De Winter’s Pattern - A Rare Electrocardiographic Sign of the Proximal Left Anterior Descending Artery Occlusion
Author(s): Ashmita KC, Vijay Yadav*, Ratna Mani Gajurel, Chandra Mani Poudel, Rajaram Khanal, Smriti Shakya, Roshan Ghimire and Sutap Yadav
Department of Cardiology, Manmohan Cardiothoracic Vascularand Transplant Center (MCVTC), Institute of Medicine (IOM), Kathmandu, Nepal.
*Correspondence:
Dr. Vijay Yadav, Department of Cardiology, ManmohanCardiothoracic Vascular and Transplant Center (MCVTC),Institute of Medicine (IOM), Kathmandu, Nepal, Phone no: +977- 9851201126.
Received: 25 Feb 2022; Accepted: 27 Mar 2022; Published: 02 Apr 2022
Citation: Ashmita KC, Yadav V, Gajurel RM, et al. De Winter’s Pattern - A Rare Electrocardiographic Sign of the Proximal Left Anterior Descending Artery Occlusion. Cardiol Vasc Res. 2022; 6(2): 1-5.
Abstract
De Winter’s pattern is a rare anterior wall ST segment elevation myocardial infarction (STEMI) equivalent electrocardiogram (ECG) pattern that signifies 2% of proximal left anterior descending (LAD) coronary artery occlusion. We present a case of 48 years old male who presented in emergency room with a typical ischemic type of chest pain for 2 hours duration whose 12 lead ECG showed the typical De Winter’s pattern. The patient underwent immediate coronary angiography (CAG) which revealed 95-99% thrombotic occlusion of the proximal to mid left anterior descending artery. He underwent primary percutaneous coronary intervention (PPCI) with an Everolimus eluting stent that eventually resulted in a favorable outcome. Through this case report, we aim to highlight the importance of timely recognition of the rare ECG pattern and the role of PPCI as an optimal therapeutic option for such patients.
Keywords
Introduction
De Winter’s ECG is an ECG pattern that was first described by De Winter et al in 2008 [1]. It signifies occlusion of the proximal left anterior descending coronary artery (p-LAD). It is characterized by an upsloping ST-segment depression of 1-3mm at the J-point in leads V1–V6 in concert with relatively tall, symmetrical T-waves along with possible loss of precordial R wave progression and mostly associated with concomitant 1–2 mm ST-segment elevation in lead aVR [1-3]. The QRS complexes are usually narrow and the ST-segment depression and T wave amplitude are frequently maximal in V3. Its importance lies on identification of myocardial ischemia due to p-LAD occlusion and need of early PPCI. The dilemmatic question of considering it as ST- elevation myocardial infarction (STEMI-equivalent) and its further management exempt the patient from timely management [1,4].
Case Presentation
We report the case of a hypertensive 48- year-old man who was a current smoker and had a family history of coronary artery disease. He presented in June 2021 to the emergency room with acute onset of severe retrosternal chest pain for 2 hours duration. The pain radiated to jaw, left arm, and was associated with diaphoresis and palpitation.
On Physical examination, he looked anxious, tachycardic (120 beats/min, irregular) and normotensive (120/80 mmHg). His bilateral upper eyelids showed the presence of xanthalesma (Figure 1). The chest auscultation revealed normal vesicular breath sound on bilateral lung fields. He had normal heart sounds without cardiac murmur and no added sounds.

Figure 1: Xanthelasma over bilateral upper eyelids
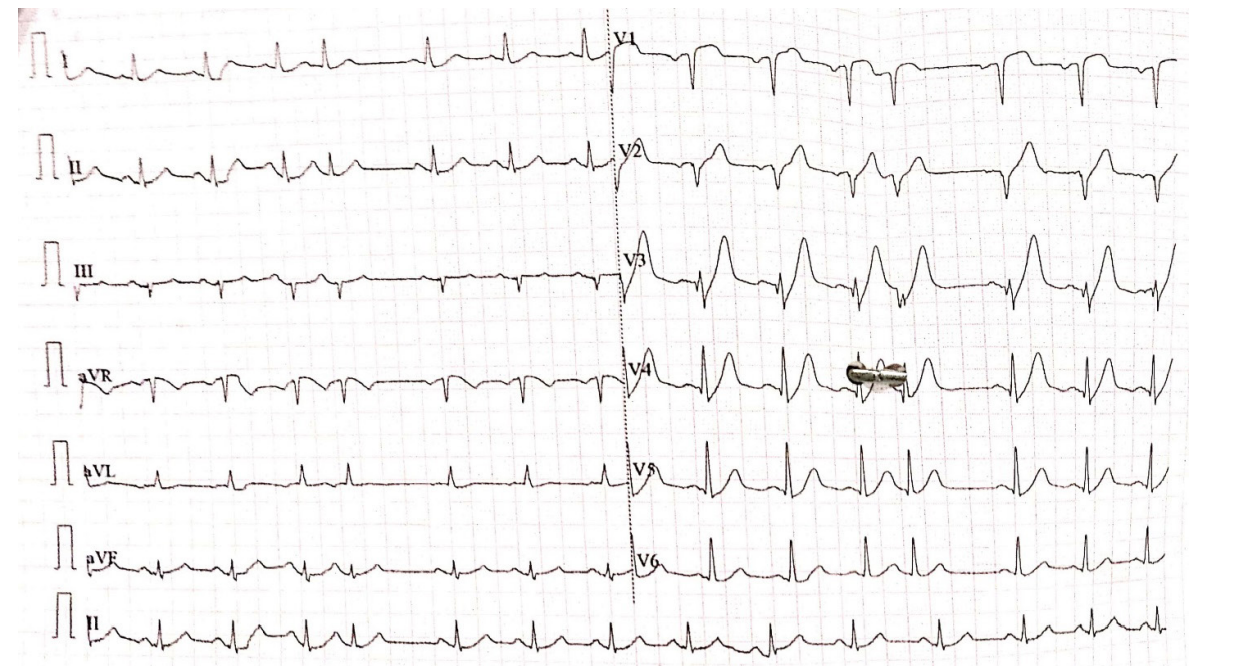
Figure 2: ECG at presentation showing De Winter’s pattern; upsloping ST-segment depression of >1mm at the J-point in leads V3–V6 with relatively tall, symmetrical T-waves, and >1mm ST-segment elevation in lead aVR.
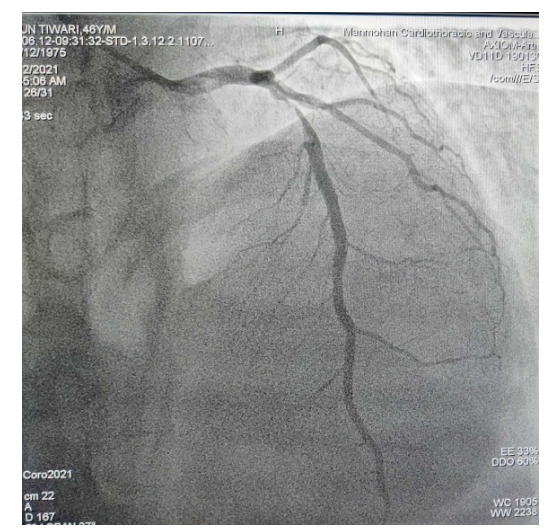
Figure 3: CAG showing thrombotic occlusion of p-m LAD
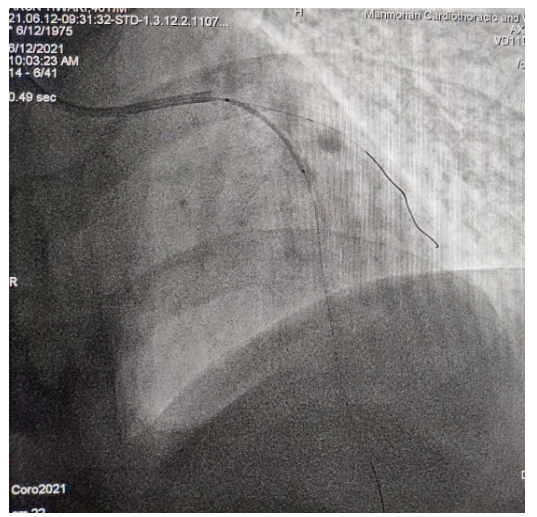
Figure 4: Stenting of the culprit artery (LAD).
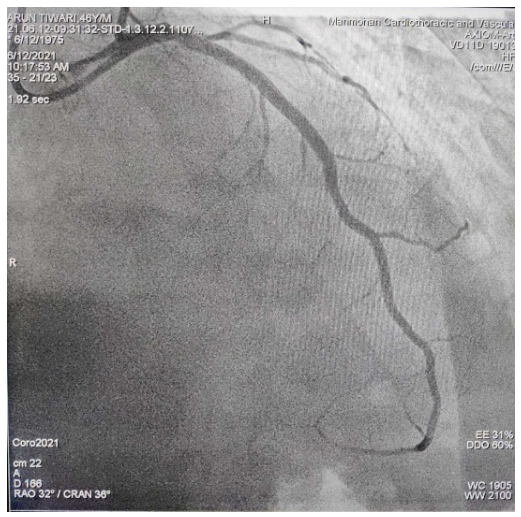
Figure 5: TIMI 3 flow in LAD following revascularization.
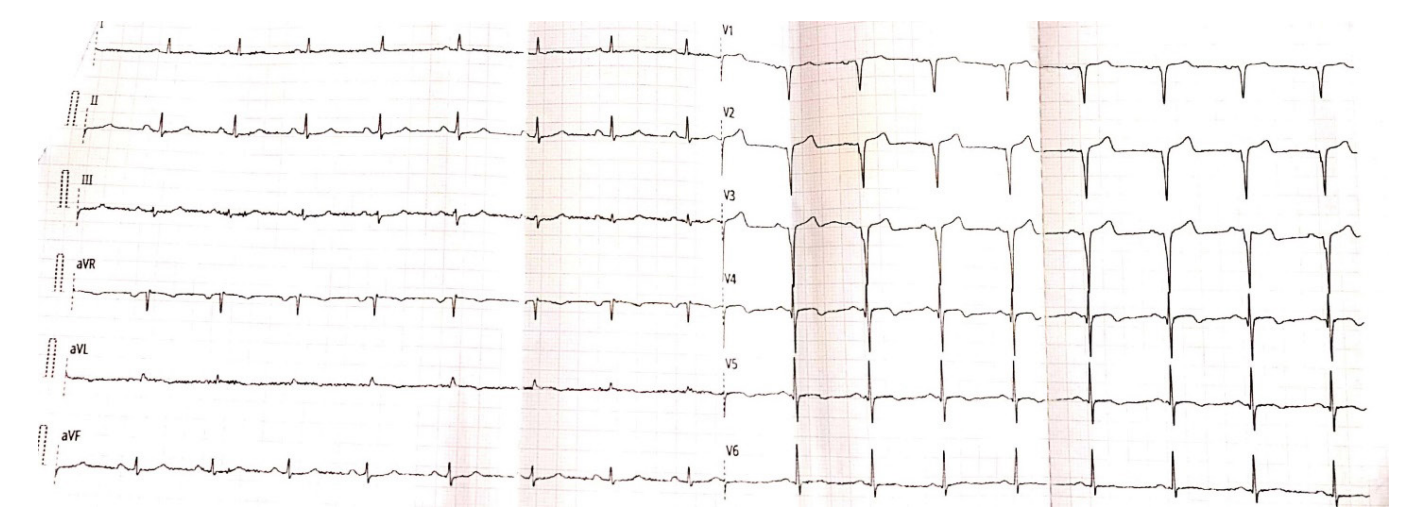
Figure 6: ECG after revascularization showing sinus rhythm with loss of De Winter’s pattern.
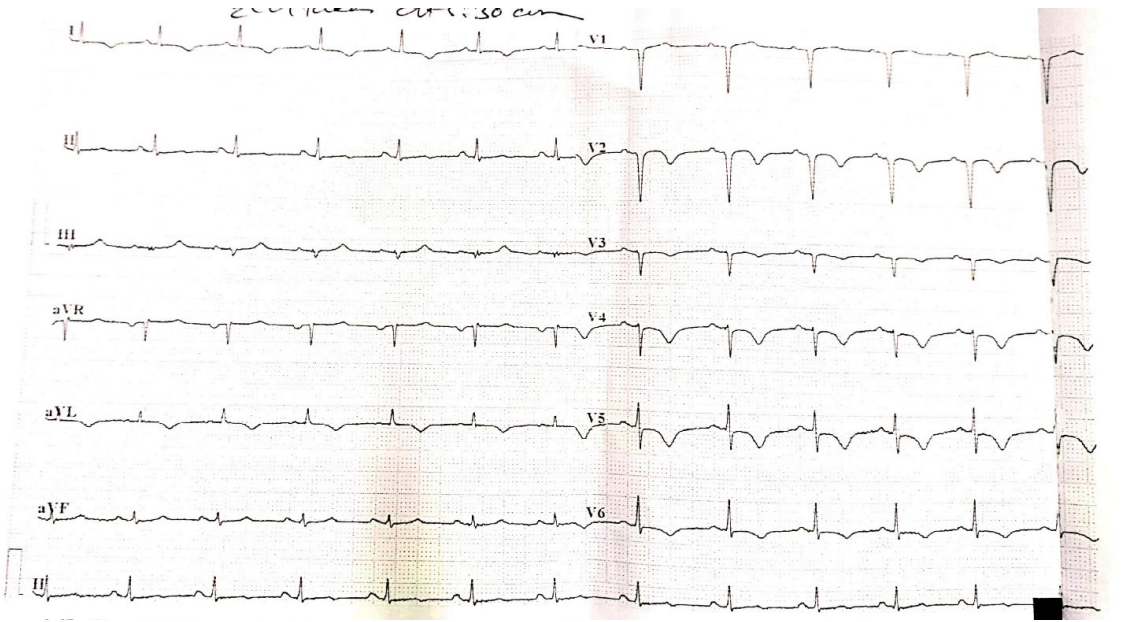
Figure 7: ECG at the time of discharge; sinus rhythm with T- wave inversion indicating successful reperfusion therapy.
Investigations
A 12-lead left sided ECG done immediately revealed a sinus rhythm with up sloping ST-segment depression of >1mm at the J-point in leads V3–V6, a relatively tall and symmetrical T-waves, and >1mm ST-segment elevation in lead aVR (Figure 2).
The bedside transthoracic echocardiography (TTE) depicted hypokinetic left anterior descending artery (LAD) territory, mild left ventricular systolic dysfunction with ejection fraction of 40- 45%, and grade I left ventricular diastolic dysfunction.
His baseline blood investigations, thyroid profile, fasting lipid profile were within normal limit and the quantitative troponin I level was within normal limits i.e., 0.038 ng/ml (normal <0.12 ng/ml). The baseline chest x-ray revealed no significant abnormality.
Treatment
Considering the possibilities of acute anterior wall myocardial infarction, patient was immediately provided with the loading dose of dual antiplatelets (Aspirin 300mg and Clopidogrel 600mg), statin (Rosuvastatin 40mg) and other required supportive measures in the emergency room. The immediate coronary angiography (CAG) showed 95-99% thrombotic occlusion of proximal to mid left anterior descending (p-m LAD) artery (Figure 3). The other coronary arteries were normal. A drug eluting stent (Everolimus) was deployed that eventually established a TIMI 3 flow in the culprit artery with no residual stenosis (Figures 4,5). Following revascularization, there was a loss of De Winter’s pattern in the ECG as shown in the figure 6.
Following the procedure, the patient was admitted in coronary care unit (CCU) and managed with dual antiplatelet, statin, low molecular weight heparin and other supportive measures. He had no post-procedure complications and was kept in observation for 2 days. He was discharged on oral dual anti-platelets, statin, beta- blocker, angiotensin converting enzyme inhibitor and diuretic. ECG at the time of discharge (Figure 7) showed T- wave inversion indicating successful reperfusion therapy.
Discussion
Electrocardiogram (ECG) plays a crucial role in diagnosis and timely management of STEMI. However, despite large acute myocardial infarction (MI), ST-elevation may not be evident on some cases posing diagnostic and therapeutic challenges. One such known variation is De Winter’s pattern; first described by De Winter et al in 2008 among 30 of 1532 patients (2.0%) with anterior myocardial infarction whose angiography later revealed occlusion of left anterior descending coronary artery. It is a static pattern as compared to hyperactive acute tall T waves in these patients [1]. However, it is still a dilemma that this pattern should be considered as static or those tall T waves as transient early feature of overt ST elevation.
De Winter’s pattern has a high positive predictive value (PPV) for proximal LAD obstruction. In earlier study conducted by Raja et al. the PPV ranged from 95.2%-100% [5]. Various theories have been postulated about pathophysiology behind this pattern. Anatomical variant of the Purkinje fiber with endocardial conduction delay could be the reason for absence of ST-elevation or it could be due to ischemic adenosine triphosphate (ATP) depletion causing lack of activation of sarcolemmal ATP-sensitive potassium channels (as observed in knock- out animal models of acute ischemia) [1,3]. Another mechanism may be large transmural ischemia directing the injury current away from the precordial leads and towards lead aVR [2,3]. It is also suggested that collateral supply to myocardium may prevent transmural ischemia preventing ST- elevation. However, ST elevation may be seen in absence of these collaterals [6].
As per a number of other studies, this pattern was observed among younger patients (mean age 52 years) as compared to STEMI patients (mean age 61 years) [5]. Active smokers, hypercholesteremia and family history of coronary artery disease were the common associated risk factor among these patients [5]. As with our case, typical ischemic chest pain is reported as the most common presenting symptom [3,7-10]. Initial level of troponin I was variable, it was elevated in majority of cases [3,8] however some cases report negative troponin I level [7,10]. Troponin I level of our case was 0.038 ng/ml (normal <0.12 ng/ml). Regarding the management, different studies consider it as a STEMI-equivalent and PPCI is accepted as appropriate treatment with possible benefits [1,3,5,10]. However, role of thrombolysis is still elusive but can be considered upon unavailability of PPCI [3,5,10]. Similarly in our case although the initial troponin I was negative patient was opted for coronary angiogram based on the ECG pattern which revealed 95-99% of p-m LAD for which PPCI to p-m LAD was done. Post procedure period was uneventful and he was discharged after 2 days.
There are no universally accepted guidelines to the optimal management of De Winter’s ECG pattern. The current management recommendations are based on available case reports and case series, which suggest PPCI as successful procedure. Our experience with this case also suggests that it can be considered as STEMI-equivalent and PPCI will be beneficial for such patients.
Conclusion
- The De winter’s ECG pattern signifies proximal left anterior descending coronary artery occlusion and it is seen in 2% of
- It is a cardiac emergency and early recognition of this pattern is pivotal for timely management.
- De Winter’s pattern can be considered as STEMI-equivalent and Primary percutaneous coronary intervention is beneficial for optimal outcomes.
References
- De Winter RJ, Verouden NJW, Wellens HJJ, et al. A New ECG Sign of Proximal LAD N Engl J Med. 2008; 359: 2071-2073.
- Verouden NJ, Koch KT, Peters RJ, et Persistent precordial “hyperacute” T-waves signify proximal left anterior descending artery occlusion. Heart. 2009; 95: 1701-1706.
- John TJ, Pecoraro A, Weich H, et al. The de Winter’s pattern revisited: A case Eur Hear J Case Reports. 2020; 4: 1-5.
- De Winter RW, Adams R, Verouden NJW, et al. Precordial junctional ST-segment depression with tall symmetric T-waves signifying proximal LAD occlusion, case reports of STEMI equivalence. J Electrocardiol. 2016; 49: 76-80.
- Raja JM, Nanda A, Pour-Ghaz I, et al. Is early invasive management as ST elevation myocardial infarction warranted in de Winter’s sign?-a “peak” into the widow-maker. Ann Transl Med. 2019; 7: 412-412.
- Birnbaum Y, Wilson JM, Fiol M, et al. ECG diagnosis and classification of acute coronary Ann Noninvasive Electrocardiol. 2014; 19: 4-14.
- Carrington M, Santos AR, Picarra BC, et De Winter pattern: A forgotten pattern of acute LAD artery occlusion. BMJ Case Rep. 2018; 226413.
- Barbati G, Caprioglio de Winter’s Pattern: An Unusual but Very Important Electrocardiographic Sign to Recognize. CJC Open. 2020; 2: 22-25.
- Missaoui E, Cherifa BC, Ahmed M, et al. The De Winter Dilemma: The Management and Outcome of a Patient with De Winter Electrocardiographic Pattern in the Pre-Hospital Setting. Med Case Rep. 2020; 6: 149.
- Prasad RM, Al-abcha A, Elshafie A, et The rare presentation of the de Winter’s pattern: Case report and literature review. Am Hear J Plus Cardiol Res Pract. 2021; 3: 100013.