of endoscopy use in the United States. Gastroenterology. 2000; 118: 619-624.
- Gonvers JJ, Froehlich F, Burnand B, et al. The European EPAGE Study Group. A European view of appropriateness and diagnostic yield of colonoscopy: A multicentre study. 2002; 122: A574.
- Ismaila BO, Misauno MO. Colonoscopy in a tertiary hospital in J Med Trop. 2011; 13: 172-174.
- Onyekwere CA, Odiagah JN, Ogunleye OO, et Colonoscopy Practice in Lagos, Nigeria: A Report of an Audit. Diagnostic and Therapeutic Endoscopy. Volume2013, Article ID798651, 6pages.
- Cahyono SB, Bayupurnama P, Ratnasari N, et al. Evaluating indications and diagnostic yield of colonoscopy in Sardjito general J Int Med Acta Int. 2014; 4: 51-56.
- Al-Shamali MA, Kalaoui M, Hasan F, et al. Colonoscopy: Evaluating indications and diagnostic yield. Ann Saudi Med. 2001; 21: 304-307.
- Mahomed AD, Cremona E, Fourie C, et A clinical audit of colonoscopy in a gastroenterology unit at a tertiary teaching hospital in South Africa. South Afr Gastroenterol Rev. 2012; 10: 9-15.
- Dakubo JC, Seshie B, Ankrah LN. Utilization and diagnostic yield of large bowel endoscopy at Korle-Bu Teaching J Med Biomed Sci. 2014; 3: 6-13.
- Alatise OI, Arigbabu AO, Agbakwuru EA, et al. Spectrum of colonoscopy findings in Ile-Ife Nigeria. Niger Postgrad Med 2012; 19: 219-224.
- Olokoba AB, Obateru OA, Bojuwoye MO, et Indications and findings at colonoscopy in Ilorin, Nigeria. Niger Med J. 2013; 54: 111-114.
- Akere A, Oke TO, Otegbayo JA. Colonoscopy at a tertiary healthcare facility in Southwest Nigeria: Spectrum of indications and colonic abnormalities. Ann Afr Med. 2016; 15: 109-113.
- Kassa Colonoscopy in the investigation of colonic diseases. East Afr Med J. 1996; 73: 741-745.
- Ogutu EO, Okoth FA, Lule Colonoscopic findings in Kenyan African patients. East Afr Med J. 1998; 75: 540-543.
- Osinowo A, Lawal O, Lesi OA, et al. Audit of colonoscopy practice in Lagos University Teaching Hospital. J Clin Sci. 2016; 13: 29-33.
- Ray-Offor E, Abdulkareem F. Screening colonoscopy in Port Harcourt, Nigeria. Gastroenterology Insights. 2019; 10: 7987.
- Berkowitz I, Kaplan Indications for colonoscopy. An analysis based on indications and diagnostic yield. S Afr Med J. 1993; 83: 245-248.
- Sahu SK, Husain M, Sachan Clinical spectrum and diagnostic yield of lower gastrointestinal endoscopy at a tertiary centre. Internet J Surg. 2009:18: 1-5.
- Lee MG, Martin A, Terry Colonoscopy in Jamaica- a 12 year experience. West Indian Med J. 1989; 38: 213-216.
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010; 127: 2893-2917.
- Elesha SO, Owonikoko Colorectal neoplasms. A retrospective study. East Afr Med J. 1998; 75: 718-723.
- Ohanaka CE, Ofoegbu The pattern of surgical cancers in Nigeria: the Benin experience. Trop. Doct. 2002; 32:38-39.
- Abdulkareem FB, Abudu EK, Awolola NA, et al. Colorectal carcinoma in Lagos and Sagamu, Southwest A histopathological review. World J Gastroenterol. 2008; 14: 6531-6535.
- Smith RA, Cokkinides V, Brooks D, et Cancer screening in the United States, 2010: a review of current American Cancer Society guidelines and issues incancer screening. CA Cancer J Clin. 2010; 60: 99-119.
- Douglas KR, David AJ, Joseph CA, et American College of Gastroenterology Guidelines for colorectal cancer screening 2008. Am J Gastroenterol. 2009; 104: 739-750.
- Raquel ED, Elizabeth R, Todd HB, et al. American Society for Gastrointestinal Endoscopy: colorectal cancer screening and surveillance 2006. Gastrointestinal Endoscopy. 2006; 63: 546-892.
- Bernard L, David AL, Beth M, et Screening and Surveillance for the Early Detection of Colorectal Cancer and Adenomatous Polyps, 2008: A Joint Guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008; 134: 1570-1595.
- Alese OB, Irabor Pyoderma gangrenosum and ulcerative colitis in the tropics. Rev Soc. Bras. Med. Trop. 2008; 41: 6647.
- Mayberry J, Mann R. Inflammatory bowel disease in Sub Saharan Africa: Rarity of diagnosis in patients attending mission Digestion. 1989; 144: 1726.
- Ukwenya AY, Ahmed A, Odigie VI, et al. Inflammatory bowel disease in Nigerians: Still a rare diagnosis? Ann Afr Med. 2011; 10: 175-179.
- Oludara M, Akinola R, Popoola A, et al. Inflammatory Bowel Disease, a Rare or Under Diagnosed Disease in British Journal of Medicine & Medical Research. 2014; 4: 5620-5628.
- Molodecky NA, Soon IS, Rabi DM, et Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142: 46- 54.
- Kaplan GG, Ng Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017; 152: 313-321.
- Alatise OI, Otegbayo JA, Nwosu MN, et Characteristics of inflammatory bowel disease in three tertiary health centers in southern Nigeria. West Afr J Med. 2012; 31: 28-33.
- Obaseki DE, Forae Clinicopathological features of inflammatory bowel disease in Benin City, Nigeria. Int J Adv Med Health Res. 2014; 1: 16-19.
- Akere A, Akande Cecal intubation rate during colonoscopy at a tertiary hospital in South-West Nigeria: How frequent and what affects completion rate? Niger J Clin Pract. 2017; 20: 303-306.
- Church JM. Complete colonoscopy: How often And if not, why not? Am J 1994; 89: 556-560.
- Dafnis G, Granath F, Påhlman L, et Patient factors influencing the completion rate in colonoscopy. Dig Liver Dis. 2005; 37: 113-118.
- Morini S, Hassan C, Meucci G, et Diagnostic yield of open access colonoscopy according to appropriateness. Gastrointest Endosc. 2001; 54: 175-179.
- Rex DK. Colonoscopy: A review of its yield for cancers and adenomas by indication. Am J Gastroenterol. 1995; 90: 353-