Dellon Triple Decompression under WALANT
Author(s): Alves Marcelo Pinho Teixeira1*, Nunes Catia FC2
1Consultant Orthopaedic Surgeon at Hospital de Portalegre, Portugal.
2Orthopaedic Surgery Resident Doctor, Hospital Garcia de Orta, Portugal.
*Correspondence:
Alves Marcelo Pinho Teixeira, Consultant Orthopaedic Surgeon at Hospital de Portalegre, Portugal, Tel: +351 245 301 000.
Received: 11 Sep 2023 Accepted: 13 Oct 2023 Published: 20 Oct 2023
Citation: Pinho Teixeira AM, Nunes Catia FC. Dellon Triple Decompression under WALANT. Diabetes Complications. 2023; 7(1); 1-5.
Abstract
The Wide-Awake Local Anesthesia No Tourniquet (WALANT) Approach to Dellon Triple decompression involves the use of local anesthetic with epinephrine and no tourniquet. This study shows that WALANT is a safe and effective procedure and can be performed in an outpatient setting for the decompression of the common peroneal nerve in the knee, tibial nerve in the ankle and deep peroneal nerve in the dorsum of the foot in diabetic patients with superimposed nerve compressions to diabetic neuropathy. WALANT technique demonstrated to be a safe procedure to surgically treat diabetic patients with superimposed compressive neuropathy to diabetic neuropathy in the lower limbs and had no complications.
Keywords
Introduction
The Wide-Awake Local Anesthesia No Tourniquet (WALANT) approach involves the use of local anesthetic with epinephrine and no tourniquet. WALANT technique has been proven to be safe and effective for upper extremity surgery and is frequently associated with lower costs and less postoperative pain when compared with traditional methods of anesthesia [1].
Bilgetekin et al. observed that WALANT technique provided a short length of hospital stay in patients with foot and ankle injuries and affirmed that simple foot and ankle injuries could be managed successfully with this technique through adequate hemostasis without a tourniquet [2].
Wei et al. investigated the effectiveness of partial anterior cruciate ligament (ACL) suture repair under WALANT technique and observed that the use of this technique to repair partial ACL injuries under arthroscopy could retain the patient's own ligament tissue to the maximum extent and achieve satisfactory short-term effectiveness [3].
Maimaijiang et al. evaluated the effectiveness of lower extremity Dellon triple nerve decompression in the treatment of early-stage diabetic Charcot foot. They concluded that Dellon triple nerve decompression could improve the symptoms of Eichenholtz stage 0-1 diabetes Charcot foot, and had the advantages of less trauma, faster recovery, and fewer complications [4].
Fakkel et al. evaluated 60 patients that underwent Dellon triple lower extremity nerve decompression surgery between September of 2017 and March of 2019. The common, superficial, and deep peroneal nerves and the tibial nerve at the tarsal tunnel and soleal sling were decompressed if an entrapment was diagnosed. They observed that lower extremity nerve decompression surgery significantly improved patients’ quality of life by reducing neuropathy symptoms in cases of lower extremity nerve compressions [5].
In fact, to date there is no current paper that puts together WALANT surgery and the Dellon triple decompression in the treatment of lower limb superimposed nerve compression to chronic diabetic neuropathy. The goal of this study is to show that WALANT can be a safe and effective procedure and can be performed in an outpatient setting for Dellon triple decompression surgery, which is the decompression of the common peroneal nerve in the knee, deep peroneal nerve in the dorsum of the foot and the tibial nerve in the ankle in diabetic patients with superimposed nerve compressions to diabetic neuropathy.
Methods
The author obtained Institutional Review Board approval and followed Helsinki’s Declaration for human research and all patients signed an informed consent. During the year of 2022, a series of 10 patients with diabetic neuropathy were operated on for superimposed nerve compression of the common peroneal nerve in the knee (CPN), tibial nerve in the ankle (TN) and deep peroneal nerve (DPN) in the dorsum of the foot – the Dellon Triple surgical approach to superimposed nerve compression in diabetic neuropathy - using the WALANT technique. All patients had a positive Tinel’s sign over the CPN, TN and DPN and elicited pain on compression of the nerves (an effect similar to Durkan’s test for carpal tunnel syndrome). All had positive electromyograms (EMG) for diabetic neuropathy. No vascular compromise was detected because all patients had arterial and venous doppler studies before surgery. No previously amputated patient was included in this study.
The Dellon triple decompression was performed in all patients using WALANT. The first injection was over the course of the CPN over the head of the fíbula, at the lateral aspect of the knee (Figure 1). The used amount was 20mL of 1% lidocaine with 1:100.000 epinephrine. In figure 2, the area of vasoconstriction provided by WALANT is shown.
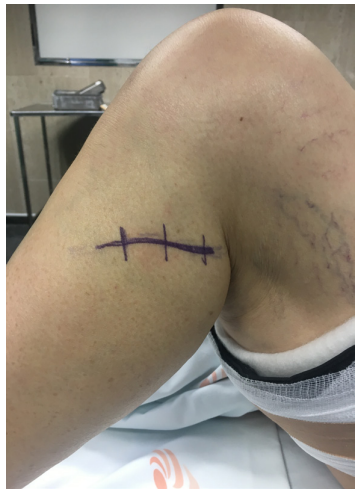
Figure 1: Site of injection over the common peroneal nerve at the neck of the fíbula. The picture shows the security tourniquet applied.
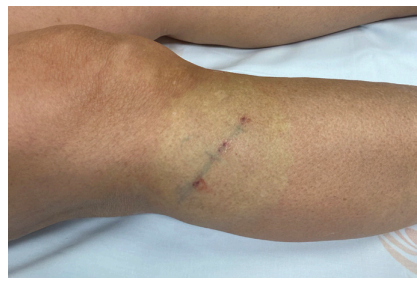
Figure 2: The WALANT effect over the common peroneal nerve course and programmed incision.
The second injection was at the medial aspect of the ankle, over the course of the TN (figure 3) in the tarsal tunnel; for this injection, the used amount was 10mL of the same mixture of lidocaine and epinephrine.

Figure 3: Site of injection over the tarsal tunnel and tibial nerve.
The third injection was on the dorsum of the foot, over the course of the DPN (figure 4), using 10mL of the same mixture of lidocaine and epinephrine.

Figure 4: Site of injection over the deep peroneal nerve on the dorsum of the foot.
After the injections, the limb is prepared for surgery. For a safety reason, the tourniquet is positioned in the proximal third of the thigh. The whole preparation of the limb and the surgical team gave enough time for the vasoconstriction effect provided by epinephrine to be achieved. It is known that the average time for this effect to be achieved is around 27 minutes. The incision was made on the appropriate locations over the course of the three nerves, starting with the CPN, followed by the TN and then the DPN. The CPN release was done proximally and distally until its division into deep and superficial peroneal nerves. In figures 5, 6, 7 and 8 the bloodless field and the course of the common peroneal nerve can be seen, and specially the area of constriction and compression of the nerve, which was completely released.

Figure 5: View of the bloodless field and the common peroneal nerve.

Figure 6: View of the bloodless field and the common peroneal nerve showing the area of compression.

Figure 7: View of the bloodless field and the common peroneal nerve.
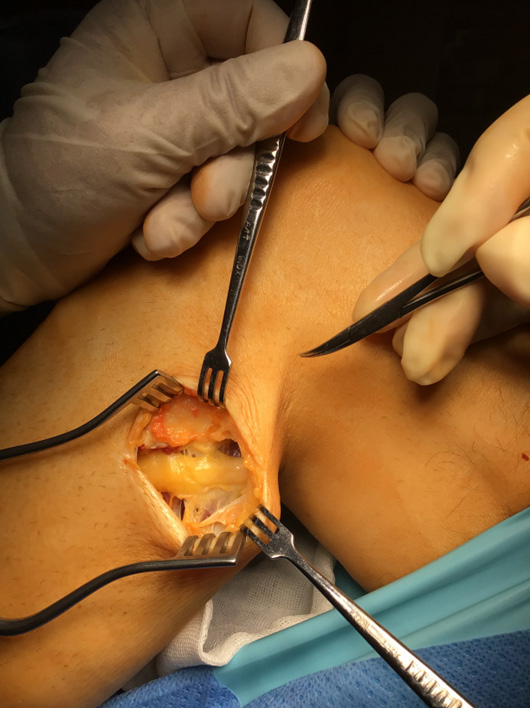
Figure 8: View of the bloodless field and the common peroneal nerve released.
The TN was also released proximally and distally, including its four branches. The DPN (figure 9) was decompressed by the division of the extensor hallucis brevis tendon, which crosses above the nerve to reach the hallux.

Figure 9: View of the deep peroneal nerve released in a bloodless field.
Results
All surgeries were performed in an outpatient setting. The author observed no complications. Complete release of the CPN, TN and DPN was achieved in all patients. There was no need for the use of phentolamine to revert the vasoconstriction effect. There was no need for insuflation of the tourniquet and the surgeries were performed in an almost bloodless field. All patients were able to walk home after the procedure, with the aid of a pair of crutches to avoid pressure on the operated limb.
In the first post-operative week, all patients were reevaluated, with special focus on the scars of the surgical incisions to observe if there was any bleeding. It was observed no bleeding, as seen in figures 10, 11 and 12. To date, no complications were observed in any patients after at least eight post-operatory months.

Figure 10: Scar of the first incision after one week.

Figure 11: Scar of the second incision after one week. The scar on the dorsum of the foot can also be seen without any oedema.

Figure 12: Scar of the third incision after one week.
Discussion
Wide-awake local anesthesia no-tourniquet (WALANT) surgery is an attractive option for hand surgeons and peripheral nerve surgeons [1]. Common peroneal neuropathy is the most common compressive neuropathy in the lower limb and should be included in the differential diagnosis for patients presenting with foot drop, chronic pain in the lower limb, or numbness of the lower extremity [6].
Symptoms of peroneal neuropathy may occur due to compression of the common peroneal nerve (CPN), superficial peroneal nerve (SPN), or deep peroneal nerve (DPN), each with different clinical presentations. Tarsal tunnel syndrome affects the tibial nerve (TN) and is a cause of chronic pain and numbness on the medial side of the ankle and the foot [7]. Impaired glucose tolerance creates a peripheral nervous system that is susceptible to chronic nerve compression. While it is accepted that surgical decompression of the median nerve at the wrist for carpal tunnel syndrome is appropriate in the diabetic, the application of this concept to the lower extremity has not yet gained widespread recognition [7].
Many diabetic patients have other comorbilities, turning them into difficult patients to treat. The risk of occult or hard to diagnose vascular diseases also is high, and this risk may prevent the use of a tourniquet in the lower limbs. It is known that any level of surgical trauma can lead to a physiological stress response involving the hypothalamic-pituitary-adrenal axis. The resultant hormone releases can have negative effects on glucose homeostasis [8]. This fact may increase the difficulties for the surgeon when dealing with diabetic patients. WALANT surgery is a common practice nowadays with a low risk of complications [9,10].
Considering this approach and the safety of WALANT surgery, the author began to apply WALANT for the decompression of the CPN, TN and DPN (the Dellon Triple decompression) [4,11] in superimposed nerve compressions to diabetic neuropathy patients. The procedure was considered safe, with an almost bloodless field and allowed full release of the affected nerves.
No complications were noted and all patients were followed up in a weekly basis until discharge. Decompression of superimposed nerve compressions in the diabetic patient with symptomatic neuropathy reliably relieves pain, restores sensation, and thereby prevents ulceration and amputation as noted by Dellon [7].
The application of WALANT technique has allowed the complete decompression of the peripheral nerves with no need to inflate the tourniquet, no need of additional anesthetic procedures and none case required the use of phentolamine to revert the vasoconstriction effect of epinephrine. The observed almost completely bloodless field in the three incisions during the three nerve decompressions as shown in the pictures is encouraging. A limitation of this study is that there were initially only 10 treated patients. The author considers this technique a promising technique that can be safely applied to a higher number of patients in indicated cases.
Conclusion
WALANT technique is a safe technique and may be a reliable tool to increase the number of diabetic patients suffering from chronic pain in the lower limbs related to superimposed nerve compressions to diabetic neuropathy that can be surgically treated with the release of the CPN, TN and DPN in diabetic neuropathy.
References
- Connors KM, Kurtzman JS, Koehler SM, et Successful Use of WALANT in Local and Regional Soft Tissue Flaps A Case Series. Plast Reconstr Surg Glob Open. 2023; 11: e4756.
- Bilgetekin YG, Kuzucu Y, Öztürk A, et al. The use of the wide awake local anesthesia no tourniquet technique in foot and ankle injuries. Foot Ankle Surg. 2021; 27: 535-538.
- Wei Y, Yun X, Liu Y, et al. Effectiveness of partial anterior cruciate ligament suture repair with wide awake local anesthesia no tourniquet technique. Chinese. 2021; 35: 337 342.
- Maiwulajiang Maimaijiang, Maimaiaili Yushan, Alimujiang Abulaiti, et al. Effectiveness of lower extremity Dellon triple nerve decompression in treatment of early stage diabetic Charcot foot. Chinese. 2020; 34: 1005-1011.
- Fakkel TM, Rinkel WD, Henk Coert J, et al. Does Lower Extremity Nerve Decompression Surgery Improve Quality of Life. Plast Reconstr Surg. 2022; 150: 1351-1360.
- Dellon Susceptibility of nerve in diabetes to compression implications for pain treatment. Plast Reconstr Surg. 2014; 134: 142S-150S.
- Dellon AL. Neurosurgical prevention of ulceration and amputation by decompression of lower extremity peripheral nerves in diabetic neuropathy update 2006. Acta Neurochir Suppl. 2007; 100: 149-151.
- Negus OJ, Watts D, Loveday DT, et Diabetes a major risk factor in trauma and orthopaedic surgery. Br J Hosp Med. 2021; 82: 1-5.
- Connors KM, Guerra SM, Koehler SM, et Current Evidence Involving WALANT Surgery. J Hand Surg Glob Online. 2022; 4: 452-455.
- Shahid S, Saghir N, Saghir R, et al. WALANT A Discussion of Indications Impact and Educational Requirements. Arch Plast Surg. 2022; 49: 531-537.
- Liao C, Li S, Nie X, et Triple nerve decompression surgery for the treatment of painful diabetic peripheral neuropathy in lower extremities A study protocol for a randomized controlled trial. Front Neurol. 2022; 13: 1067346.