Culture Negative Endocarditis
Author'(s):Adel Ekladious1,2*
1Associate Professor, Faculty of health and medical sciences,University of western Australia, G11 M Block, UWA Health Campus(QEI) Monash, Australia.
2Bega- south East Regional Hospital, 4 Virginia Drive, Bega New South Wales 2550, Australia.
*Correspondence:
Adel Ekladious, Associate Professor, Faculty of health and medical sciences, University of western Australia, G11 M Block, UWA Health Campus (QEI) Monash, Australia, Tel: 61499449905;E-mail: ekladiou@gmail.com.
Received: 26 July 2021; Accepted: 15 August 2021
Citation: Ekladious A. Culture Negative Endocarditis. Anesth Pain Res. 2021; 5(2): 1-3.
Keywords
Introduction
50--year-old gentleman went for a 3 weeks holiday trip to Indonesia with his partner and daughter He is an ex-smoker and ex-drug user; he drinks two glass of wine every night and few beers in the week end. He was diagnosed with mild obstructive airway disease with last FEV1 2.5 liter and fatty liver. He used sortied inhaler 25mcg/250mcg, 2 puffs BD daily, he takes Lipitor 20 mg for high cholesterol.
He spends one hour in the gym daily; he is up to date with his vaccination. He started to feel short of breath in the last week before going back home, he was seen by general practitioner who examined him and diagnosed him with chronic bronchitis and pulmonary congestion. The doctor ordered few blood tests and started him on Augmentin and oral steroids.
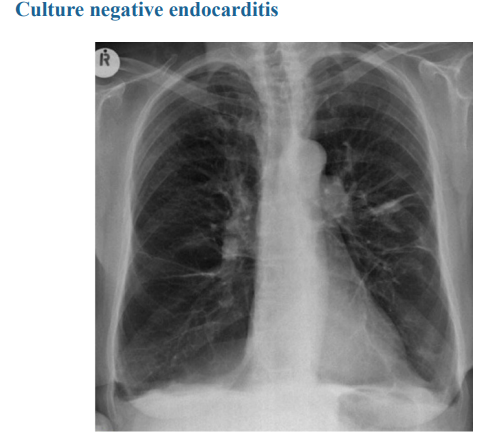
The patient did not improve and went to see his GP who discussed the results of blood test with him. The notable abnormal blood tests are ESR 130 and CRP 200, the results of the blood tests which included, Blood culture, full blood count, Liver function tests, urea and creatinine were all normal. Chest x ray showed mild right sided plural effusion, his doctor advised him to stay on the antibiotic, prednisolone and Seretide inhaler. He added salbutamol inhaler, the patient did not improve and the family decided to take him back home two days earlier.
The patient seen his GP again who decided to send him back for hospital admission as his oxygen saturation dropped to 94 on 2 liters of oxygen. The patient was admitted to acute medical unit in a tertiary hospital. He was diagnosed by the registrar as heart failure for investigation, the following investigations were requested, FBC, ESR, Blood culture, Urea, creatinine, D dimer, troponin, BNP, CTPA, ABG, pulmonary function test, induced sputum for pneumocystis jiroveci and Deaminase.
All above investigation was negative or normal apart from BNP was 400PG/ml (ref <100pg.ml). ESR 200, normal troponin, patient started on IV Tazocin 4.5 grams QID, pulmonary function can’t be done because the patient was breathless and his oxygen saturation dropped to 80% on non-rebreather musk. The patient reviewed by the consultant who decided to start him on hydrocortisone 100 mg/6 hours continue on IV Tazocin. The patient’s oxygen saturation dropped to 70%, heart rate accelerated to 140/min, respiratory rate accelerated to 40/min. The met call was initiated, patient was intubated and was mechanically ventilated.
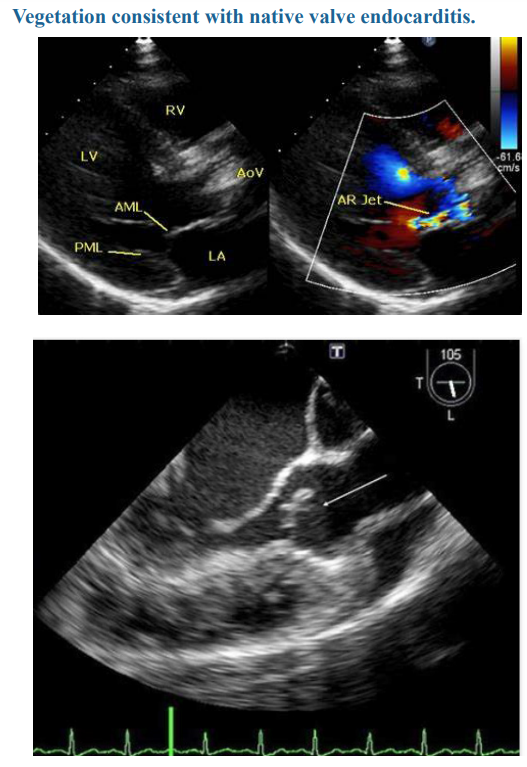
The patient had a bed site transthoracic echo which showed frank aortic incompetence, cardiothoracic surgeon was called to see the patient which had been taken to theatre for transesophageal echo which confirmed few small vegetations on the aortic valve. The metallic aortic valve replacement was performed, patient weaned from ventilator on day five, and started rehabilitation under multidisciplinary team and moved to the medical ward. In the medical ward the patient improved gradually, antibiotic stopped and he was started on warfarin indefinite with aim for INR from 2.5.-3.5.
The patient discharged home and given a diagnosis of culture negative aortic endocarditis probably due to treatment with antibiotic before the diagnosis., frank aortic incompetence and metallic Aortic valve replacement, repeated blood culture was sterile and the explanted valve was examined under microscopy, culture, serology and molecular testing for Coxiella Burneti, serology for Bartonella Henselae, Bartonella Quinana, Brucella Fastidious, Fungi, Tropheryma whipplei.
TB and other mycobacteria, in addition to Mycoplasma and Legionella. All results were negative apart from serology for Bartonella Henselae IGG was 1000. bacteriology and infectious diseases service were contacted, both agreed this titer is consistent with infection and advised for molecular testing with 16S r RNA which came strongly positive. The patient started on gentamycin for 2 weeks and doxycycline for three months with complete clinical and serological cure as repeated TOE and serology was negative.
Discussion
The culture negative endocarditis is not uncommon, accounting for 20% of all patients receiving the diagnosis of infective endocarditis [1] most commonly due to starting antimicrobial before confirmation of the diagnosis. The patient only received the diagnosis after examination of the explanted the native aortic valve
The delayed diagnosis prevents active management with optimal antibiotics, early involvement of multi-disciplinary team and patient centered care including interdisciplinary are essential and considered best practice [2]. The current best practice is to use conventional automated blood culture and conventional media subculture for one week [3]. In order to diagnose slow growing organisms including the HACEK (Haemophilus, Aggregatibacter, Cardiobacterium, Eikenlla, Kingella) group [3]. The other infective organisms Coxiella Burnetii, Mycobacteria including mycobacterium chimera (usually following cardiac surgery). The fungi including Aspergillus, Bartonella henselae, Bartonella Quintana, Brucella, non-infective causes of endocarditis encompass systemic Lupus causing Liebman- Sacks endocarditis, marantic endocarditis due to malignancy (breast, lung, prostate, colon cancer) [4] and Bechet’sendocarditis [5]. The current multimodal diagnostic strategy consider valve biopsy specimens are essential part of the examination which includes serology, broad range molecular and histopathology.
Duke Criteria for infective endocarditis include either one major and two minor criteria, or two major or 5 minors. The major criteria are positive blood culture, vegetation positive histology of the valve for microorganisms consistent with endocarditis [6].
Minor criteria includes fever >38, vascular phenomena, immunologic phenomena, predisposing heart disease, because most of the organism in culture negative endo carditis are intracellular, slowly growing, some needs specific media (Torts, brown and Bern, Brown and Hopps),is commonly used for identifying and characterizing organisms in cardiac valves, GMS stain identify Fungi and other bacteria in the valve tissue, Zeihl- Nelson detect acid fast Bacilli, Bartonella is very hard to be detected by any stain and most micro bacteriologist consider when serology is
Caution should be exercised when interpreting staining properties, as microorganisms in valves removed from patients on antibiotics as bacterial morphology and stain may be altered [7].
Histological diagnosis is of paramount importance to diagnose culture negative non infective endocarditis due to neoplasm, and autoimmune disease [8].
Auto immune, antiphospholipid and vasculitis should be performed in culture negative endocarditis.
Few studies found culture of valves from patient without evidence of endocarditis were found to be falsely positive in 28%, a finding which could be dure to contamination during processes [9].
Molecular testing is increasingly utilized to aid in the diagnosis of culture negative endocarditis and have been applied to blood and excised tissue. The molecular methods used in endocarditis include organism specific PCR and broad range bacterial PCR followed by sequencing.
Organism specific primers had been developed for C burnetii, Bartnella species, T Whippeli, C acnes and M hominis (10) due to relative abundance of bacterial DNA in valves compared with blood or serum testing of cardiac tissues with organism - specific PCR is more sensitive than in blood testing.
Broad range bacterial PCR with amplification primers targeting the Bacterial 16S rRNA gene is a molecular method for ducting bacteria in general. The bacterial identification is determined by sequencing amplified DNA followed by comparison of the sequence to established date base.
Although a broad range bacteria PCR had been applied to blood, sensitivity is superior when performed on valve tissue and help detecting the organism in 70%. Molecular testing should be applied and performed on ant explanted or removed heart tissue [11].
Acknowledgment
A/P Adel Ekladious thank Dr Eline Ekladious for Editing the paper.
References
1.A Katsouli, MG Massad. Current issues in the diagnosis and management of Blood culture negative infective and non- infective endocarditis. Ann Thorac Surg. 2013; 95: 1467-1474.
2.José Zamorano, Javier Sanz, Carlos Almería, et al. difference between endocarditis with true negative blood culture and those with previous antibiotic treatment. J Heart Valve Dis. 2003; 12: 256-260.
3.Udoka Okaro, Anteneh, Addisu, Beata Cassanas, Burt Anderson. Bartonella Species, an emerging cause of Blood-culture negative Endocarditis.
4.M Demircin, R Dogan, O Peker, et al. Aortic insufficiency and enterococcal endocarditis complicating systemic lupus erythematosus. Thorac Cardiovasc Surg. 1995; 43: 302-304.
5.Jennifer L Lee, Stanley M Naguwa, Gurtej S Cheema, et al. Revisiting Libman-Sacks Endocarditis; a historical review and update. Clin Rev Allergy Immunol. 2009; 36: 126-130.
6.GA Dodds, DJ Sexton, DT Durack, et al. Negative predictive value of Duke criteria for infective endocarditis. Am J Cardiol. 1996; 77: 403-407.
7.Chaloncer GL, Harrison TG, Birtles RJ. Bartonella species as a cause of infective endocarditis in the UK. Epidemison Infect. 2013; 141: 841-846.
8.Harris KA, Yam T, Jalili S, et al. Service evaluation to establish the sensitivity, specificity and additional value of broad-range 16s r DNA PCR for the diagnosis of infective endocarditis from resected endocardial material in patients from eight UK and Ireland hospitals. EUR J Cli Microbiol Infect Dis. 2014; 33: 2061-2066.
9.D Raout, Jean-Paul Casalta, Herve richest, et al. Contribution of systematic serological testing in diagnosis of infective endocarditis. Journal of clinical Microbiology. 2005; 43: 5238-5242.
10.Clarisse Rovery, Gilbert Greub, Hubert Lebert, et al. PCR Detection of Bacteria on cardiac valves of patient treated for Bacterial endocarditis. Journal of Clinical Microbiology. 2005; 43: 163-167.
11.Tattevin P, Watt G, Revest M, et al. Update on blood culture negative endocarditis. Med Mal Infect. 2015: 45: 1-8.