Cryoablation Pulmonary Artery Denervation for the Treatment of Combined Post-Capillary Pulmonary Hypertension Caused Be Left Heart Diseases
Author(s): Rudenko B1, Feshchenko D2, Shukurov F2 and Tkacheva O1
1Pirogov Russian National Research Medical University, Moscow, Russia.
2National Medical Research Center for Therapy and Preventive Medicine, Health ministry of Russia, Moscow, Russia.
*Correspondence:
Boris Rudenko, Pirogov Russian National Research Medical University, Moscow, Russia.
Received: 08 Jun 2024; Accepted: 28 Jul 2024; Published: 05 Aug 2024
Citation: : Rudenko B, Feshchenko D, Shukurov F, et al. Cryoablation Pulmonary Artery Denervation for the Treatment of Combined Post-Capillary Pulmonary Hypertension Caused Be Left Heart Diseases. Cardiol Vasc Res. 2024; 8(2): 1-8.
Abstract
Introduction: Pulmonary artery denervation is rapidly evolving method for treatment of pulmonary hypertension. The purpose of our first-in-man study is to assess the effectiveness of cryoablation for pulmonary artery denervation in patients with pulmonary hypertension secondary to a left heart disease.
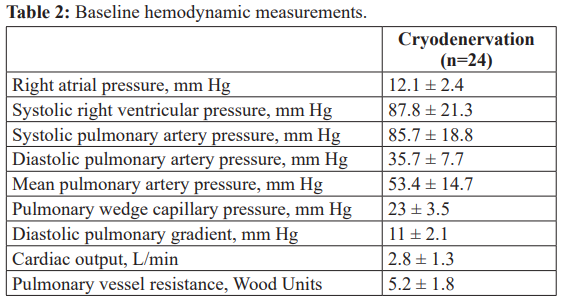
Methods: 24 patients with combined post capillary pulmonary artery hypertension (mPAP ≥25 mm Hg, PCWP >15 mm Hg, PVR >3.0 WU or DPG ≥ 7 mm Hg (or both) were included in the study. The effectiveness of cryodenervation was assessed according to the changes in clinical status, functional capacity and pulmonary hemodynamics during 12-month follow-up.
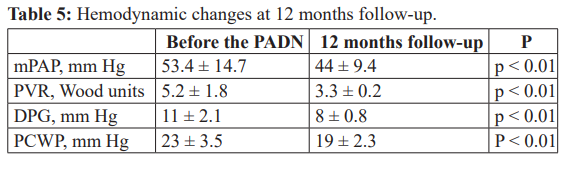
Results: There were no complications during and immediately following the cryoablation procedure. There was significant increase in functional capacity measured by 6MWT: 319 ± 18 m before cryodenervation and 502 ± 22 m (p<0.05) at 12 months follow-up. The N-terminal pro–brain natriuretic peptide value decreased from 2928 ± 223 ng/mL at baseline to 989 ± 67 ng/mL (p<0.05). The right heart catheterization demonstrated the distinctive reduction of mean pulmonary artery pressure (mPAP) from 59 ± 6 to 32 ± 4 mm Hg, pulmonary vessel resistance (PVR) from 9,3 ± 2,2 to 3,4 ± 1,5 WU and diastolic pulmonary gradient (DPG) from 11 ± 2.1 to 8 ± 0.8 mm Hg (p<0.05). Also the decrease of pulmonary capillary wedge pressure (PCWP) from 23 ± 3.5 to 19 ± 2.3 mm Hg was also observed (p<0.05).
Conclusions: This is the first clinical study to demonstrate the clinical, functional and hemodynamic benefits of cryoablation procedure in patients with combined postcapillary PAH caused by left heart diseases.
Keywords
Introduction
Pulmonary artery hypertension (PAH) – one of the most negative consequences of different cardiovascular diseases and it’s associated with poor prognosis. The leading causes of cardiovascular death ischemic heart disease, arterial hypertension, pulmonary thromboembolism deteriorate severely with the onset of pulmonary hypertension (the 5-year survival rate is less than 50%) [1]. The
high pulmonary pressure as a result of idiopathic pulmonary artery hypertension (IPAH), chronic obstructive pulmonary disease, structural heart disease is also a life-threatening situation. The main reason of high mortality rate is a rapid progression of heart failure due to a poor compensatory ability of right ventricle and low effectiveness of drug therapy.
The pulmonary hypertension is associated with enhanced sympathetic activity, that has been proven in several experimental studies. In 1980 Juratsch et al. successfully attempted surgical pulmonary denervation and chemical sympathectomy for lowering pulmonary artery pressure caused by distension of the pulmonary artery [2]. Subsequent animal-based experiments [3,4] and the widespread successful use of radiofrequency ablation in patients with cardiac arrhythmias and high arterial blood pressure [5,6] paved the way for this method as a new treatment of pulmonary hypertension.
Clinical studies of pulmonary artery denervation (PADN) technique started in 2012. A single-center PADN-1 study (first- in-man pulmonary artery denervation for treatment of pulmonary artery hypertension) included 21 patients with precapillary type idiopathic pulmonary artery hypertension mean pulmonary artery pressure (mPAP) > 25 mmHg, pulmonary capillary wedge pressure (PCWP) < 15 mmHg, pulmonary vessels resistance (PVR) > 3 WU (Wood Units). This study reported the significant reduction of pulmonary pressure after denervation procedure, carried out by the radiofrequency system with special dedicated circular- tip catheter [7]. The phase II from the PADN-1 study included 66 patients with different types of PAH: precapillary IPAH and postcapillary pulmonary hypertension as well, associated with left ventricular dysfunction (mPAP > 25 mmHg, PCWP > 15 mmHg, PVR > 3 WU). The results of denervation procedure in this study demonstrated the distinctive reduction of mPAP and significant improvement of functional capacity, measured by 6MWD [8]. Despite the initial positive results of PADN in patients with postcapillary PH secondary to left heart failure, the clinical benefit of such interventions remains controversial.
Catheter Cryoablation is new exiting and promising treatment modality to address the issue of pulmonary hypertension. Offering patients, a higher safety profile and less discomfort than radiofrequency ablation, catheter cryoablation is a safe and efficient alternative for clinicians treating different kind of cardiac arrhythmias. The purpose of our study was to assess the safety and effectiveness of Catheter Cryoablation for pulmonary artery denervation procedure (Cryodenervation) in patients with pulmonary hypertension secondary to a left heart disease.
Methods
Patient selection
Patients with left ventricular dysfunction and CHF (chronic heart failure) II-IV functional class, according to NYHA classification, underwent preliminary echocardiographic measurements. Patients with a systolic pulmonary arterial pressure (sPAP) ≥ 30 mm Hg were eligible for consequent right heart catheterization.
Right Heart Catheterization
Right atrial (RA) pressure, right ventricular (RV) pressure, systolic pulmonary artery pressure (sPAP), diastolic pulmonary artery pressure (dPAP), pulmonary capillary wedge pressure (PCWP) were measured, cardiac output (CO) were derived using thermodilution method with a 7-F flow-directed Swan-Ganz catheter. Then mean pulmonary artery pressure (mPAP) = (sPAP- dPAP/3+dPAP), pulmonary vessels resistance (PVR) = (mPAP− PCWP]/CO) and diastolic pulmonary gradient (DPG) = (dPAP− PCWP) were calculated. All measurements and calculations were made before and 12-months after the Cryoablation procedure. 24 patients were enrolled in the study according to inclusion and exclusion criteria.
Inclusion and exclusion criteria
Inclusion criteria: age ≥18 years, mean PAP (mPAP) ≥25 mm Hg, a pulmonary capillary wedge pressure (PCWP) >15 mm Hg, PVR >3.0 WU or DPG ≥ 7 mm Hg (or both); written consent to undergo the procedure. Exclusion criteria: severe renal dysfunction (creatinine clearance <30 ml/min); systemic active infection, cancer, inability to provide consent.
This study was approved by local Ethics Committee of the National Medical Research Center for Therapy and Preventive Medicine.
Assessment of N-terminal pro–B-type natriuretic peptide levels
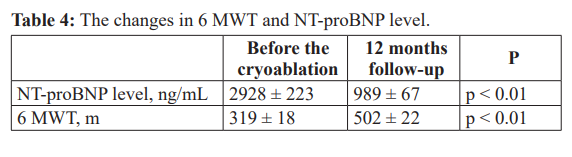
Blood samples (taken in the supine position) were obtained in the morning to measure the levels of N-terminal pro–B-type natriuretic peptide (NT-proBNP) before and 12 months after cryoablation procedure.
Cryoablation Procedure
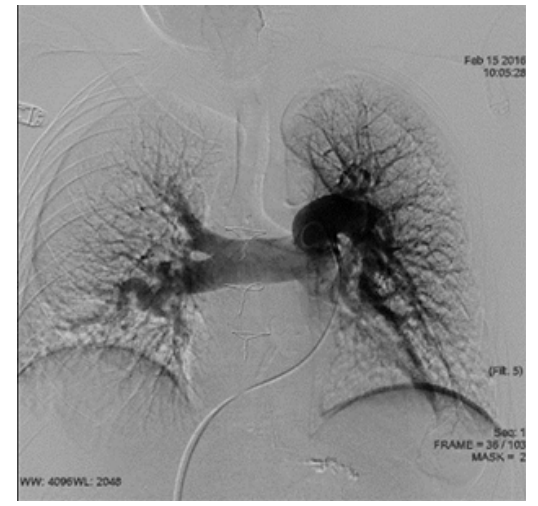
First a 9-Fr long sheath was inserted through the femoral vein and advanced to the main pulmonary artery (MPA). A baseline pulmonary artery angiography was performed using standard 6 Fr pig-tail catheter to identify the PA bifurcation level and the ostiums of the right and left pulmonary arteries (Figure 1). Cryoablation procedure was performed using Cardiac Cryoablation Catheter System (Medtronic, Ireland) which included Cryoconsole and a single-point Freezor™ MAX Cardiac Cryoablation Catheter. After withdrawing the sheath and pushing slightly the cryoablation catheter at the ostium of the left pulmonary artery, the single-point tip of the catheter was placed at the ostium of the left pulmonary artery within 2 mm from its orifice (Figure 2). The tip angulation was formed by steering handle to ensure the proper contact with the vessel wall. Rotating the single-point tip the cryoablation was applied in a circular way around the ostium with the pace of 2 mm. The following ablation parameters were used at each spot: temperature minus 75-80°C, time = 120s. At average, from 7 to 10 ablation spots would be made at the ostium. The same procedure would be performed at the ostium of the right pulmonary artery (Figure 3). The electrocardiogram and hemodynamic pressure were monitored and continuously recorded throughout the procedure, the cryoablation would be stopped automatically in case of the sudden temperature change.
Assessment of functional capacity
Functional capacity was determined before and 12 months after the cryoablation using the standard 6 minutes walking distance test (6MWD) according to the guidelines of the American Thoracic Society protocol. Dyspnea was assessed using the Borg scale at peak exercise during 6MWD test [9]. The functional class of chronic heart failure (CHF) was assessed according to 6MWD measurement and clinical status using NYHA classification [10].
Figure 1: Pulmonary artery angiography.
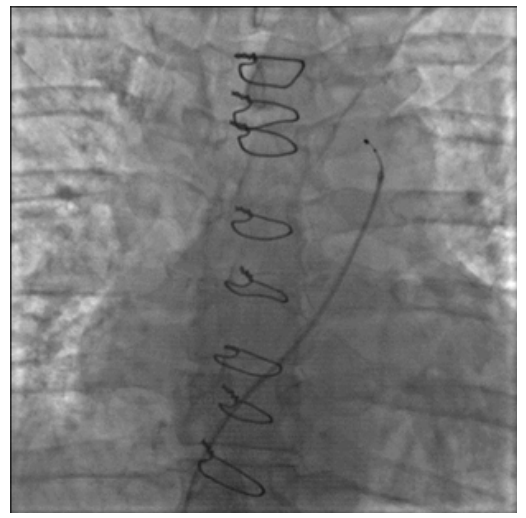
Figure 2: Cryoablation of the left pulmonary artery.
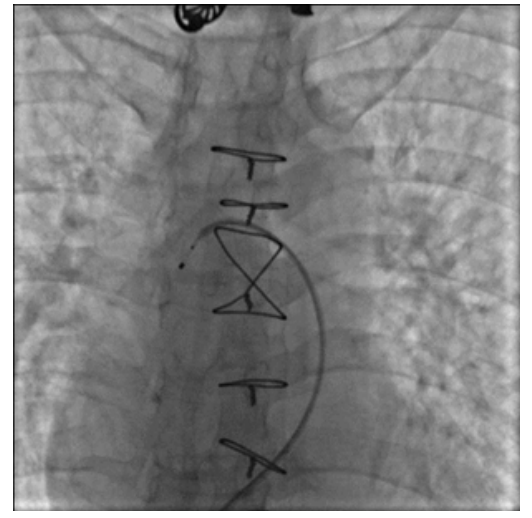
Figure 3: Cryoablation of the right pulmonary artery.
Follow-up
Patients were monitored in the intensive care unit for at least 24 hours before discharge from the hospital. Clinical follow-up was 12 months period: patients were hospitalized for assessment of clinical status and right heart catheterization, 6MWD, and NT- proBNP measurement.
Endpoints and definitions
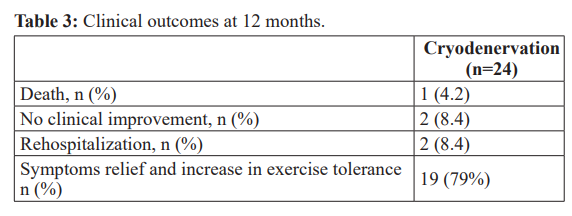
The primary endpoints were: the changes in clinical status according to NYHA classification; the occurrence of adverse clinical events (all-cause death, the lack of improvement in CHF functional class, rehospitalization during follow-up period due to worsening clinical status); the changes in functional capacity (measured by 6 MWT) and in NT-proBNP level. The secondary endpoint was the dynamic of hemodynamic parameters (mPAP, PWCP, PVR, DPG) at 12-month follow-up examination.
Statistical Analysis
Continuous variables are expressed as mean ± SD. Differences in continuous variables were analyzed using paired-sample Student t tests. The categorical variables were compared using the Fisher exact test. Statistical significance was defined as p value < 0.01. All analyses were performed using the statistics program SPSS version 20.0 for Windows (SPSS Institute, Chicago, Illinois).
Results
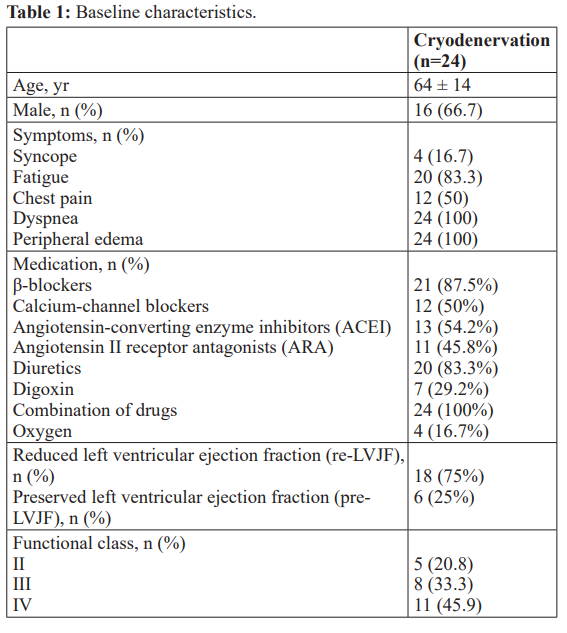
Patients were being included in the study between April 2018 and April 2019. All patients had clinical symptoms of chronic heart failure: dyspnea, fatigue, peripheral edema. Among the 24 patients, 18 (75%) had pulmonary hypertension secondary to left heart disease with reduced left ventricular ejection fraction (re-LVJF) – 5 patients (20.8%) had aortic valve disease, 7 patients (29.2%) had ischemic heart disease with previous myocardial infarction and 6 (25%) patients had dilated cardiomyopathy; 6 (25%) patients had pulmonary hypertension with preserved left ventricular ejection fraction (pre-LVJF) secondary to systemic arterial hypertension.
Procedural Outcomes
The median number of cryoablation sites was 10.8 ± 0.9, the median duration of cryoablation was 22 (18–25) minutes. There were no complications during and immediately following the cryoablation procedure (death, arrhythmias, PA perforation, acute thrombus formation in the right heart or at the access site, bleeding). All patients tolerated the procedure without the need for sedative or analgesic agents. Three patients developed sinus bradycardia during the cryoablation, none of them required special treatment.
12 months follow-up
During 12-months of follow-up one patient died for non-cardiac reason (severe gastric bleeding), 19 patients reported significant relief of symptoms and increase in exercise tolerance, 2 patients did not demonstrate any clinical improvement and 2 more needed rehospitalization because of deterioration of CHF status.
Functional capacity and NT-proBNP level before and 12 months after cryoablation procedure.
There was statistically significant increase in functional capacity measured by 6MWT: 319 ± 18 m before cryodenervation and 502 ± 22 m 12 months after procedure. The N-terminal pro–brain natriuretic peptide value decreased from 2928 ± 223 ng/mL at baseline to 989 ± 67 ng/mL at 12 months follow-up.
Hemodynamic responses to the cryoablation procedure
At 12 months follow-up the right heart catheterization (performed in 23 patients) demonstrated the significant improvements in parameters related to pulmonary hypertension. There was distinctive reduction of mean pulmonary artery pressure (mPAP) from 59 ± 6 to 32 ± 4 mm Hg, pulmonary vessel resistance (PVR) from 9,3 ± 2,2 to 3,4 ± 1,5 WU and diastolic pulmonary gradient (DPG) from 11 ± 2.1 to 8 ± 0.8 mm Hg. Moreover, the decrease of pulmonary capillary wedge pressure (PCWP) from 23 ± 3.5 to 19 ± 2.3 mm Hg was also observed.
Discussion
Pulmonary artery hypertension (PAH) is condition caused by different hemodynamic mechanisms. Over the past two decades most of the studies have been focused on the research and treatment of precapillary pulmonary hypertension. Precapillary pulmonary hypertension is characterized by an increased mPAP (> 25 mm Hg), pulmonary vessel resistance – PVR (> 3 WU) and normal pulmonary capillary wedge pressure – PCWP (< 15 mm Hg). Normal PCWP (< 15 mm Hg) is indicator of preserved left ventricular function. The most common reasons behind development of precapillary pulmonary hypertension are chronic pulmonary thromboembolism, chronic obstructive lung disease and idiopathic pulmonary arterial hypertension.
The hypothesis of sympathetic overreaction as a trigger in the development and progression of different pathologic condition has been the object of particular scientific interest for a long time. The leading role of enhanced sympathetic activity in setting PAH was established in several experimental and clinical studies. Increased circulating catecholamine levels and high sympathetic nerve traffic in patients with severe PAH have been reported in the studies by Velez-Roa et al. [11] and Wensel et al. [12]. These finding were confirmed by another evidences enhanced muscle sympathetic nerve activity and impaired heart rate variability [13] conditions correlated strongly with advanced PAH.
The sympathetic overreaction leads to vasoconstriction prevalence (e.g., thromboxane A2, endothelin, and serotonin) over vasodilatation (e.g., prostacyclin, nitric oxide, and vasoactive intestinal peptide) and to significant morphologic changes in the pulmonary circulation consequently. Anatomic and pathological studies have revealed hypertrophy of the muscular layer and general remodeling of a small arterioles and main arteries of pulmonary vessel bed [14,15]. Furthermore, vasoconstriction mechanism and general pulmonary vascular remodeling result in RV strain and development of right heart failure.
It has been well established fact that right heart failure is condition very difficult to treat. The existing medications have very limited ability to slow down PAH progression and have not been associated with significant improvements in clinical symptoms, functional capacity or long-term prognosis according to several studies [16,17]. Besides, the severe side effects and high cost are serious limitation for patients receiving drug therapy for the treatment of pulmonary artery hypertension. Several randomized control trials in patients with PAH (IPAH, chronic thromboembolic pulmonary hypertension and associated PAH) demonstrated very modest clinical and hemodynamic response from a different drugs combination: the average improvement of functional capacity as assessed by 6MWT was 35.61 m, and the mean reduction in the mPAP was only 2.86 mm Hg [18,19].
The unsatisfactory effects of medical therapy in patients with PAH and proven evidences of enhanced sympathetic activity as a leading mechanism in pathogenesis of PAH were the main stimulus behind the development a new non-medical treatment and its implementation into clinical practice. The data, gathered from morphologic studies, demonstrated that the innervation of the pulmonary artery is predominantly sympathetic [20,21]; with 23 bundles of large nerve trunks around bifurcation of PA diminishing in size rapidly in the direction to the arterioles. Other experimental studies discovered the superficial location of PA nerve trunk (at the PA bifurcation level) very close to the intimal surface [22,23]. These findings have proven to be favorable for sympathetic ablation at this specific location and substantiate the methodology to carry out PADN at the main pulmonary artery and at the ostium of left and right pulmonary arteries.
The potential benefit of PADN in lowering pulmonary pressure rise was clearly demonstrated in experimental model. The authors studied hemodynamic effects of PADN in animal laboratory performing acute occlusion one of the main PA branches [24]. The results showed that during occlusion of left interlobar PA, mPAP and PVR increased significantly reaching peak values after 5 min, and that this pressure rise was completely abolished after PADN at the MPA bifurcation level. The experimental success of PADN and also proven clinical effectiveness of renal denervation for the treatment of the refractory arterial hypertension postulated the potential clinical benefit of the pulmonary artery denervation [25,26].
In 2013 Chen et al. published results of the first phase PADN-1 first-in-human study [7]. The purpose of the study was to evaluate effectiveness and safety of radiofrequency pulmonary artery denervation in patients with idiopathic pulmonary hypertension. IPAH is a typical precapillary pulmonary hypertension and it is characterized by an increased mPAP (> 25 mm Hg), pulmonary vessel resistance – PVR (> 3 WU) and normal pulmonary capillary wedge pressure – PCWP (< 15 mm Hg). In this study were included only patients with IPAH refractory to medical therapies. Out of a total of 21 patients, 13 patients received the pulmonary artery denervation (PADN) procedure; the other 8 patients who refused the PADN procedure were assigned to the control group. The major findings in this study were that PADN was safe, associated with significant hemodynamic improvements and increase in functional capacity. Authors reported at 3-month follow-up reduction of mPAP (from 55 ± 5 mmHg to 36 ± 5 mmHg, p<0.01) and improvement of the 6MWT (from 324 ± 21 m to 491 ± 38 m, p<0.006) in the PADN group with no significant changes of mPAP and 6 MWT in the control group.
Although the pathogenesis and treatment of precapillary pulmonary hypertension have received most of attention from a recent studies, the postcapillary PAH is far more common and difficult to manage. Apart from precapillary PAH, postcapillary PAH is a common complication of a chronic heart failure secondary to left side disease either with reduced or preserved ejection function. Any type of left heart disease might result in a rise of pulmonary venous pressure: ischemic heart disease, valve disease or any other obstructive lesion, systemic arterial hypertension. Left ventricular disturbances in systolic or diastolic function leads to increased left ventricular diastolic filling pressure, which in turn creates hemodynamic condition for the backward transmission of increased left ventricular filling pressure to the left atrium and pulmonary veins. This status is known as passive or isolated post- capillary (Ipc) pulmonary artery hypertension (PAH), with elevated mPAP and PCWP but without an elevation of pulmonary vascular resistance (PVR) or diastolic pulmonary gradient (DPG) [27]. The effective management of PAH at this stage depends mostly on the background disease. Moreover, the special medications targeting the elevating pulmonary artery pressure is not recommended and lowering pulmonary vessel resistance (PVR) is considered as potential harm because of possible overload of impaired left ventricular function. The potential mechanisms behind this unfavorable effect are a large amount of blood return following mPAP reduction and CO increases (hyperkinetic status).
The development of postcapillary PAH due to the progression of left heart diseases is not only an important sign of clinical worsening, but also a turning point in sympathetic neurohumoral response. The enhanced sympathetic activation may trigger vasoconstriction, global vascular remodeling and consequent development of “overreactive” or “out of proportion” pulmonary hypertension. This condition is also known as Combined postcapillary PAH (CpcPAH), which is defined as a DPG of ≥ 7 mm Hg or PVR of >3 Wood units (WU), or both [28]. These hemodynamic changes are associated with more severe clinical status and poor clinical outcomes. controversy still exists regarding the routine treatment of CpcPAH with drugs targeting pulmonary arterial hypertension (PAH). This controversy underlines the importance of fully understanding the neurohumoral mechanisms in these patients behind the increased pulmonary artery pressure. Taking into account, that superimposed pulmonary arterial vasoconstrictor component is one of the major mechanisms of CpcPAH, the potential of pulmonary artery denervation (PADN) to target the sympathetic over activation is quite promising.
Second phase of PADN-1 study included 66 patients with pulmonary hypertension of different causes, such as idiopathic pulmonary artery hypertension and PAH secondary to left-sided heart failure [8]. At 12 months after procedure of pulmonary denervation the 6MWD increased by a mean of 94 ± 73 m, the N-terminal pro– brain natriuretic peptide value decreased from 2229 ± 2922 ng/ mL at baseline to 917 ± 947 ng/mL and the mean paired WHO class was 2.7 ± 0.6 at baseline compared to 1.9 ± 0.7 at the last follow-up (P<0.001). These results clearly demonstrated that PADN procedure was associated with significant improvements in exercise capacity and cardiac function in patients with precapillary and combined postcapillary PAH as well.
The PADN-5 randomized sham-controlled study, which included 98 patients with Combined postcapillary Pulmonary Artery Hypertension Associated with Left Heart Failure, showed much favorable clinical results in radiofrequency denervation group over medical treatment (sildenafil) group [29]. This is first randomized clinical trial studied the effectiveness of PADN in patients with CpcPAH using a sham-procedure control group. These findings confirmed previous reports about the safety and efficacy of PADN for patients with CpcPAH. Moreover, the authors demonstrated significantly less frequent clinical worsening with PADN compared with sildenafil therapy.
The Catheter Cryoablation is a rapidly advancing method for the treatment of cardiac arrhythmias. Recent studies have found cryoablation to be very effective in symptoms relief and improving long-term prognosis in patients with different kind of heart rhythm and conduction disorders. For a example, the catheter cryoablation for pulmonary vein isolation (PVI) in atrial fibrillation (AF) has become an established treatment option as alternative for radiofrequency catheter ablation [30,31]. Moreover, cryoablation method has some advantages over radiofrequency ablation that makes this procedure more preferable in clinical practice.
Experimental studies have demonstrated that cryoablation did not induce stenosis of PV or coronary sinus and was associated with less activation of platelet and a lower thrombogenic tendency than RF energy [32,33]. Furthermore, the cryoablation procedure is conducted with few adjunctive tools and with non- general anesthesia in most cases, which may support the wide- spread utilization of this method. Typically, the time required to perform cryoablation procedure is much shorter in comparison to radiofrequency ablation; and patients generally experience less pain than with radiofrequency ablation. Additionally, moderate sedation during cryoablation procedures has been reported to result in similar efficacy and patient satisfaction as general anesthesia while reducing procedure costs [34,35] Together, these results reinforce the safety of cryoablation in real-world practice and suggest that cryoablation might be applicable for effective destruction of different type of tissues without general anesthesia. The widespread use of cryoablation in modern world, the similar effectiveness of cryoablation and radiofrequency ablation in managing cardiac arrhythmias encouraged us to perform cryoablation procedure for sympathetic pulmonary artery denervation. We postulated that proven efficacy of radiofrequency PADN and favorable anatomical characteristics (mostly sympathetic innervation of pulmonary artery) substantiated the use of cryoablation for destruction of sympathetic fibers located at the bifurcation of the main pulmonary trunk. The main goal of our study was to evaluate the impact of modulated sympathetic activity after cryodenervation in patients with pulmonary artery hypertension. To the best of our knowledge, this is the first study to report hemodynamic, functional, and clinical responses to cryoablation procedure in patients with combined postcapillary PAH secondary to left heart disease.
We assessed changes of hemodynamic parameters, functional capacity and clinical status at 12-months follow-up period. First of all, we did not register any complication related to cryoablation procedure during the hospital stay. The procedure was tolerated well by all patient, none of them reported any pain or discomfort during intervention. There were no requirements for general anesthesia and all patients received mild sedation.
The major finding of our study is that the cryoablation PADN procedure was associated with significant changes in hemodynamic parameters, functional capacity and clinical status after 12 months. Favorable 12 months outcomes were evidenced by improvements in pulmonary hemodynamic, increased stamina as shown by 6MWD, decreased N-terminal pro–brain natriuretic peptide level, and a low rehospitalization rate due to heart failure related events. The right heart catheterization, performed 12 months after cryoablation revealed statistically significant reduction of mPAP, PVR and DPG. These positive trends might indicate the possibility of a changes in stiffness and remodeling of vascular wall as a result of modulated sympathetic activity. The hemodynamic changes of pulmonary circulation were quite predictable and anticipated. These improvements were clearly demonstration of better pulmonary hemodynamic and less resistance of microcirculatory vascular bed. Interestingly, there was significant reduction of PCWP after cryoablation a clear mark of better left ventricular function. Fortunately, these finding did not prove our concerns that larger amount of blood return following PVR reduction and increased cardiac output (hyperkinetic status) would lead to further pulmonary vein congestion and left ventricular overloading. In fact, the decrease in PCWP might be explained by potential positive role of cryoablation PADN for left ventricular remodeling. These finding are consistent with scientific data indicated the positive impact of renal arteries denervation on left ventricular function and clinical status in patients with chronic left heart disease [36,37]. Neurohumoral disbalance and predominantly sympathetic activation are most likely behind the same damaging effect on myocardium and pulmonary circulation as well. There are scientific evidences that enhanced sympathetic drive may induce inflammation response and facilitate immune activation in the most body tissues that in turn leads to insulin resistance, peripheral vasoconstriction, renal insufficiency and aggravation of heart failure [38,39]. Furthermore, peripheral vascular constriction and left ventricular remodeling aggravate left ventricular function. Consequent pulmonary vein congestion, development of isolated postcapillary pulmonary artery hypertension (IpcPAH) and then combined postcapillary pulmonary artery hypertension (CpcPAH) complete the vicious circle with further exacerbation the existing neurohumoral disbalance with prevalent sympathetic drive.
Potentially, combined pulmonary and renal denervation are justified and would have clinical effect in patients with left hear disease deteriorating into progression of pulmonary hypertension. Both procedures eliminate factors and sympathetic-parasympathetic disbalance contributing to worsening left hear disease (with either preserved or reduced EF) and progression of pulmonary hypertension.
Conclusion
This is the first clinical study to demonstrate the clinical, functional and hemodynamic benefits of cryoablation procedure in patients with CpcPAH secondary to left heart diseases. Randomized clinical trials are needed to prove favorite outcomes after treatment with cryoablation in this patient population.
Study Limitations
The study included the small number of patients without a control group. Although the long-term results of cryoablation in patients with CpcPAH are encouraging, more multicenter and randomized trials must be done in a larger cohort of patients before clinical efficacy of this method is determined.
References
- Marc Humbert, Gabor Kovacs, Marius M Hoeper, et 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: Developed by the task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Endorsed by the International Society for Heart and Lung Transplantation (ISHLT) and the European Reference Network on rare respiratory diseases (ERN-LUNG). European Heart Journal. 2022; 43: 3618-3731.
- Juratsch CE, Jengo JA, Castagna J, et Experimental pulmonary hypertension produced by surgical and chemical denervation of the pulmonary vasculature. Chest. 1980; 77: 525-530.
- Laks MM, Juratsch CE, Garner D, et Acute pulmonary artery hypertension produced by distention of the main pulmonary artery in the conscious dog. Chest. 1975; 68: 807-813.
- Zhou L, Zhang J, Jiang XM, et Pulmonary artery denervation attenuates pulmonary arterial remodeling in dogs with pulmonary arterial hypertension induced by dehydrogenized monocrotaline. J Am Coll Cardiol Intv. 2015; 8: 2013-2023.
- Esler MD, Krum H, Sobotka PA, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. 2010; 376: 1903-1909.
- Bhatt DL, Kandzari DE, O’Neill WW, et al. A controlled trial of renal denervation for resistant N Engl J Med. 2014; 370: 1393-1401.
- Chen SL, Zhang FF, Xu J, et Pulmonary artery denervation to treat pulmonary arterial hypertension: a single-center, prospective, first-in- man PADN-1 study (first-in-man pulmonary artery denervation for treatment of pulmonary artery hypertension). J Am Coll Cardiol. 2013; 62: 1092-1100.
- Chen SL, Zhang H, Xie DJ, et Hemodynamic, functional, and clinical responses to pulmonary artery denervation in patients with pulmonary arterial hypertension of different causes: phase II results from the Pulmonary Artery Denervation-1 Study. Circ Cardiovasc Interv. 2015; 8: e002837.
- ATS Statement. Guidelines for the Six-Minute Walk Test. American Journal of Respiratory and Critical Care Medicine. 2002; 166: 111-117.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Circulation. 2013; 128: 1810-1852.
- Velez-Roa S, Ciarka A, Najem B, et Increased sympathetic nerve activity in pulmonary artery hypertension. Circulation. 2004; 110: 1308-1312.
- Wensel R, Jilek C, Dorr M, et Impaired cardiac autonomic control relates to disease severity in pulmonary hypertension. Eur Respir J. 2009; 34: 895-901.
- Grigioni F, Potena L, Galiè N, et al. Prognostic implications of serial assessments of pulmonary hypertension in severe chronic heart J Heart Lung Transplant. 2006; 25: 1241-1246.
- Guazzi M, Borlaug Pulmonary hypertension due to left heart disease. Circulation. 2012; 126: 975-990.
- Fayyaz A, Edwards W, Maleszewski J, et Global pulmonary vascular remodeling in pulmonary hypertension associated with heart failure and preserved or reduced ejection fraction. Circulation. 2018; 137: 1796-1810.
- Galiè N, Palazzini M, Leci E, et Current Therapeutic Approaches to Pulmonary Arterial Hypertension. Rev Esp Cardiol. 2010; 63: 708-724.
- Anderson J, Nawarskas J. Pharmacotherapeutic management of pulmonary arterial hypertension. Cardiol Rev. 2010; 18: 148-162.
- Galiè N, Manes A, Negro L, et A meta-analysis of randomized controlled trials in pulmonary arterial hypertension. Eur Heart J. 2009; 30: 394-403.
- Hwang I, Kim Y, Park J, et Pulmonary hemodynamics and effects of phosphodiesterase type 5 inhibition in heart failure: a meta-analysis of randomized trials. BMC Cardiovasc Disord. 2017; 17: 150.
- Verity M, Bevan Fine structural study of the terminal effectors plexus, neuromuscular and intermuscular relationships in the pulmonary artery. J Anat. 1968; 103: 49-63.
- Richardson J. Nerve supply to the lungs. Am Rev Respir Dis. 1979; 119: 785-802.
- Chen S, Zhang Y, Zhou L, et al. Percutaneous pulmonary artery denervation completely abolishes experimental pulmonary arterial hypertension in vivo. EuroIntervention. 2013; 22: 269-276.
- Rothman A, Arnold N, Chang W, et al. Pulmonary artery denervation reduced pulmonary artery pressure and induces histological changes in an acute porcine model of pulmonary Circulation Cardiovasc Interv. 2015; 8: e002569.
- Zhou L, Zhang J, Jiang X, et Pulmonary artery denervation attenuates pulmonary arterial remodeling in dogs with pulmonary arterial hypertension induced by dehydrogenized monocrotaline. J Am Coll Cardiol Intv. 2015; 8: 2013-2023.
- Esler M, Krum H, Sobotka P, et Renal sympathetic denervation in patients with treatment-resistant hypertension (the Symplicity HTN-2 trial): a randomized control trial. Lancet. 2012; 376: 1903-1909.
- Bhatt D, Kandzari D, O’Neill W, et al. SYMPLICITY HTN- 3 Investigators. A controlled trial of renal denervation for resistant N Engl J Med. 2014; 370: 1393-1401.
- Opitz C, Hoeper M, Gibbs J, et Precapillary, combined and postcapillary pulmonary hypertension: a pathophysiological continuum. JACC. 2016; 68: 368-378.
- Vachiery J, Adir Y, Barbera J, et al. Pulmonary hypertension due to left heart disease. JACC. 2013; 62: 100-108.
- Hang Z, Juan Z, Mengxuan C, et Pulmonary Artery Denervation Significantly Increases 6-Min Walk Distance for Patients with Combined Pre- and Post-Capillary Pulmonary Hypertension Associated with Left Heart Failure: The PADN- 5 Study. JACC Cardiovasc Interv. 2019; 12: 274-284.
- January C, Wann S, Alpert J, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm J Am Coll Cardiol. 2014; 64: 1-76.
- Garg J, Chaudhary R, Palaniswamy C, et al. Cryoballoon versus Radiofrequency Ablation for Atrial Fibrillation: A Meta-analysis of 16 Clinical Trials. J Atr Fibrillation. 2016; 9: 14-29.
- Farah A, Khan F, Machado Thrombus formation at the site of radiofrequency catheter ablation. Pacing Clin Electrophysiol. 2000; 23: 538-540.
- Khairy P, Chauvet P, Lehmann J, et al. Lower Incidence of Thrombus Formation with Cryoenergy Versus Radiofrequency Catheter Circulation. 2003; 107: 2045-2050.
- Kuck K, Fürnkranz Cryoballoon ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2010; 21: 1427- 1431.
- Andrade J, Khairy P, Guerra P, et al. Efficacy and safety of cryoballoon ablation for atrial fibrillation: a systematic review of published Heart Rhythm. 2011; 8: 1444-1451.
- Almeida M, Gonçalves P, Branco P, et al. Impact of Renal Sympathetic Denervation on Left Ventricular Structure and Function at 1-Year Follow-Up. PLoS One. 2016; 11:
- Schirmer SH, Sayed MM, Reil JC, et Improvements in left ventricular hypertrophy and diastolic function following renal denervation: effects beyond blood pressure and heart rate reduction. J Am Coll Cardiol. 2014; 63: 1916-1923.
- Li Chao MM, Xia, Wei MM, Wang Li MM, et al. Effect of Renal Denervation on Cardiac Function and Inflammatory Factors in Heart Failure After Myocardial Infarction. Journal of Cardiovascular 2020; 76: 602-609.
- Zaldivia MT, Rivera J, Hering D, et al. Renal denervation reduces monocyte activation and monocyte–platelet aggregate formation: an anti-inflammatory effect relevant for cardiovascular Hypertension. 2017; 69: 323-331.