Comparison of the Safety and Efficacy of Arterial Compression Tourniquet and Bandaging Used in Patients with Hepatocellular Carcinoma after Transfemoral Arterial Chemoembolization
Author'(s): Jinkun He1, Guihua Huang2* and Yingqiang Zhang1
1Department of Radiology, The Seventh Affiliated Hospital, Sun Yatsen University, Shenzhen, China.
2Department of Gastroenterology, The Seventh Affiliated Hospital,Sun Yat-sen University, Shenzhen, China.
*Correspondence:
Guihua Huang, Department of Gastroenterology, The Seventh Affiliated Hospital, Sun Yat-sen University, 628 Zhenyuan Road,Shenzhen, 518107, P.R. China; E-mail: huangguihua@sysush.com.
Received: 18 Aug 2023; Accepted: 22 Sep 2023; Published: 29 Sep 2023
Citation: Jinkun He, Guihua Huang, Yingqiang Zhang. Comparison of the Safety and Efficacy of Arterial Compression Tourniquet and Bandaging Used in Patients with Hepatocellular Carcinoma after Transfemoral Arterial Chemoembolization. Cancer Sci Res. 2023; 6(1): 1-4.
Abstract
Objective: To compare the safety and efficacy of arterial compression tourniquet with bandaging in patients with hepatocellular carcinoma (HCC) after trans-femoral arterial chemoembolization (f-TACE).
Materials and Methods: Between the January 2020 and December 2022, 80 patients with HCC who received transfemoral TACE in our hospital were retrospectively analyzed. Forty patients used arterial compression tourniquet for hemostasis (group A), while other 40 patients used bandaging for hemostasis (group B). The hemostasis success rate, operation time, time in bed, and the incidence of complications between the two groups were compared. Results: The hemostasis success rate was 100% in both groups, no patients experienced hemorrhage related death. The mean operation time in the Group A was significant shorter than that of Group B (4.2 min vs. 9.3 min, P<0.001). Correspondingly, the mean time in bed was also significant shorter in Group A compared with Group B (6.7 h vs. 20.3 h, P<0.001). The incidence of inguinal hematoma and ecchymosis in the group A and group B were 10%, and 7.5%, (P=0.692); and the incidence of urinary retention was 5% vs. 12.5%, (P=0.432), respectively.
Conclusion: Arterial compression tourniquet is effective for hemostasis in patients with HCC after transfemoral TACE. Compared to bandaging, arterial compression tourniquet can reduces the operate time and time in bed, and in the certain extent it can reduces the incidence rate of complications.
Keywords
Introduction
Hepatocellular carcinoma (HCC), with more than 700,000 new cases per year worldwide, was the third leading cause of cancer-related death [1]. More than a half of patients were diagnosed at unresectable stage HCC and the radical treatments such as liver resection and ablation, were not allowed. Transarterial chemoembolization
(TACE) can effectively control the tumor growth and improve the overall survival, and is the most commonly used treatments for unresectable stage HCC [2,3]. Because the femoral artery has the characteristics of thick, straight and fixed, therefore trans- femoral artery is the preferred puncture route for TACE [4,5]. However, postoperative hemostasis at puncture site of femoral artery has always been a non-negligible problem in the clinical practice. Although the traditional bandaging pressure hemostasis is economical, safe and effective, the longer bed rest time may cause back pain, insomnia, urinary retention and other discomforts
Recently, arterial compression tourniquet, as a safe and effective tool for hemostasis after trans-arterial interventional therapy, was widely used in the clinical practice [6]. However, the safety and efficacy of arterial compression tourniquet versus bandaging is not clear. Recently, the arterial compression hemostats have been used in our department as a tool for compression hemostasis after f-TACE. Therefore, this study retrospectively reviewed the patients who either received arterial compression tourniquet or bandaging for hemostasis after f-TACE. All hemostasis success rate and complications were recorded between the two methods.
Materials and Methods
Patient selection
Between the January 2020 and December 2022, the electronic medical records of patients with newly diagnosed HCC who received f-TACE treatment were reviewed. The diagnosis of HCC was based on Chinese HCC guideline [7].
Inclusion criteria
To exclude bias due to disease, all patients were primary HCC undergoing TACE. (a) age 18-75 years old; (b) physical status ECOG score ≤ 2; if those with liver function Child-Pugh grade C, or those with refractory ascites, or those who cannot take care of their own life, or those have serious hematological system diseases or coagulation disorders, heart, lungs, kidneys and other serious diseases.
In total, 80 patients were included in the present study, of which 40 cases who received arterial compression tourniquet (Work, Hangzhou, China, Shanyou Medical Equipment Co., LTD) for hemostasis and the other 40 cases who received traditional bandaging for hemostasis after f-TACE. All enrolled patients were recorded in detail for general information, physical status, liver and kidney function, presence of hematoma, petechiae and size of petechiae in the postoperative wounds, back pain and urinary retention.
TACE treatment [5]
All patients received trans-femoral artery TACE using Selinger technique. Briefly, a 5-F catheter sheath and 5-Fr Yashiro or RH catheter was introduced into the celiac artery and superior mesenteric artery, and angiography was performed to assess the tumor-feeding artery and the patency of the portal vein. All chemoembolization procedures included superselective catheterization to the tumor- feeding arteries by using a microcatheter. Depending on the tumor size and liver function, 2-20 ml lipiodol plus 20-60 mg epirubicin was mixed and slowly infused into the liver tumor through the microcatheter. Then embolization-using gelfeom was performed. After the operation, the patients were routinely hospitalized for 1-3 days to observe their postoperative conditions and were given hepatoprotective and symptomatic treatments.
Use of Arterial Compression Tourniquet [6]:
Patients was taken in a supine position, then the femoral artery puncture site was identified, the arterial sheath was withdrawn 1-2 cm, and covers the body surface with sterile gauze; rotates the spiral handle clockwise for 1-2 turns, and presses the bionic pressure plate along the direction of groin on the femoral artery puncture site; then yanks the fixation tape around the femur in a smooth manner and adheres to it; rotates the spiral handle clockwise to increase pressure on the hemostasis point through the pressure plate; confirms that the arterial artery has a blood supply to the tumor, then confirms that the arterial arteries have been infiltrated. The pressure on the hemostatic point is increased by turning the spiral handle clockwise to increase the pressure on the hemostatic point through the pressure plate to confirm that the arterial compression hemostat is fixed accurately and stably, if it feels unstable, continue to rotate the spiral handle clockwise to increase the pressure until it is stable; and then the arterial sheath is pulled out, and the spiral handle is adjusted to increase the pressure to the point of visual inspection without oozing of blood, and the patient's looseness and tightness are appropriate without oozing of blood, and the patient's routine braking is appropriate for 6-8 hours after the operation.
Bandaging Compression Hemostasis
Finger pressure on the femoral artery above about 1 cm of puncture point, then the sheath tube is remove, finger pressure, appropriate intensity of the puncture point with blood seepage is appropriate, routine pressure about 10 minutes, and then use bandage roller to pressure the puncture point, bandage to bing and fix, routine postoperative braking for 24 hours. Record the time used to bandage the wounds of the two groups of patients, observe the hemostatic effect of the femoral artery puncture wounds, and on the next day, observe whether the wounds have hematomas, petechiae, whether the lower limbs have any pain, and whether there is any urinary retention.
Statistical analysis
All statistical analyses were performed using SPSS 16.0 software. The patients’ demographics including age, gender, tumor stage, liver function, blood routine and other laboratory test data were statistically described, continuous variables are expressed medians± standard deviation, and compared using student t test. Categorical variables are expressed as frequencies and percentages, and compared using χ2 test. All statistical tests were two-sided, and P< 0.05 was considered statistically significant.
Results
Demographics of all patients are shown in table 1. All characteristics between the two groups were comparable, and there are no significant difference between them in terms of age, gender, tumor stage, liver function, performance status score.
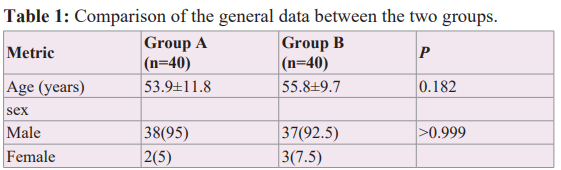
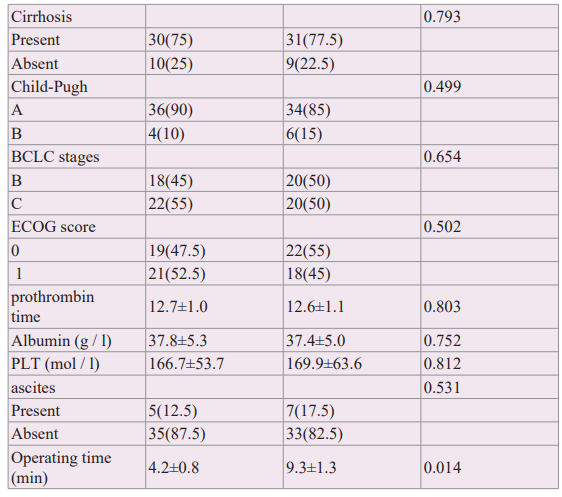
BCLC: Barcelona Clinic Liver Cancer; ECOG: Eastern Cooperative Oncology Group. PLT: Platelet.
All patients had successful hemostasis, and no hemorrhage or death due to bleeding was observed. In the group A, the incidence of inguinal hematoma and ecchymosis in the group B was 4/40=10% and 3/40=7.5%, respectively (P =0.692). In the group A, the incidence of urinary retention was 2/40=5% and 5/40=12.5% in the group B, respectively (P=0.432). No serious complications such as pulmonary embolism, pseudoaneurysm, and lower limb nerve injury were seen.
Discussion
At present, interventional diagnosis and treatment is listed as the third major discipline together with internal medicine and surgery, and more and more diseases can be diagnosed and treated through interventional channels, among which oncological intervention is an important branch of interventional diagnosis and treatment. Transhepatic artery chemoembolization is the most important treatment for unresectable hepatocellular carcinoma, but postoperative femoral artery compression and hemostasis is a problem that should not be neglected in the clinic.
In this study, the case-control study confirmed that the arterial compressor and bandage pressure dressing were comparable in hemostatic effect, and both groups achieved complete hemostasis, and the incidence of postoperative inguinal hematoma and ecchymosis in the two groups were basically comparable. However, the operation time of arterial compressor was significantly less than that of the bandage compression bandage group, because bandage compression bandage routinely requires about 10 minutes of compression after removing the sheath and then giving the bandage compression bandage, while arterial compressor can be used to remove the sheath directly after the bandage compression bandage has been tied, so it can reduce the operation time and save the time for the next surgery. At the same time, we also found that the incidence of urinary retention in the arterial compressor group was slightly lower than that in the bandage compression bandage group, which may be attributed to the fact that the arterial compressor using the compressor is generally subjected to bed braking for about 6-8 hours, whereas the bandage compression bandage is generally subjected to bed braking for 24 hours; the unaccustomed urination in bed or the soreness of the lumbar and back leading to urinary retention; and the fact that due to the reduction of the time spent on bed braking, the risk of pulmonary embolism resulting from the formation of venous thrombosis in the lower limbs can be reduced to some extent. Risk, especially for elderly, tumor patients, it has been pointed out to report that elderly, tumor patients have higher blood viscosity than normal people, and the risk of forming venous thrombosis is increased [8], therefore, reducing the time of bed braking has a certain effect on reducing the formation of lower limb veins. Although no case of pulmonary embolism was encountered in this study group but the author had encountered a case of acute pulmonary embolism caused by lower limb venous thrombosis after TACE in a 70-year- old patient with hepatocellular carcinoma, the patient's preoperative hepatic function Child-Pugh grade A, coagulation function was not abnormal, the next day after removing the bandage and getting out of the bed, he suddenly suffered from chest pain and chest tightness, respiratory distress, oxygen saturation decreased, and finally died.
In conclusion, arterial compression hemostat is a safe and effective tool for compression hemostasis after femoral artery puncture, which has the advantages of fast operation, reduced bed braking time, reduced the incidence of urinary retention in patients to a certain extent, and improved discomfort such as low back pain compared with traditional bandage compression dressing.
References
- Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: systematic analysis for the Global Burden of Disease study Lancet. 2019; 394: 1145-1158.
- Reig M, Alejandro F, Jordi R, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022; 76: 681-693.
- Sieghart W, Hucke F, Peck-R M. Transarterial chemoembolization: modalities, indication, and patient selection. J Hepatol. 2015; 62: 1187-1195.
- Zhang Y, Miao H, Xie W, et al. The PPRD score stratifies patients with hepatocellular carcinoma and portal vein tumor thrombosis treated with sorafenib plus transarterial chemoembolization. Eur Radiol. 2021; 31: 232-243.
- Zhang YQ, Jiang LJ, Wen J, et Comparison of α-fetoprotein criteria and modified response evaluation criteria in solid tumors for the prediction of overall survival of patients with hepatocellular carcinoma after transarterial chemoembolization. J Vasc Interv Radiol. 2018; 29: 1654-1661.
- Zhang Z, Zhong Q, Tan J, et al. Progress on compression haemostasis after radial coronary Chin J Nursing. 2013; 48: 476-478.
- Zhou J, Huichuan S, Zheng W, et al. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (2019 edition). Liver Cancer. 2020; 9: 682-720.
- Mukai M, Oka Mechanism and management of cancer- associated thrombosis. J Cariol. 2018; 72: 89-93.