Concurrent Deep T-Wave Inversions and QT Prolongation with Azithromycin Treatment
Author(s): Melissa Wasilewski MD1, Sara Kwiatkowski DO1 , Kunal Kapoor MD MSc2 and Sumon Roy MD2*
1Department of Internal Medicine, Virginia Commonwealth University, Richmond, VA.
2Division of Cardiology, VCU Pauley Heart Center, Virginia Commonwealth University, Richmond, VA
*Correspondence:
Sumon Roy MD, Department of Cardiovascular Disease, Virginia Commonwealth University, 1201 E Marshall St, Richmond, VA 23298, Phone: 804-828-9726, Fax: 804-828-0395.
Received: 20 Mar 2022; Accepted: 23 Mar 2022; Published: 28 Mar 2022
Citation: Wasilewski M, Kwiatkowski S, Kapoor K, et al. Concurrent Deep T-Wave Inversions and QT Prolongation with Azithromycin Treatment. Cardiol Vasc Res. 2022; 6(2): 1-5.
Abstract
The tendency of macrolide antibiotics to prolong the QT interval in certain patient populations is well documented. In contrast, limited reports exist of medication-induced deep T-wave inversions. We recently encountered a case of azithromycin-induced QT prolongation with concurrent deep TWI, an association that is rarely observed in clinical practice. As similar ECG changes can be seen with life-threatening conditions such as coronary ischemia and cerebral hemorrhage, comprehensive workup to rule out acute pathologies is critical when this pattern is recognized.
Keywords
Introduction
A common adverse effect of azithromycin is QT interval prolongation on electrocardiogram (ECG), predisposing patients to life-threatening ventricular arrhythmias, including torsades de pointes (TdP). Azithromycin is particularly prone to causing QT prolongation in patients who possess other risk factors for arrhythmia, such as age-related conduction disease, electrolyte abnormalities, concurrent use of other QT-prolonging medications, or a history of long-QT syndrome [1]. Certain genetic mutations may further increase this risk by way of specific cardiac channelopathies [2]. As a result, the United States Food and Drug Administration (FDA) advises clinicians to consider the risks of fatal heart arrhythmias when prescribing azithromycin [3].
Medications can cause other disturbances in cardiac rhythm, conduction, and ECG waveforms. For instance, antiarrhythmic drugs, diuretics, digoxin, and psychoactive medications can cause T-wave inversions (TWI) [4]. However, the appearance of deep TWI often portends a grim prognosis. These have been associated with coronary ischemia, cerebral hemorrhage, acute adrenergic stress cardiomyopathy, or post-tachycardia T-wave syndrome, which often develops after ventricular tachycardia [4].
There are limited reports of medication-induced deep TWI. Furthermore, literature describing concurrent QT prolongation and deep TWI is rare. To our knowledge, we present the first case of oral azithromycin-induced concomitant QT prolongation and deep TWI with no identifiable predisposing risk factors, associated genetic mutations, or alternative clinical explanation. Recognition of these potentially life-threatening ECG changes is critical to early decision making. Our case underscores the relevant workup. Furthermore, we suggest a theoretical association between macrolide antibiotics and the appearance of isolated TWI on ECG. If present, providers ought to consider an alternate antibiotic agent.
Case Report
A 60-year-old female with heart failure with mid-range left ventricular ejection fraction (LVEF) of 40-45%, paroxysmal atrial fibrillation, COPD, and tobacco use presented with complaints of progressive dyspnea over the preceding three days. Her symptoms worsened despite using her albuterol nebulizer and inhaler.
On arrival, she was noted to be hypertensive to 230/120 mmHg and was hypoxic with an oxygen saturation of 70-80% despite receiving continuous positive airway pressure therapy en route to the hospital. Laboratory studies revealed normal electrolytes, blood counts, renal function, and hepatic function. Cardiac enzymes were undetectable and B-type natriuretic peptide level was mildly elevated at 234 pg/mL (reference range ≤ 100 pg/mL). Presenting ECG was non-ischemic, showing sinus tachycardia with a heart rate of 125 bpm and a corrected QT interval (QTc) of 460ms (Figure 1). A chest x-ray revealed cardiomegaly with pulmonary edema.
The patient denied significant alcohol or illicit drug use, and she reported compliance with her home medications, including metoprolol succinate 100 mg daily, apixaban 5 mg twice daily, aspirin 81 mg daily, budesonide/formoterol 160 mcg/4.5 mcg twice daily, and an as-needed albuterol inhaler. After an uncomplicated ED course, the patient was admitted to the intensive care unit on bi- level positive airway pressure therapy and intravenous nitroglycerin for management of acute hypoxic respiratory failure secondary to mixed heart failure and chronic obstructive pulmonary disease (COPD) exacerbation. The patient’s condition started to improve within hours of receiving albuterol and ipratropium nebulizers, steroids, and intravenous diuretics.
As an additional precaution, the patient was started on azithromycin for empiric treatment of community-acquired pneumonia, with an initial dose of 500 mg and plans for four subsequent days of 250 mg daily. Soon after starting azithromycin, telemetry revealed new intermittent bradycardia. Upon receiving her second dose, she reported sudden onset of vague, non-cardiac chest pain. Physical exam was unchanged with moderate air entry bilaterally. Laboratory studies showed a potassium of 4.6 mg/dl, magnesium 2.2 mg/dl, and creatinine 0.99 mg/dl. A high-sensitivity troponin was elevated at 0.21 ng/mL (reference range ≤ 0.19) but down- trended and normalized on repeat evaluation. Repeat ECG revealed a corrected QT interval (QTc) of 640ms, prompting immediate discontinuation of azithromycin. Her ECG also showed profoundly deep TWI in V1-V3, and very tall, wide T waves in the inferior and lateral leads (Figure 2).
As azithromycin is not commonly known to evoke deep TWI, these findings were initially concerning for cerebrovascular or cardiovascular pathologies such as intracranial hemorrhage, left main coronary disease, or apical hypertrophy. As such, a comprehensive evaluation ensued. A computed tomography study of the head was unremarkable for acute intracranial pathologies. Echocardiogram was unchanged compared to a prior study, revealing an LVEF of 40-45%, mild concentric left ventricular hypertrophy, septal wall hypokinesis, and concern for moderate pulmonary hypertension. Coronary angiography demonstrated non-obstructive coronary artery disease and mildly elevated left- sided filling pressures.
By the following day, the patient’s chest pain and initial respiratory symptoms completely resolved. Serial ECGs obtained over the remainder of her hospitalization showed further QTc prolongation initially, then progressive improvement while the deep TWI persisted (Figure 3). She was discharged on hospital day 8. EKG at that time showed a QTc of 540ms. Two weeks later, her QTc normalized to 457ms with significant but incomplete resolution of T-wave changes (Figure 4). Genetic testing for QT-prolonging syndromes was negative, and an electrophysiology study did not identify any inducible arrhythmias.

Figure 1: Baseline ECG prior to initiation of azithromycin, showing sinus tachycardia with a heart rate of 125 bpm and a corrected QT interval (QTc) of 460ms.
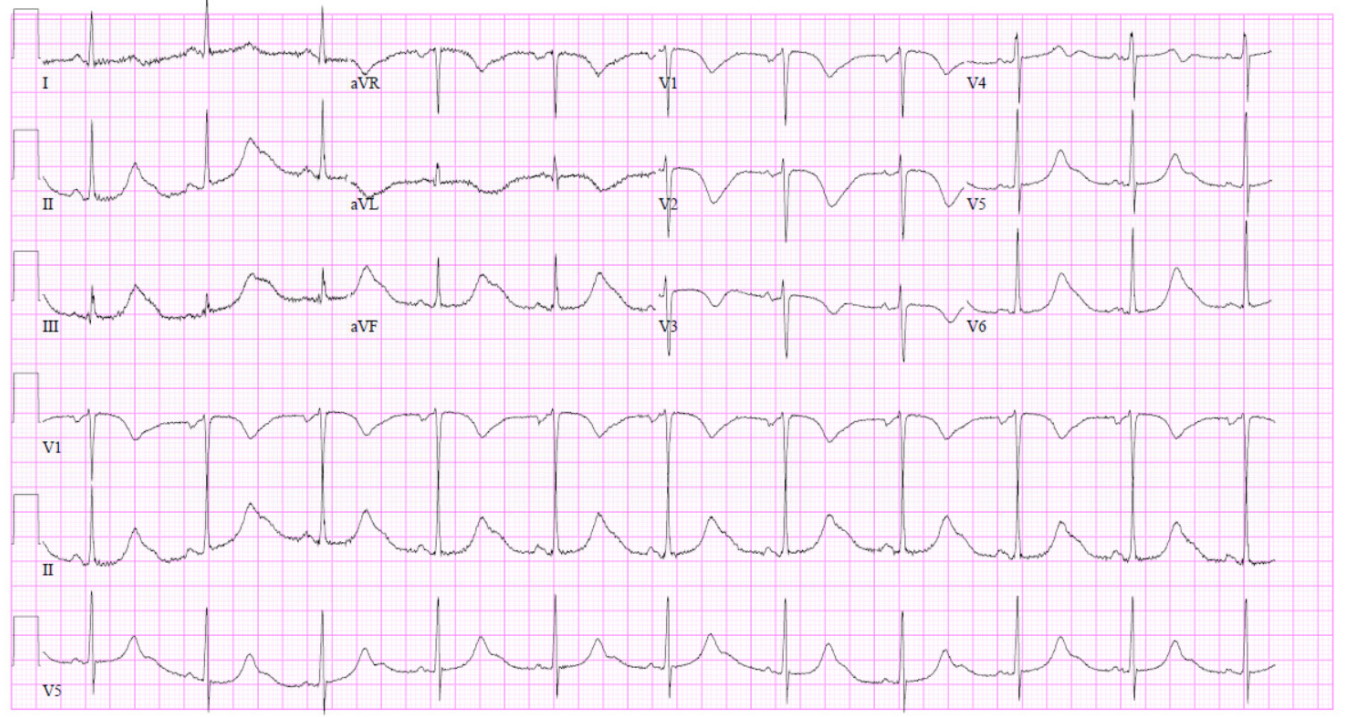
Figure 2: After receiving azithromycin, the patient’s repeat ECG revealed a QTc of 640ms as well as profoundly deep TWI in V1-V3, and very tall, wide T waves in the inferior and lateral leads.
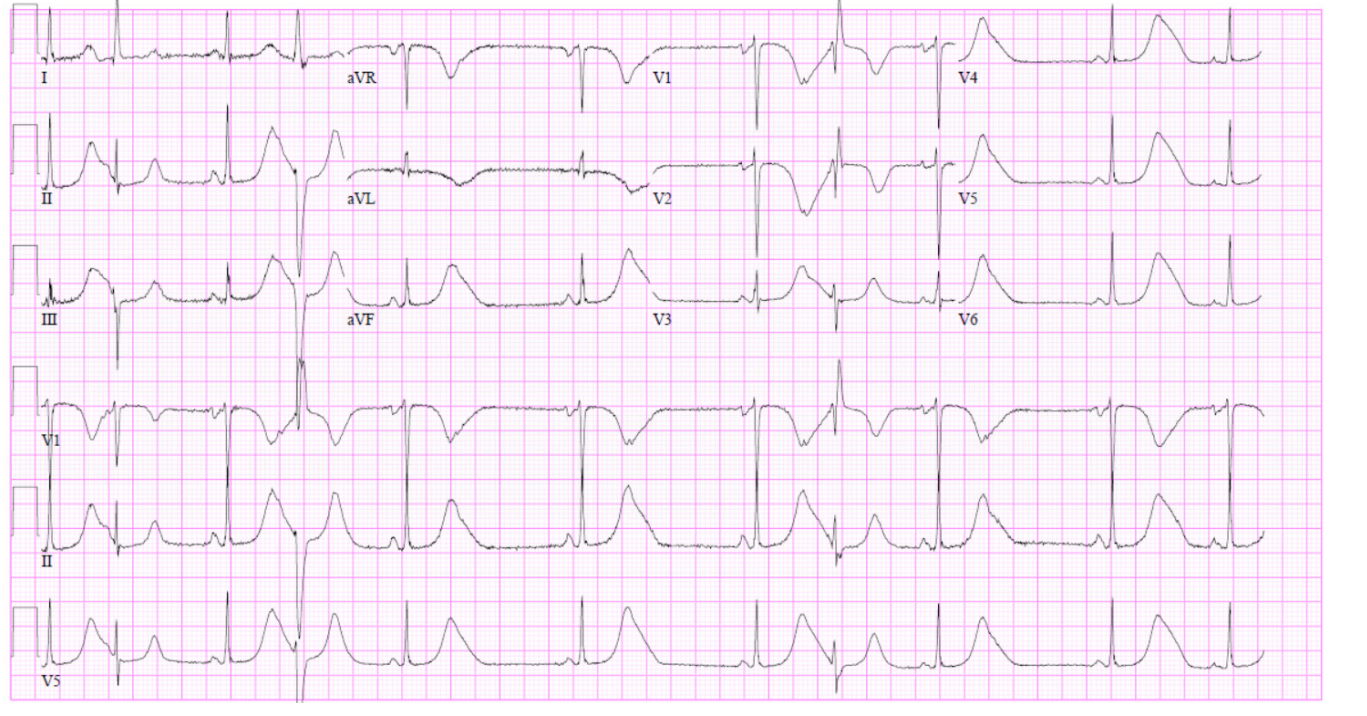
Figure 3: Serial ECGs showed further QTc prolongation initially, then progressive improvement, while the deep TWI persisted
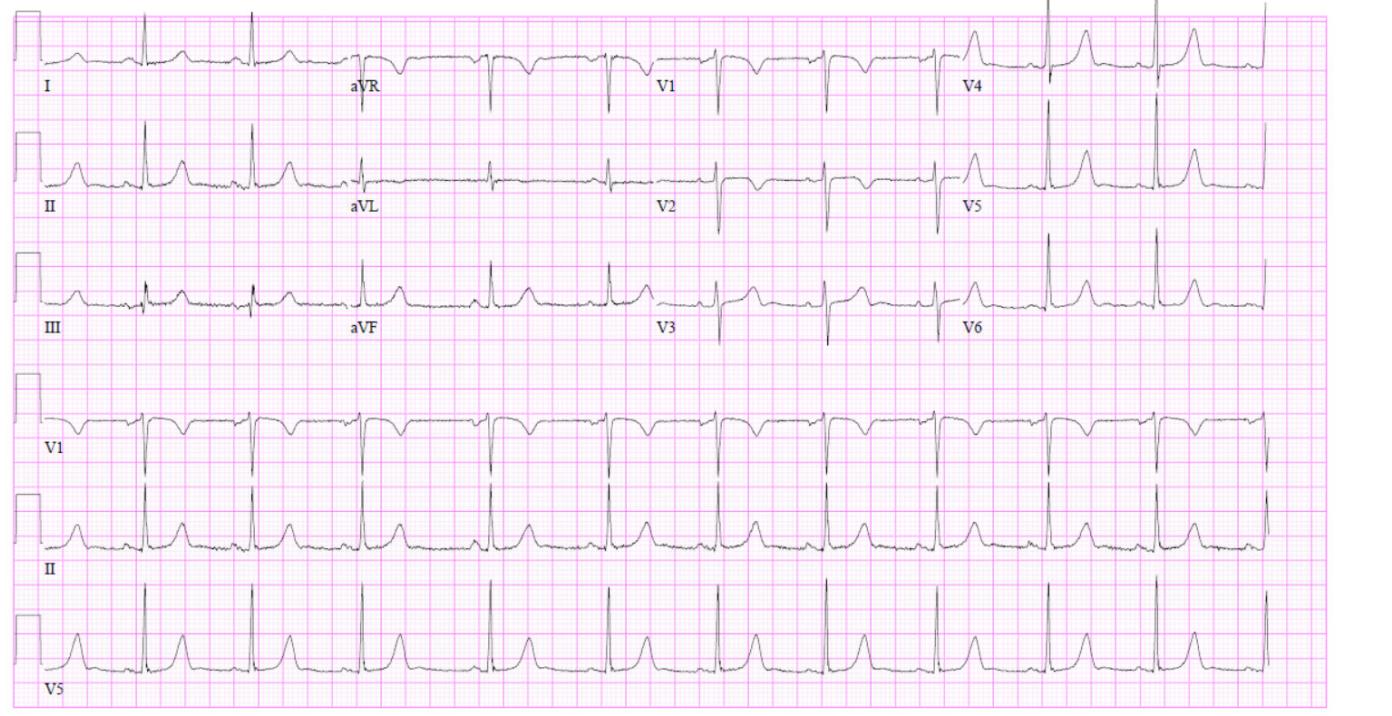
Figure 4: Two weeks later, an ECG obtained in clinic showed a normal QTc of 457ms, with ongoing but resolving T-wave changes
Discussion
This case identifies oral azithromycin as a possible trigger for concurrent QT prolongation and deep TWI, an association that is not commonly recognized in clinical practice. While the pathophysiology behind these abnormality remains unclear, it has been proposed that macrolide antibiotics may cause arrhythmias in patients with certain risk factors such as age-related conduction disease, electrolyte abnormalities, concurrent use of other QT- prolonging medications, or genetic mutations [1,2]. One such case described an elderly male with a previously normal QT interval who was admitted with acute heart failure exacerbation. He developed TWI alongside QT prolongation, which progressed to TdP requiring defibrillation. Once his home fluoxetine and amitriptyline were held, his QT interval reduced with simultaneous resolution of his deep TWI. Genetic testing later resulted positive for a mutation at the SCN5A gene.
A separate case series examining ten patients with concomitant deep TWI and QT prolongation found that left anterior descending artery infarction was the most common etiology associated with these ECG changes [5]. For this reason, identification of concurrent deep TWI and prolonged QT interval on ECG should prompt consideration of an ischemic pathology, even with an established history of recent use of QT-prolongation medications.
While our patient’s course was most suggestive of medication- related QT prolongation, a thorough investigation was undertaken to rule out alternative, critical causes of her acute ECG abnormalities. A non-contrast head CT, plain film of the chest, and coronary angiography were unremarkable. Subsequent genetic tests for mutations associated with QT abnormalities and an electrophysiology study were similarly unrevealing. It was hypothesized that the patient may have been predisposed to the observed ECG findings due to a genetic channelopathy that has yet to be described.
Due to the increased risk of fatal cardiac arrhythmias associated with azithromycin use in high risk patients, the FDA encourages healthcare providers to consider arrhythmia risk before prescribing azithromycin in patients with at least two of the following risk factors: female gender, advanced age, chronic heart disease, concurrent QT prolonging medications, hypokalemia, and bradycardia [6]. Per this criterion, our patient would be considered high risk because of her gender and history of cardiomyopathy. However, while some prospective and observational studies have demonstrated increased risk of pro-arrhythmic events with azithromycin use, others have challenged this association and denied any effect of macrolide antibiotics on QT interval duration [7]. Given this conflicting data, clinicians have the difficult task of screening patients on a case-by-case basis for predisposition to QT prolongation prior to prescribing azithromycin.
Nevertheless, prolongation of the QT interval following onset of macrolide antibiotics should be considered a relative contraindication to continued use. In addition, this case suggests a possible association between macrolide antibiotics and the appearance of TWI on ECG, independent of the QT interval. As such, the development of isolated TWI following initiation of azithromycin therapy should similarly alert providers to consider an alternate antibiotic agent.
References
- Schwartz PJ, WoosleyRL. Predicting the Unpredictable: Drug- Induced QT Prolongation and Torsades de Pointes. J Am Coll Cardiol. 2016; 67: 1639-1650.
- Ping Yang, Hideaki Kanki, Benoit Drolet, et al. Allelic variants in long-QT disease genes in patients with drug-associated torsades de pointes. Circulation. 2002; 105: 1943-1948.
- FDA Drug Safety Communication: Azithromycin (Zithromax or Zmax) and the risk of potentially fatal heart rhythms. 2018.
- Salah Am Said, Rene Bloo, Ramon de Nooijer SA, et al. Cardiac and non-cardiac causes of T-wave inversion in the precordial leads in adult subjects: A Dutch case series and review of the literature. World J Cardiol. 2015; 7: 86-100.
- De Zwaan C, FW Bär, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982; 103: 730-736.
- Jules C Hancox, Mehrul Hasnain, W Victor R Vieweg, et al. Azithromycin, cardiovascular risks, QTc interval prolongation, torsade de pointes, and regulatory issues: A narrative review based on the study of case reports. Ther Adv Infect Dis. 2013; 1: 155-165.
- Howard PA. Azithromycin-induced proarrhythmia and cardiovascular death. Ann Pharmacother. 2013; 47: 1547-1551.