Endometrial Volume Assessment by VOCAL as a Predictor of The Success Rate of ART
Author'(s): Wael S Nossair*
M.D. of obstetrics and gynecology, faculty of medicine, Zagazig University, Egypt.
*Correspondence:
Wael S Nossair, M.D. of Obstetrics and Gynecology, Faculty of Medicine, Zagazig University, Egypt, E-mail: mohammedelsokkary1@yahoo.com.
Received: 02 May 2017 Accepted: 26 May 2017
Citation: Wael S. Nossair. Endometrial Volume Assessment by VOCAL as a Predictor of The Success Rate of ART. Gynecol Reprod Health. 2017; 1(1): 1-5.
Abstract
Objective: To explore the role of estimating endometrial volume by Virtual Organ Computer-aided AnaLysis (VOCAL) and it's correlation with endometrial thickness, on the day of hCG, in prediction of IVF/ICSI success.
Patients and Methods: It was a prospective study that was carried out at Zagazig University Hospitals, and Agial Fertility Center. Endometrial thickness and volume were measured in women undergoing an IVF/ICSI cycle, on the day of HCG, using the 3D transvaginal ultrasound probe. women were divided as regards to endometrial volume calculated into 3 subgroups; < 3ml, 3-5ml, and >5ml, also according to endometrial thickness into 3 groups; <7mm, 7-12mm and >12mm. Success rate of IVF/ICSI was compared between all groups.
Results: the number of pregnancies and pregnancy rates in each subgroup and differences were found to be non significant. A non-significant difference in the mean endometrial volume but significant mean endometrial thickness in the pregnant as compared to the non-pregnant group.
Conclusions: Endometrial thickeness on day of hCG is a better predictor of success rate of IVF/ICSI cycles than endometrial volume.
Keywords
Introduction
There are many causes of infertility. In the majority of couples, an apparent male or a female factor explaining their failure to conceive is usually present, in 10-25% there will be no explanation. Within this cohort of women there is a spectrum of diseases ranging from those women with a decreased fertility that will get pregnant with time to those in whom pregnancy is very difficult with available medical practice [1].
Pregnancy in In Vitro Fertilization (IVF) / intracytoplasmic sperm injection (ICSI) programs needs embryos of good quality and a receptive endometrium [2]. Despite the outstanding progress in these techniques, the implantation rate per embryo is constant at very low at 20% [3]. While the evaluation of quality of embryos and correct grading is performed in the lab before transfer, the evaluation of uterine lining receptivity is somewhat difficult. Transvaginal sonogram (TVS) is an ideal non-invasive technique, but with deficient specificity [2-4].
The utilization of 3D ultrasonography to test the details of the uterine cavity surpasses the diagnostic ability of Two Dimensional (2D) ultrasound [5,6]. There is a rising trend to utilize noninvasive methods as TVS, to assess the endometrial thickness, diagnose dysfunctional uterine bleeding (DUB), adenomyosis, endometrial polyps & fibroids [7]. Another important potential of 3D TVS is volume calculation utilizing the Virtual Organ Computer-aided AnaLysis (VOCAL) even in irregularly shaped organs. This technique has been shown to be more precise than 2D-volume estimation [5].
Many studies have stated a high level of reproducibility and accuracy of endometrial volume measurement using 3D ultrasound [8-9]. The aim of this study was to evaluate endometrial volume measured by VOCAL, on the day of human chorionic gonadotrophin (hCG), to endometrial thicknes in the prediction of IVF/ICSI success.
Patients and Methods
This was a prospective study performed at Zagazig University Hospitals, and Agial Fertility Center, and included 144 women who were presented for having unexplained infertility and were scheduled for IVF/ICSI done using ejaculate sperms. This study is performed over a 2-year period, between Jan 2015 and Jan 2017. Endometrial thickness and volume were measured in women undergoing an IVF/ICSI cycle, on the day of HCG, using the 3D transvaginal ultrasound probe. women were divided as regards to endometrial volume calculated into 3 subgroups; <3ml, 3-5ml, and >5ml. Also according to the thickness of the endometrium they were divided into 3 groups; <7mm, 7-12mm and >12mm. Success rate of IVF/ICSI was compared between all groups.
Inclusion criteria:
- Women under 40 year old.
- Women with unexplained infertility.
Exclusion criteria:
- Loss to follow-
- Any patient with uterine abnormality was excluded (e.g. fibroid, mullerian anomaly).
- Patients with a previous poor
- Those with difficult embryo transfer response.
- Women with a known systemic disease
- Women with more than 3 failed IVF
Informed consent was taken from every women, after they were fully discussed about the nature, scope the potential risks of this clinical trial.
Ovulation induction protocol used was the long luteal phase agonist protocol. Women received Decapeptyl 0.1 mg/day starting on day 20 of the cycle till the day of hCG intake. After down regulation, daily 150- 300 IU of human menopausal gonadotrophin (hMG) was commenced for 7 days, then the needed dose was given according to the follicular response. 10.000 units of hCG (Pregnyl; Nile CO., Cairo Egypt) were administered I.M. when more than two follicles reached 17mm in mean diameter. Ovum pickup (OPU) using transvaginal ultasound was performed 36 hour after hCG intake [10].
Embryo transfer was performed on day 5 after OPU using the Wallace catheter (H.G.Wallace Ltd, West Sussex, UK). Daily progesterone injection (100 mg, progesterone; Steris, Phoenix, AZ, USA) was given for luteal phase support. A serum B-hCG test was performed to check pregnancy two weeks after embryotransfer. Clinical pregnancy was diagnosed 3 weeks after a positive test by the presence of a gestational sac with fetal echoes and pulsations on ultrasound.
Endometrial evaluation on the day of hCG intake
The patients were checked using the TV 3D probe, the endometrial thickness was assessed at the maximum thickness between the highly reflective interfaces of the endometrial-myometrial junction [8]. Three-dimensional volumetry was done with an empty bladder, the patient was examined at the Special Care Center Of The Fetus by the same sonographer in the lithotomy position using Voluson Pro 720 GENERAL ELECTRIC USA, transducer with frequency range 5-8 MHZ. Sonar is done to study uterine size, shape and exclusion of any uterine or ovarian pathology. The 3D image was obtained by switching on the 3D volume mode and defining the region of interest by a movable sector on the screen. This sector has the shape of a truncated cone which can be manipulated to ensure that the whole of the endometrial cavity was included in the volume sampling while the patient remain still and the probe is held stationary. Volume sampling lasted about 4 seconds, during that time the conventional 2D plane was rotated through 180áµ? with the rotation axis oriented exactly along the longitudinal axis of the vaginal probe.
The data was stored digitally on the internal disc drive for subsequent analysis after the ultrasound probe is removed. For the purpose of volume calculation, 3D data was retrieved and presented in multi-planer display mode which simultaneously displays 3 perpendicular planes on the screen. The actual volume was calculated by the built-in computer program using VOCAL. This is a rotational method based on rotation in given steps (6,9,15,30) on a given orthogonal plane (A,B OR C). The endometrial volume was measured in plane A by delineating the endometrial margin at the endometrial-myometrial interface from the fundus to the internal cervical os in a number of parallel slices which are 1-2 mm apart [8].
The hospital ethics committee approved the study. All patients gave their informative consent before entering into the study.
Statistical analysis: Retrieved data were recorded on an investigative report form. The data were analyzed with SPSS® for Windows®, version 15.0 (SPSS, Inc, USA). Significance level was set at 0.05.
Results
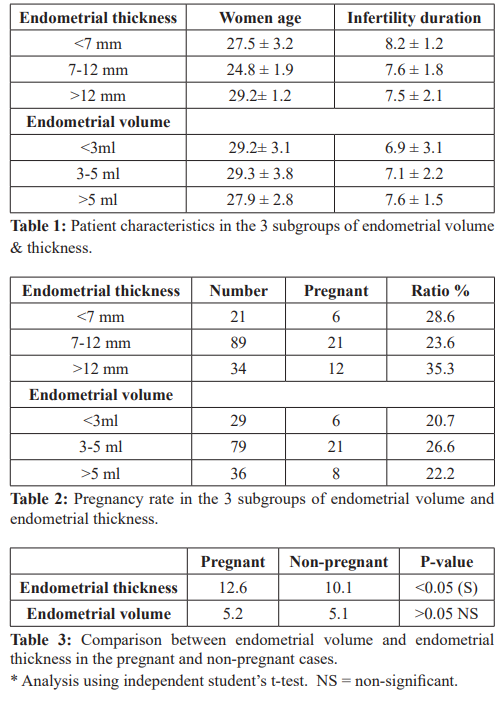
The mean age was 29.3 ± 3.4 (range 20-40), The mean duration of infertility was 7.3 ± 1.9 years. The number of embryos transferred was 2. The overall fertilization rate was 71.5%, clinical pregnancy rate; 31.8%. Patients were divided into three subgroups according to endometrial volume calculated; <3ml, 3-5ml, >5ml and according to endometrial thickness into three subgroups; <7mm, 7-12mm, >12mm. The mean age, period of infertility and number of embryos transferred in all subgroups is shown in table 1and there was no significant difference in these parameters Table 2 shows the number of pregnancies and pregnancy rates in each subgroup and differences were found to be non significant. Table 3 shows a non-significant difference in the mean endometrial volume but significant mean endometrial thickness in the pregnant as compared to the non-pregnant group.
Discussion
It is well known that the quality of embryos and the receptivity of the endometrium determine the success rate of IVF/ ICSI and successful implantation [11]. In the last few years, there has been a rising interest in evaluation of endometrial receptivity by methods of ultrasound technology. Many researchers tried to assess endometrial receptivity through many sonographic parameters, as endometrial thickness, but with low specificity [12]. Utilizing 2D transvaginal ultrasound to evaluate endometrial thickness does not comprise the total endometrial volume [2]. Other investigators stated a 12.6% as an error rate of for two dimensional volume measurements, whereas the error rate for three dimensional volume measurement was 6.4% only [13].
In addition the benefit of reproducibility of 3D endometrial volume measurement has been established by many researchers [8,9]. Many reports examined the volume of the endometrium on the days of downregulation, ovum retrieval and embryo transfer. In the current study there was no statistically significant difference in endometrial volume in women who conceived as compared to those who did not, but there was a significant difference in endometrial thickness between the two groups. This is in partial agreement with previous studies that reported no predictive value of measuring endometrial volume and thickness on IVF success [14,15]. When subdividing the women into three groups according to endometrial volume; <3ml, 3-5ml, >5 ml, also according to the thickness of the endometrium <7mm, 7- 12mm, >12mm, no statistically significant difference in pregnancy rates was found as regards to endometrial volume but there was a significant difference as regads to endometrial thickness which doesn't match with other investigators who subdivided the women similarly [16].
In the current study when analyzing endometrial volume & thickness assessment of women with grade I embryos, endometrial thickness was found to be better than endometrial volume in predicting pregnancy. Hence the validity of endometrial volume for canceling ET or cryopreserving embryos is questionable. Other authors reported that endometrial volume and thickness significantly higher in women who conceived as compared to those who did not conceive. However in agreement with our results, it was reported no significant reduction in pregnancy rates with endometrial volume < 2ml when compared to > 2ml [17]. In conclusion, 3D endometrial volume assessment is an easy, practical and reproducible method of endometrial evaluation in IVF programs. However endometrial volume is not a better predictor of IVF success when compared to endometrial thickness measured on day of hCG.
References
- Hull MG, Glazener CM, Kelly Population study of causes, treatment and outcome of infertility. Br Med J (Clin Res Ed). 1958; 291: 1693-1697.
- Friedler S, Schenker JG, Herman A, et al. The role of ultrasonography in the evaluation of endometrial receptivity following assisted reproductive treatments: a critical review. Hum Reprod Update. 1996; 2: 323-35.
- Pope CS, Cook EK, Arny M, et al. Influence of embryo transfer depth on in vitro fertilization and embryo transfer outcomes. Fertil Steril. 2004; 81: 51-8.
- Sundstrom P. Establishment of a successful pregnancy following in-vitro fertilization with an endometrial thickness of no more than 4 mm. Hum Reprod. 1998; 13: 1550-1552.
- Jurkovic D, Geipel A, Gruboeck K, et al. Three-dimensional ultrasound for the assessment of uterine anatomy and detection of congenital anomalies: a comparison with hysterosalpingography and two-dimensional sonography. Ultrasound Obstet Gynecol. 1995; 5: 233-237.
- Lev-Toaff AS, Pinheiro LW, Bega G, et Three-dimensional multiplanar sonohysterography: Comparison with conventional two-dimensional sonohysterography and X-ray hysterosalpingography. J Ultrasound Med. 2001; 20: 295-306.
- Alcazar JL, Galvan R. Three-dimensional power Doppler ultrasound scanning for the prediction of endometrial cancer in women with postmenopausal bleeding and thickened endometrium. Am J Obstet Gynecol. 2009; 200: 44-46.
- Lee A, Sator M, Kratochwil A, et al. Endometrial volume change during spontaneous menstrual cycles: Volumetry by transvaginal three-dimensional Fertil Steril. 1997; 68: 831-835.
- Yaman C, Ebner T, Sommergruber M, et Role of three- dimensional ultrasonographic measurement of endometrium volume as a predictor of pregnancy outcome in an IVF-ET program: a preliminary study. Fertil Steril. 2000; 74: 797-801.
- Mansour RT, Aboulghar MA, Serour GI, et al. Intracytoplasmic sperm injection using microsurgically retrieved epididymal and testicular sperm. Fertil Steril. 1996; 65: 566-572.
- Ozturk O, Bhattacharya S, Saridogan E, et al. Role of utero ovarian vascular impecance: predictor of ongoing pregnancy in an IVF-embryo transfer program. Reprod Biomed Online. 2004; 9: 299-305.
- Remohi J, Ardiles G, Garcia-Velasco JA, et al. Endometrial thickness and serum oestradiol concentrations as predictors of outcome in oocyte Hum Reprod. 1997; 12: 2271- 2276.
- Riccabona M, Nelson TR, Pretorius DH. Three-dimensional ultrasound: accuracy of distance and volume measurements. Ultrasound Obstet Gynecol. 1996; 7: 429-34.
- Schild RL, Indefrei D, Eschweiler S, et Three-dimensional endometrial volume calculation and pregnancy rate in an in- vitro ertilization programme. Hum Reprod. 1999; 14: 1255-1258.
- Schild RL, Knobloch C, Dorn C, et Endometrial receptivity in an in vitro fertilization program as assessed by spiral artery blood flow, endometrial thickness, endometrial volume, and uterine artery blood flow. Fertil Steril. 2001; 75: 361-366.
- Raga F, Bonilla-Musoles F, Casan EM, et al. Assessment of endometrial volume by three-dimensional ultrasound prior to embryo transfer: clues to endometrial receptivity. Hum Reprod. 1999;14: 2851-2854.
- Zollner U, Zollner KP, Specketer MT, et al. Endometrial volume as assessed by threedimensional ultrasound is a predictor of pregnancy outcome after in vitro fertilization and embryo transfer. Fertil Steril. 2003; 80: 1515-1517.