Effect of an Anti-Reflux Bed Wedge on Gastro esophageal Reflux Symptoms and Acid Reflux
Author'(s): Andrea Oliveira Batista1, Fernando Cesar Ferreira Pinto2, and Roberto Oliveira Dantas3*
1Department of Ophthalmology, Otorhynolaryngology and Head and Neck Surgery, Ribeirão Preto Medical School - University of São Paulo, Ribeirão Preto SP, Brazil.
2Surgery Institute, Ribeirão Preto SP - Brazil.
3Department of Medicine, Ribeirão Preto Medical School - University of São Paulo, Ribeirão Preto SP, Brazil.
*Correspondence:
Roberto Oliveira Dantas, Ribeirão Preto Medical School - University of São Paulo, Av. Bandeirantes, 3900 Campus da USP, 14049-900 Ribeirão Preto, SP Brazil, Tel: 55.16.36022457 Fax: 55.16.36020229, ORCID: 0000-0003-2183-0815.
Received: 04 December 2020 Accepted: 27 December 2020
Citation: Batista AO, Pinto FCF, Dantas RO. Effect of an Anti-Reflux Bed Wedge on Gastroesophageal Reflux Symptoms and Acid Reflux. Gastroint Hepatol Dig Dis. 2020; 3(2): 1-5.
Abstract
Background and Aim: Gastro esophageal reflux disease is common in the population, with a long pharmacological and non-pharmacological treatment. One of the non-pharmacological treatments is the elevation of the head of the bed to avoid gastro esophageal reflux when the patients are in the supine position. The objective of this investigation was to evaluate the effects of two bed wedges placed over a flat mattress on symptoms and acid reflux.
Patients and Methods: Two bed wedges were placed over a flat mattress, one with 18 cm depth (5.5° inclination, wedge-1) and the other with 28 cm depth (8.6° inclination, wedge-2) and evaluated the effect on symptoms and gastro esophageal reflux. The bed wedge-1 was tested in 12 patients and the bed wedge-2 in 25 patients. All patients were assessed for symptoms, and underwent upper digestive endoscopy and 48-hour pH monitoring. The pH was measured continuously 5 cm proximal to the lower esophageal sphincter for 48 hours – 24 hours on a bed wedge (18 cm or 28 cm depth) and 24 hours without a bed wedge (i.e., on a flat mattress), in a random order.
Results: Both bed wedges reduced the frequency of gastro esophageal reflux symptoms in the supine position compared with the flat mattress. Bed wedge-2 caused more discomfort during the night than the wedge-1. The pH monitoring measurements were not different between the two wedges.
Conclusions: The bed wedges tested reduced the frequency of symptoms, but had no effect on gastro esophageal acid reflux. The 28 cm-depth wedge caused discomfort in supine position in most its users.
Keywords
Introduction
Gastro esophageal reflux disease (GERD) is a common condition in the population, which causes heartburn and acidic regurgitation. Heartburn may be exacerbated by the supine position and bending over, causing sleeping difficulties, which may decrease the threshold for symptoms perception [1]. Clinical treatment may be prescribed based on symptoms. However, in the presence of alarm symptoms (dysphagia, anemia, bleeding, weight loss) or atypical symptoms (chest pain, laryngopharyngeal symptoms) an upper endoscopy is important, which may be followed by 24-hours esophageal pH acidic reflux monitoring or 24-hour- of pH/impedance acid and non-acid reflux monitoring [2]. New diagnostic tests for GERD have been proposed, such as narrow band imaging, mean nocturnal baseline impedance, salivary pepsin concentration and esophageal mucosal impedance [3].
Treatment of GERD consists of acid suppression by proton pump inhibitors or, less frequently, by H2 blockers, and non- pharmacological anti-reflux management, including anti-reflux surgery, weight loss for obese patients, lifestyle and dietary changes, as to avoid late-night meals and elevation of the head of the bed [4,5].
Elevation of the head of the bed may be important for some patients, mainly for those with nocturnal and extra-esophageal symptoms, situation that cause significant impairment of the quality of life [4]. Head of the bed elevation decreased from 21% to 15% the time of acid exposure in the supine position compared with flat position [5]. Elevation of head of the bed with blocks of 28 cm decreased the time the pH was below five, the number of reflux episodes, and acid clearance time, leading to symptomatic benefit [6]. However, the frequency of reflux episodes remained unchanged [7].
In a comparison of three sleeping positions – elevation of the head of the bed on bed blocks, elevation by a foam wedge and flat position – there was no difference in reflux frequency between the positions, but the wedge caused a decrease in the time that distal esophageal pH was less than 4, and also decreased the longest episode experienced by the patients [8]. This investigation suggested that elevation of the head of the bed can decrease esophageal exposure to acid but the effect of different methods of head-of-bed elevation on gastro esophageal reflux is not the same. One controversial issue is the ideal height of bed head elevation to achieve the desired effects.
The aim of this study was to evaluate the effects of two bed wedges (18 cm and 28 cm depth) placed over a conventional flat mattress, on symptoms and gastro esophageal acid reflux of patients with GERD. The hypothesis was that the bed wedge would reduce GERD symptoms in the supine position and the occurrence of gastro esophageal acid reflux.
Patients and Methods
Two bed wedges were tested in patients with heartburn and acid regurgitation for more than one year and more than three times a week, one 18 cm depth and the other 28 cm depth (DK Furniture, Brazil). The bed wedges covered the complete length and width of the bed, and was placed over the existing, conventional flat mattress, resulting in a tilt of 5.5o and 8.6o, respectively (Figure 1). The volunteers had the option to use a pillow.
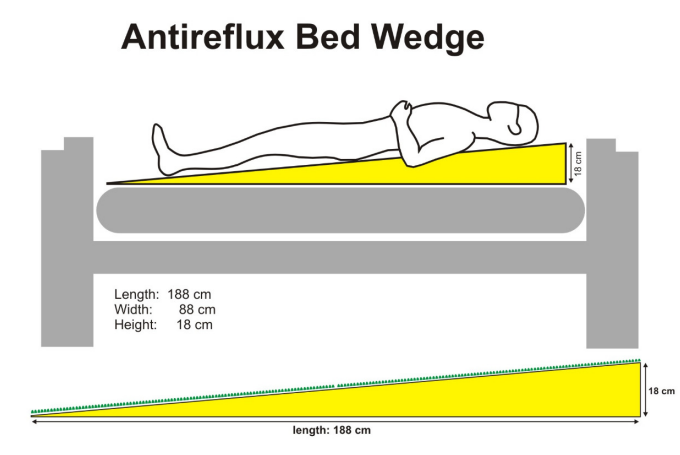
Figure 1: Illustration of the bed wedge of 18 cm, placed over the conventional flat mattress and its dimension.
The effects of wedge-1 (18 cm) was tested in 12 patients (10 men), aged 39 ± 12 years (25-63 years), body mass index (BMI) 27.3 ± 2.0 kg/m2 (17.6 -39.3 kg/m2). Endoscopic diagnosis and grading of reflux esophagitis, according to the Los Angeles classification [9], revealed that three patients had grade an esophagitis (LA- A), five LA-B, one LA-C, one LA-D and two patients had non- erosive reflux disease (NERD) [2]. The effects of wedge-2 (28 cm) was tested in 25 patients (five men), aged 47 ± 13 years (21-67 years), BMI 27.5 ± 3.1 kg/m2 (19.7 -39.6 kg/m2). Five patients had esophagitis, one with LA-A, three LA-B, one LA-C, and 20 with NERD.
Each patient answered the health-related quality of life scale (GERD-HRQL) proposed by Velanovich et al [10,11], which has a maximal score of 50, and the eating assessment tool (EAT-10) to assess dysphagia [12-14], which has a maximal score of 40. The study was approved by the Research Ethics Committee of the tertiary care Ribeirão Preto Medical School University Hospital, IRB number 12220/2016, and registered at the Brazilian Clinical Trials Registry (RBR-58vsqp). Written informed consent was obtained from all participants. Their anonymity was protected.
After at least seven days of discontinuation of GERD treatment with proton pump inhibitors and/or H2 blockers and 6 hours of fasting, the patients were submitted to 48-hour pH monitoring. Patients included in the evaluation of wedge-1 were submitted to esophageal manometry for identification of the gastro esophageal junction, and in patients included in the evaluation of wedge-2 gastro esophageal junction was identified by the pH change (from acid to neutral). Previously calibrated pH catheter with a distal pH sensor (ALACER Biomedica, SP, and Brazil) was introduced via the nostril. In the wedge-1 group, the pH sensor was placed 5 cm from the upper border of the lower esophageal sphincter (LES) determined by esophageal manometry and, in the wedge-2 group, the pH sensor was placed 5 cm from the changing point from acidic to neutral pH during the continuous withdrawal of the catheter. After pH catheter placement, patients were taken to the clinical research ward of the hospital, where they stayed for 48 hours. In a random sequence, patients used a flat mattress alone or a bed wedge that was placed over the flat mattress, for 24 hours each. In the morning following each 24-hour period, each participant reported the time of the meals, the time they were in supine or in upright positions and the symptoms when in supine position, and if they had a comfortable or uncomfortable night. They did not take any medication during the pH monitoring.
Patients were given a 2,000 - calorie diet daily, providing 273 g of carbohydrate, 85 g of protein and 68 g of fat, at pre-established times: 8:30 am – breakfast, 12:00 (noon) – lunch, 3:00 pm snack, 6:30 pm – dinner, 9:00 pm – snack.
After 48 hours of pH monitoring, the results were downloaded to a computer and analyzed. The 48-hour recordings were divided into two periods of approximately the same duration, started just before the breakfast of each day. Reflux was considered when the pH decreased to below 4. Along with the results of the 24 hours pH monitoring the following parameters were assessed when patients were in supine position: presence of symptoms, number of acid reflux episodes, number of prolonged reflux (longer than 5 minutes) episodes, duration of the longest reflux, in minutes, the time the esophageal pH was below 4, in minutes, the percentage of time when the pH was below 4, the number of reflux episodes per hour, and acid clearance time (minutes/reflux). The results were compared between the two study days (flat mattress vs. wedge-1 or flat mattress vs. wedge-2).
Statistical analysis
The statistical analysis was performed using the mixed-effects linear model (random and fixed effects) [15], controlled for the duration of the test. The variables percentage of time with reflux, the number of reflux episodes per hour and the DeMeester score were evaluated by the Student’s t-test. Differences with p<0.05 were considered significant. The results are expressed in number, percentage, mean and standard deviation (SD).
Results
Mean GERD-HRQL score was 39.8 ± 12.2 among individuals in the wedge-1 group and 35.2 ± 8.6 in the wedge-2 group (p>0.05).
Mean EAT-10 scores were 11.4 ± 9.8 and 13.8 ± 11.8 in the wedge-1 and wedge-2 groups, respectively (p>0.05). Seven patients (58%) in the wedge-1 group and 16 (64%) in the wedge-2 group had EAT-10 scores ≥5, an indication that they had perceived dysphagia.
In both groups, no difference in the 24 hours of pH monitoring between the day with flat mattress and the day with wedge was found in the DeMeester score, percentage of supine reflux time, percentage of time when the esophageal pH was below 4, and in duration of supine pH monitoring (p>0.05, Table 1).
When the individuals were in the supine position with the wedge-1 there was a decrease in the number of patients with heartburn, regurgitation, respiratory difficult, cough, throat clearing and insomnia (p≤0.03, Table 2). When in the use of the wedge-2, in the supine position, there was a decrease in the number of patients with regurgitation, choking, respiratory difficult, and insomnia (p≤0.04, Table 3).
While wedge-1 had no effect on comfort when in supine position during the night (Table 2), the proportion of patients who felt comfortable in supine position during the night decreased from 68% to 28% with the use of the wedge-2 (p=0.02, Table 3).
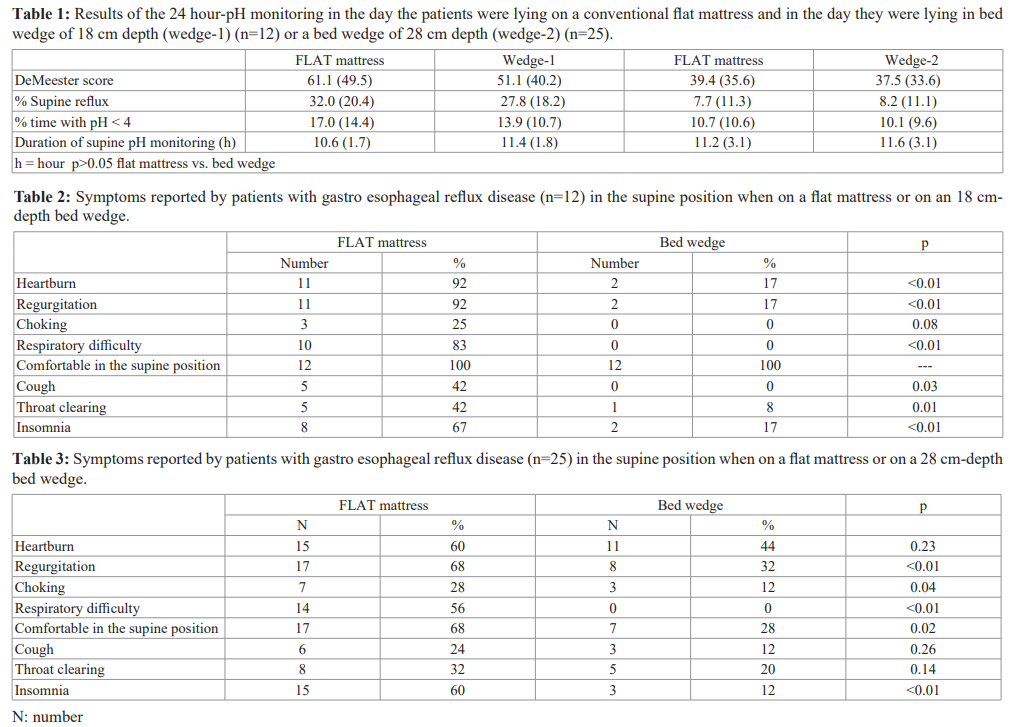

During supine position, no difference in the pH monitoring parameters were found between the use of the flat mattress and the bed wedges (p>0.05, Table 4).
Discussion
The 24-hour pH monitoring is a highly sensitive and specific method for evaluation of acid gastro esophageal reflux [16]. Supine reflux was assessed following the same procedures with patient lying either on a flat mattress or on the mattress wedge. Results of pH measurements may be different when performed on consecutive days individually; however mean values of the group were not different between the study days [17]. The mattress wedge did not significantly affect the pH monitoring parameters, as these were not significantly different between the day the patient used the flat mattress and the day the patient used the wedge (1 or 2).
Patients in the wedge-1 group showed more intense gastro esophageal reflux (mean percentage of time when the pH was below 4 of 17.0% on one day and 13.9% the other day) than the wedge-2 group (10.7% and 10.1% respectively). Esophagitis was present in 83% of patients in the wedge-1 group and 20% in the wedge-2 group and the symptoms were more frequent among patients who tested the wedge-1.
The assessment of symptoms using the GERD-HRQL scale indicated that a considerable proportion of patients complained of gastro esophageal reflux symptoms. The scale has a variation from 0 to 50, and the averages of both groups were in the upper third of the scale. For evaluation of dysphagia, an EAT-10 ≥5 was used to define dysphagia [14], which showed that 62% of the patients had perception of the symptom. Both GERD-HRQL and the EAT-10 score indicated that the patients had important symptoms related to GERD.
Both wedges reduced the frequency of symptoms in patients when in supine position. This is in accordance with previous reports showing that elevation of the head of the bed reduces the severity of their symptoms [18], although others reported that this practice is not effective in this regard [19]. In the present study, reduction of symptoms was more pronounced in the wedge-1 group, which may be explained by the more severe disease of these patients. The higher inclination of the bed (promoted by the wedge-2) was not associated with higher absence of symptoms, but did cause more discomfort, reported by 78% of the patients in the wedge-2 group, which should be balanced against the overall benefit to the patient.
As mentioned above, the use of the bed wedges had no significant effect on the pH monitoring parameters used to assess acid gastro esophageal reflux. Previous investigations described that head of bed elevation is a correct treatment to decrease gastro esophageal reflux [4-6], however, others showed that the number of reflux episodes in supine position did not change with the elevation [7,8]. Another study showed that elevation of the head of the bed by a foam wedge decreased the time that the distal esophageal pH was <4 compared to the flat position and reduced the longest episode of reflux [8], but comfort when sleeping on the wedge was not evaluated.
This study has limitations. The positioning of the pH catheter in the wedge-2 group was not determined by manometry, and the possibility that the sensor was positioned slightly below or above the standard place cannot be excluded [20]. However, since pH monitoring on the two days was performed with the pH sensor in the same position, a possible error in the sensor positioning did not affect the interpretation of results. The number of patients in the wedge-1 group was small, but we believe it was sufficient to draw meaningful conclusions, that would not be changed by an increase in the number of patients. In addition, the wedge-2 group was older than the wedge-1 group, but the difference was not statistically significant and may not have influenced the results. Finally, elevation of the head of the bed is indicated mainly for patients with severe symptoms at night, which was not the case of our patients. Also, being in the supine position does not imply that the patient was sleeping. Patients with Barrett’ esophagus has a significant higher esophageal acid exposure especially in the supine position [21], and should be the focus of further studies.
Conclusion
In conclusion, the use of bed wedges that elevated the head of the bed by 18 cm or 28 cm reduced the frequency of gastro esophageal reflux symptoms in the supine position of GERD patients, but did not reduce reflux. Elevation of the head of bed by 28 cm caused patients’ discomfort during the sleeping period compared with elevation by 18 cm.
Acknowledgements
The authors are grateful to Francisco Alves de Souza, DK Móveis e Colchões, Ribeirão Preto, and ALACER Biomedical for their support to the investigation.
Funding
Andrea Oliveira Batista received a fellowship from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) – Brazil.
Authors’ contributions
Andrea O Batista and Roberto O Dantas participated in the study planning, data collection, discussion of results, manuscript preparation and the decision to submit the manuscript for publication. Fernando C Ferreira Pinto participated in data collection, discussion of the results, manuscript preparation and the decision to submit the manuscript for publication.
References
- Richter JE, Rubenstein Presentation and epidemiology of gastro esophageal reflux disease. Gastroenterology. 2018; 154: 267-276.
- Kandulski A, Moleda L, Müller-Schilling Diagnostic investigations of gastro esophageal reflux disease who and when to refer and for what test? Visc Med. 2018; 34: 97-100.
- Vaezi MF, Sifrim D. Assessing old and new diagnostic tests for gastro esophageal reflux disease. Gastroenterology. 2018; 154: 289-301.
- Yadlapati R, DakhoulL, Pandolfino JE, et al. The quality of care for gastro esophageal reflux disease. Dig Dis Sci. 2017; 62: 569-576.
- Ness-Jensen E, Hveem K, El-Serag H, et Lifestyle intervention in gastro esophageal reflux disease. Clin Gastroenterol Hepatol. 2016; 14: 175-183.
- Stanciu S, Bennett JR. Effect of posture on gastro-esophageal Digestion. 1977; 15: 104-109.
- Johnson LF, DeMeester TR. Evaluation of elevation of the head of the bed, bethanechol, and antacid foam tablets on gastro esophageal Dig Dis Sci. 1981; 26: 673-680.
- Hamilton JW, Boisen RJ, Yamamoto DT, et al. sleeping on a wedge diminishes exposure of the esophagus to refluxed Dig Dis Sci. 1988; 33: 518-522.
- Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of esophagitis clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999; 45: 172-180.
- Velanovich V, Vallance SR, Guz JR, et Quality of life scale for gastro esophageal reflux disease. J Am Coll Surgery. 1996; 183: 217-224.
- Fornari F, Gruber AC, Lopes AB, et Questionário de sintomas na doença do refluxo gastroesofágico. Arq Gastroenterol. 2004; 41: 263-267.
- Belafsky PC, Mouadeb DA, Rees CJ, et Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008; 117: 919-924.
- Gonçalves MI, Remaili CB, Behlau Cross-cultural adaptation of the Brazilian version of the Eating Assessment Tool EAT-10. CoDAS. 2013; 25: 601-604.
- Batista AO, Nascimento WV, Cassiani RA, et al. Prevalence of non-obstructive dysphagia in patients with heartburn and Clinics. 2020; 75: e-1556.
- Schall Estimation in generalized linear models with random effects. Biometrika. 1991; 78: 719-727.
- Jamieson JR, Stein HJ, DeMeester TR, et Ambulatory 24-h esophageal pH monitoring normal values, optimal thresholds, specificity, sensitivity, and reproducibility. Am J Gastroenterol. 1992; 87: 1102-1111.
- Batista AO, Dotti AZ, Aprile LRO, et al. Intra-esophageal pH monitoring on two consecutive days in patients with gastro esophageal reflux symptoms. Gastroenterol Res. 2019; 12: 198-202.
- Dagli U, Kalkan IH. The role of lifestyle changes in gastro esophageal reflux disease treatment. Turk J Gastroenterol. 2017; S33-S37.
- Kaltenbach T, Crockett S, Gerson LB. Are lifestyle measures effective in patients with gastro esophageal reflux disease? An evidence-based approach. Arch Intern Med. 2006; 166: 965-
- Nasi A, Frare RC, Brandão JF, et Estudo prospective comparativo de duas modalidades de posicionamento do sensor de pHmetria esofágica prolongada por manometria e pela viragem do pH. Arq Gastroenterol. 2008; 45: 261-267.
- Fass R, Teramoto O, Kurin M, et al. Esophageal function abnormalities in patients with Barrett’s J Clin Gastroenterol. 2020; 54: 485-492.