ECG and Echocardiography Findings in Hypertension: A Comparative Study Male versus Female at the Gabriel Touré University Hospital (UH-GT)
Author(s): Bâ Hamidou Oumar1*,Sangaré Ibrahima1, Camara Youssouf2, Tchedre Tawoufik1, Kamaté Kassim1,Dakouo Réné-Marie1, Sidibé Noumou1, Sogodogo Adama1, Traoré A1, Camara Hamidou1 and Menta Ichaka1
1University Hospital “Gabriel Touré”, Bamako, Mali.
2University Hospital “Sidy Bocar Sall”, Kati, Mali.
3University Hospital “Mère-Enfant Le Luxembourg”, Bamako, Mali.
4University Hospital “Hôpital du Mali”, Bamako, Mali.
5University Hospital “Yalgado Ouédraogo”, Ouagadougou, Burkina Faso.
6University Hospital “Point G”, Bamako, Mali.
*Correspondence:
Hamidou Oumar BA, University Hospital “Gabriel Touré”, Bamako, Mali, Phone: +223 66 71 95 11.
Received: 17 May 2024; Accepted: 22 Jun 2024; Published: 28 Jun 2024
Citation: Oumar BH, Ibrahima S, Youssouf C, et al. ECG and Echocardiography Findings in Hypertension: A Comparative Study Male versus Female at the Gabriel Touré University Hospital (UH-GT). Cardiol Vasc Res. 2024; 8(1): 1-5.
Abstract
Background: There is a lack of data on ECG and echocardiographic modifications in hypertensive patients in our setting that justify their inclusion.
Methods: This study aims to compare induced ECG and echocardiographic modifications in female and male hypertensive patients. It was a cross-sectional study among outpatients seen in the cardiology department of the UH-GT in Bamako-Mali and included hypertensive patients aged 18 years or older.
Data were first collected on a survey form, inserted into a MS Access database, and finally analyzed with IBM SPSS software. Quantitative data are presented as mean with standard deviation and qualitative data as proportion. The level of significance for the statistical test was set at 5%.
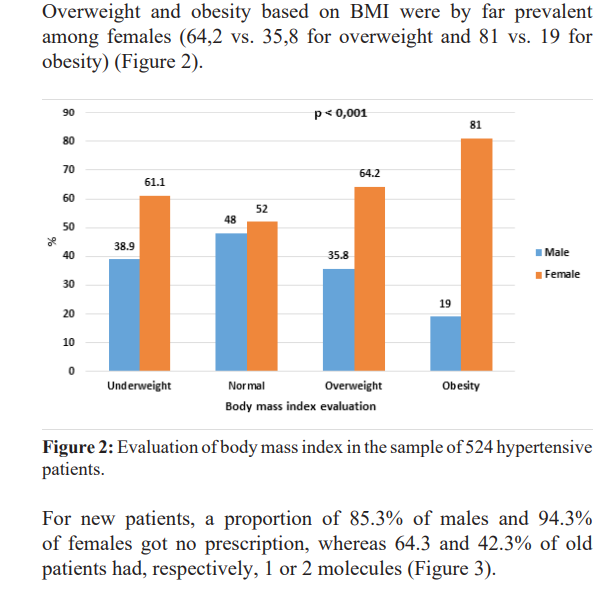
Results: Of 524 patients, 52.9% were new patients, and 96% had no known cardiac disease. The female sex represented 61.8%. The mean age was 55.33±15.013 years, and obesity based on body mass index was more prevalent in women's sex (81 vs. 19% in men's sex).
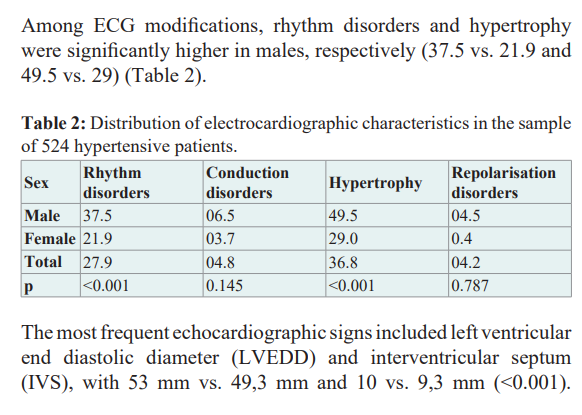
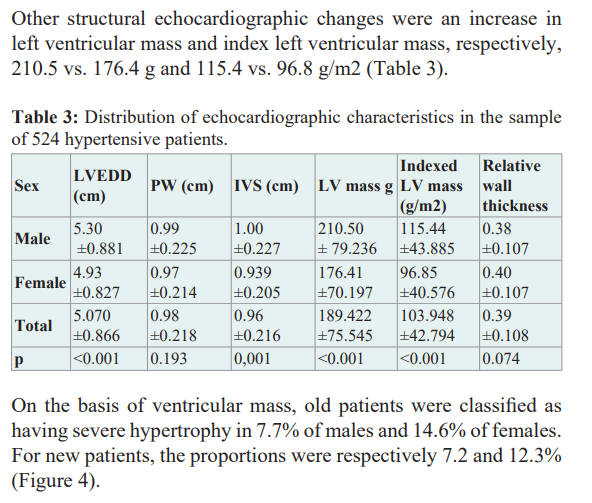
The global prevalence of HTN was 38.8% in males and 61.1% in females. Among ECG modifications, rhythm disorders and hypertrophy were significantly higher in males, respectively (37.5 vs. 21.9 and 49.5 vs. 29). The most frequent echocardiographic signs included left ventricular end diastolic diameter (LVEDD) and interventricular septum (IVS), with 53 mm vs. 49,3 mm and 10 vs. 9,3 mm (<0.001). Other structural echocardiographic changes were an increase in left ventricular mass and index left ventricular mass with, respectively, 210.5 vs. 176.4 g and 115.4 vs. 96.8 g/m2.
Conclusion: The prevalence of hypertension is high in both sexes, with consequences led by left ventricular hypertrophy in ECG and echocardiography. The higher prevalence of female HTN must be further studied, as must the associated factors.
Keywords
Background
Hypertension (HTN) has been a worldwide leading risk factor for cardiovascular diseases for decades [1-3]. The World Health Organization (WHO) named it “Silent Killer” [4] and estimated that there are near 1,3 billion adults living with HTN, most of whom live in low- and middle-income countries (LMICs) [5]. It affects all age groups, male and female [6-9], and also out of health facilities [10].
Despite a high prevalence, HTN is underdiagnosed [11], poorly controlled [12-16], and treated [17-19]. All that, plus the presence of severe HTN, particularly in low-income countries [20], leads most of the time to the development of target organ damage (TOD) that is associated with cardiovascular events [21].
Methods
There is a lack of data on the ECG and echocardiographic modifications of hypertensive patients in our setting, justifying this study, which aims to compare induced modifications in female and male genders.
Data were retrieved from a cross-sectional study from November 2022 to April 2023 in the cardiology department of the UH-GT.
Included were all patients aged 18 years or older seen in the outpatient unit with the diagnosis of hypertension.
The following definitions have been adopted:
Hypertension: patient with systolic blood pressure (SBP) 140 mmHg and/or diastolic blood pressure (DBP) 90 mmHg or patient taking antihypertensive drug therapy.
ECG left ventricular hypertrophy (LVH): Sokolow-Lyon voltage
(SV1 + RV5 or V6) ≥ 35 mV and Cornell voltage (SV3 + RaVL) > 20 mV for females and 28 for males.
LV mass and relative wall thickness (RWT) were calculated in accordance with the American Society of Echocardiography convention using the following corrected equations:
LV mass (g) = 0.80 × 1.04 [(LV end-diastolic diameter + septal wall thickness + posterior wall thickness)3 – (LV end-diastolic diameter)3] + 0.6 [22]
RWT = (septal wall thickness + posterior wall thickness)/LV end- diastolic diameter of the LV [23].
Echocardiographic LVH was defined as a LV mass index (LVMI: LV mass/body surface area) >150 g/m2 in men and >120 g/ m2 in women. The degrees of LVM abnormality were assessed according to the recommendations of the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE) [24].
All patients consented to be study participants after receiving clear information about the study and knowing that their caregiving would not be affected by their eventual refusal. Data collection has been done with all needed confidentiality rules.
Data were first collected on a survey form, inserted into a MS Access database, and finally analyzed with IBM SPSS software. Quantitative data are presented as mean with standard deviation and qualitative data as proportion. The level of significance for the statistical test was set at 5%.
Results
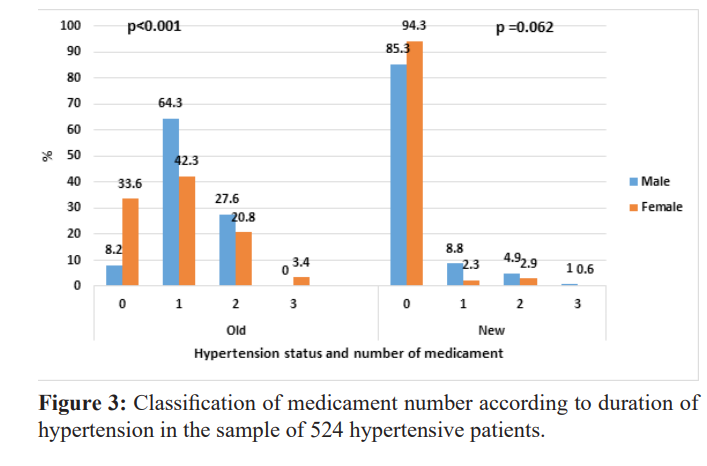
Our sample consisted of 524 patients from a population study of 990 patients (385 men and 605 women). A proportion of 52.9% were new patients, and 96% had no known cardiac disease. The female sex represented 61.8%.
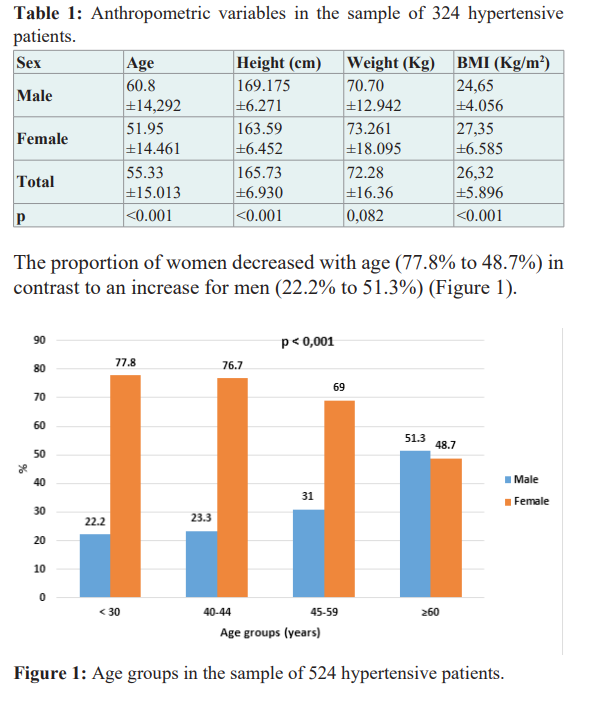
The sample mean age was 55.33±15.013 years (60.80± 14.292 for male sex and 51.95±14.461 for female sex). Male height was significantly higher than the higher body mass index (BMI) for females, with p<0.001 (Table 1).
Discussion
Our sample of 524 hypertensive patients stemmed from a population of 990 ambulatory patients seen during the study period, giving a global prevalence of HTN of 52.9%. Therefore, the prevalence of male HTN is 38.8% and that of female HTN is 61.1% of all visits. Our higher prevalence of female sex is rarely found in the literature except in older patients [25]. But global HTN is more prevalent in males [26].
HTN, as the main modifiable cardiovascular risk factor, can lead to clinical complications associated with ECG modifications and echocardiography. But even in the absence of complications, modifications can be seen in echocardiography [27,28] and TOD independently of the type of hypertension [21] and the course of symptoms [29]. It should be noted that the mechanistic common ground between chronic blood pressure elevation and cardiac disease likely begins early in life [30].
The results of this study on ECG and echocardiography revealed the following findings:
Male sex: higher ECG-LVH in males (Table 2), higher LVEDD, IVS, LVM, and LVMI (Table 3).
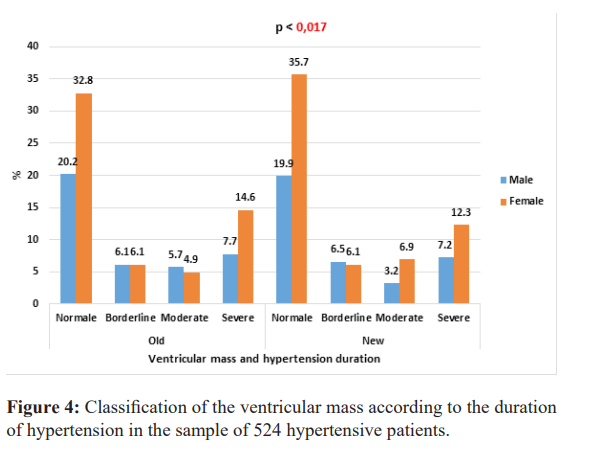
Female sex: higher RWT (Table 3), more severe echo-LVH as well in old as in new patients (Figure 4).
From the ECG abnormalities, LVH is the most important, despite the low sensitivity of the ECG [30-32]. ECG-LVH has a prognostic value [33,34] and is a stronger risk factor for cardiovascular events in women than in men [35,36]. In our study, LVH was more present in male subjects compared to data from south Asia [37] and could be explained by many other factors, including comorbidities [38,39], using criteria [40].
To improve the detection of LVH, echocardiography has long been the gold standard. Echo-LVH is assessed differently, partly explaining its various prevalences [22,41,42]. In our study, all ventricular parameters were higher in men compared to women. ECG-LVH could be absent, especially in low-risk patients, and its probability in echocardiography can be assessed using scores [43].
Limitations
As a cross-sectional study, we cannot look for a trend over time, especially through following new patients. Furthermore, not all patients underwent echocardiography and ECG to assess the sensitivity of the latter and refine the prevalence.
Conclusion
The prevalence of hypertension is high in both sexes, with consequences led by left ventricular hypertrophy in ECG and echocardiography. The higher prevalence of female HTN must be further studied, as must the associated factors.
Declarations
Ethics Approval and Consent to Participate
The study has been approved as part of the University Hospital’s research activities by the institutional board.
Informed consent has been obtained for all patients.
Author’s Contributions
BA HO designed the study. Poudiougou M was responsible for data collection. BA HO, Camara Y, Sangaré I, and Menta I were responsible for statistical analysis. BA HO and Poudiougou M wrote the first draught. Camara Y, Sangare I and Menta reviesswed and checked the manuscript. All authors approved the final version of the manuscript. All authors read and approved the final manuscript."
References
- Franklin SS, Wong ND. Hypertension and Cardiovascular Diseases: Contributions of the Framingham Heart Study. Glob Heart. 2013; 8: 49-57.
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet Lond Engl. 2017; 390: 2627-2642.
- Yusuf S, Joseph P, Rangarajan S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. The Lancet. 2020; 395: 795-808.
- https://www.who.int/cardiovascular_diseases/publications/ global_brief_hypertension/en/
- https://www.who.int/news-room/fact-sheets/detail/hypertensio n
- Bâ HO, Maiga AK, Teche YB, et al. Prévalence de l’HTA des enfants et adolescents au Centre Hospitalier Mère-Enfant le Luxembourg à Bamako. ScienceLib. 2015; 7: 17.
- http://www.panafrican-med-journal.com/content/ article/25/77/full/
- Wagner A, Dallongeville J, Ferrières J, et al. État des lieux sur l’hypertension artérielle en Franceen. 2007.
- Houehanou C, Amidou S, Preux PM, et al. Hypertension artérielle (HTA) en Afrique subsaharienne. JMV-J Médecine Vasc. 2018; 43: 87.
- Kusuayi Mabele G, Nkiama Ekisawa C, Delecluse C, et al. Évaluation de la prévalence de l’hypertension artérielle de l’adulte en milieu du travail à Kinshasa, République Démocratique du Congo. Sci Sports. 2018; 33: 213-220.
- Ataklte F, Erqou S, Kaptoge S, et al. Burden of Undiagnosed Hypertension in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Hypertension. 2015; 65: 291-298.
- Zhou B, Carrillo-Larco RM, Danaei G, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. The Lancet. 2021; 398: 957-980.
- Chobufo MD, Gayam V, Soluny J, et al. Prevalence and control rates of hypertension in the USA: 2017–2018. Int J Cardiol Hypertens. 2020; 6: 100044.
- Huang XB, Zhang Y, Wang TD, et al. Prevalence, awareness, treatment, and control of hypertension in southwestern China. Sci Rep. 2019; 9: 19098.
- Koya SF, Pilakkadavath Z, Chandran P, et al. Hypertension control rate in India: systematic review and meta-analysis of population-level non-interventional studies, 2001–2022. Lancet Reg Health - Southeast Asia. 2023; 9: 100113.
- https://oce.ovid.com/article/00004268-201804000-00013/HTML
- https://www.who.int/news/item/25-08-2021-more-than-700- million-people-with-untreated-hypertension
- Okello S, Muhihi A, Mohamed SF, et al. Hypertension prevalence, awareness, treatment, and control and predicted 10- year CVD risk: a cross-sectional study of seven communities in East and West Africa (SevenCEWA). BMC Public Health. 2020; 20: 1706.
- Ruben Turé, Albertino Damasceno, Mouhammed Djicó, et al. Prevalence, awareness, treatment, and control of hypertension in Bissau, Western Africa. J Clin Hypertens Greenwich Conn. 2022; 24: 358-361.
- Ngongang Ouankou C, Chendjou Kapi LO, Azabji Kenfack M, et al. Hypertension artérielle sévère nouvellement diagnostiquée dans un pays en Afrique sub-saharienne : aspects épidemio-cliniques, thérapeutique et évolutifs. Ann Cardiol Angéiologie. 2019; 68: 241-248.
- Tientcheu DD, Ayers C, Das S, et al. Target organ complications and cardiovascular events associated with masked hypertension and white coat hypertension: analysis from the dallas heart study. J Am Soc Hypertens. 2015; 9: e1.
- Levy D, Savage DD, Garrison RJ, et al. Echocardiographic criteria for left ventricular hypertrophy: The Framingham heart study. Am J Cardiol. 1987; 59: 956-560.
- Ganau A, Devereux RB, Roman MJ, et al. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992; 19: 1550-1558.
- Marwick TH, Gillebert TC, Aurigemma G, et al. Recommendations on the use of echocardiography in adult hypertension: a report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). Eur Heart J - Cardiovasc Imaging. 2015; 16: 577-605.
- Ninios I, Ninios V, Lazaridou F, et al. Gender-Specific Differences in Hypertension Prevalence, Treatment, Control, and Associated Conditions among the Elderly: Data from a Greek Population. Clin Exp Hypertens. 2008; 30: 327-337.
- Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020; 16: 223-237.
- Cuspidi C, Facchetti R, Bombelli M, et al. High Normal Blood Pressure and Left Ventricular Hypertrophy Echocardiographic Findings From the PAMELA Population. Hypertension. 2019; 73: 612-619.
- https://oce.ovid.com/article/00004872-201806001-00697/HTML
- Rosei EA, de Simone G, Mureddu G, et al. Arterial Hypertension and Cardiac Damage. High Blood Press Cardiovasc Prev. 2008; 15: 141-170.
- Lawler PR, Hiremath P, Cheng S. Cardiac Target Organ Damage in Hypertension: Insights from Epidemiology. Curr Hypertens Rep. 2014; 16: 446.
- Hartog-Keyzer JML de, Messaoudi SE, Harskamp R, et al. Electrocardiography for the detection of left ventricular hypertrophy in an elderly population with long-standing hypertension in primary care: a secondary analysis of the CHELLO cohort study. BMJ Open. 2020; 10: e038824.
- Pewsner D, Jüni P, Egger M, et al. Accuracy of electrocardiography in diagnosis of left ventricular hypertrophy in arterial hypertension: systematic review. BMJ. 2007; 335: 711.
- Ang DSC, Lang CC. The prognostic value of the ECG in hypertension: where are we now?. J Hum Hypertens. 2008; 22: 460-467.
- Schillaci G, Battista F, Pucci G. A review of the role of electrocardiography in the diagnosis of left ventricular hypertrophy in hypertension. J Electrocardiol. 2012; 45: 617- 623.
- Porthan K, Niiranen TJ, Varis J, et al. ECG left ventricular hypertrophy is a stronger risk factor for incident cardiovascular events in women than in men in the general population. J Hypertens. 2015; 33: 1284-1290.
- Boivin JM, Koch C, Vigié L, et al. Prévalence de l’atteinte des organes cibles chez des patients traités pour une HTA: comparaison homme/femme. Étude ESSENTIELLE. Ann Cardiol Angéiologie. 2015; 64: 150-157.
- Feng L, Khan AH, Jehan I, et al. Sex disparity in left ventricular hypertrophy in South Asians with hypertension: influence of central obesity and high blood pressure. J Hum Hypertens. 2023; 37: 327-329.
- Haukilahti Ma E, Kentta TV, Kiviniemi AM, et al. Sex differences in prevalence of electrocardiographic and echocardiographic left ventricular hypertrophy among patients with coronary artery disease. Eur Heart J. 2022.
- Bruno G, Giunti S, Bargero G, et al. Sex-differences in prevalence of electrocardiographic left ventricular hypertrophy in Type 2 diabetes: The Casale Monferrato Study. Diabet Med. 2004; 21: 823-828.
- https://login.research4life.org/tacsgr1www_ahajournals_org/ doi/epdf/10.1161/01.CIR.75.3.565
- Yildiz M, Oktay AA, Stewart MH, et al. Left ventricular hypertrophy and hypertension. Prog Cardiovasc Dis. 2020; 63: 10-21.
- Liebson PR, Grandits G, Prineas R, et al. Echocardiographic correlates of left ventricular structure among 844 mildly hypertensive men and women in the Treatment of Mild Hypertension Study (TOMHS). Circulation. 1993; 87: 476-486.
- Mancusi C, Angeli F, Verdecchia P, et al. Echocardiography in Low-Risk Hypertensive Patients. J Am Heart Assoc. 2019; 8: e013497.