Endoscopic Radiofrequency Ablation of Fistula in Ano (E-RaFisTura) in the Era of Surgical Innovation. A Serial Prospective Evaluation of 10 Patients
Author'(s): Anastasios Xiarchos, Fernand Tshijanu*, and Athanasia Tsakpini
Department of Surgery, Athens Medical Center, Clinic of Peristeri, Greece.
*Correspondence:
Fernand Tshijanu, Department of Surgery, Athens Medical Center, Clinic of Peristeri, Greece, Tel: (30)6996154491.
Received: 18 October 2021 Accepted: 06 November 2021
Citation: Anastasios X, Fernand T, Athanasia T. Endoscopic Radiofrequency Ablation of Fistula in Ano (E-RaFisTura) in the Era of Surgical Innovation. A Serial Prospective Evaluation of 10 Patients. Gastroint Hepatol Dig Dis. 2021; 4(1): 1-3.
Abstract
Background: Fistula in-ano is an abnormal chronic infected tunnel (tract) between the rectum or the anal canal and perianal skin usually, with granulation tissue which connecting a primary orifice (internal) to a secondary one (external). This morbid antity represents a dilemma for both, patients and surgeon-proctologists because of postoperative issues occurrence such as fecal incontinence. The surgical management of this infectious condition has emerged nowadays, by emphasing new surgical techniques that preserve anal sphincter's integrity and functional. Over the last decade, numerous techniques sparing anal sphinters have gained popularity such as endoscopic approach (VAAFT), Laser, fibrin glue, transanal advancement flap repair [1,6]. In the same perspective,we are presenting in this paper, our preliminary outcomes of a combination of endoscopic approach (VAAFT) with Radifrequency Ablation of the fistula's tract that we nicknamed with the acronym of E-RaFisTura).
Methods: We enrolled 10 males patients with anal fistula, age groupe 50-70 years, without any comorbidity in the term of diabetes mellitus, bowel inflammatory disease. Preoperatively each of them underwent a digital rectal examination, pelvic MRI, colonoscopy to rule out any concomitant abscess, Crohn's disease. Fleet enema, subcutaneus lower molecular weight heparin as well as intravenous broad spectrum antibiotic were administered an hour prior the surgical procedure. All patients were shifted to endoscopic surgical treatment of anal fistula (VAAFT) by using the fistuloscope of Piercarlo Meinero combined to the device of Fistura (Radiofrequency Ablation) with its probe 6-7 F (Figure 1 a,b,c).
Then we visualized the fistula's tract and we seal it with radiofrequency thermocoagulation without damaging the anal sphincters by closing the internal opening with a suture node (Vicryl Rapid 3-0). Taxinomically, 2 patients had intersphincteric fistula, 3 transphincteric and the 5 others had submucosal anal fistula.
Outcomes: We are inthe third month of follow up, none of the aboved mentioned patients has presented any postoperative issue excepting some local discomfort in immediate postoperative day, relieved with voltaren. Furthermore, the orificial wound healing is successful.
Conclusion: Focused on our preliminary results, despite the small volume of patients, this combination of endoscopic and radiofrequency ablation can be regarded with optimism in selected patients. We will perform a powerful prospective study with a huge sample to have more accurate opinion.
Bioethics Considerations: All enrolled patients had given their written consent prior. Furthermore,this surgical trial was approved by the Ethical commitee of Our Clinic.
Keywords
Description
Under general anesthesia, Patient in lithotomy position, administration of intraveneous antibiotic 10 minutes prior, meticulous inspection of the field. We used the fustuloscope of Meinero manufactued by Karl storz GmbH in Germany (Figure 1a), the endobrush, fistula probe, forceps, anoscope, probe 6-7 F of fistura's device (RFA) (Figure 1b) instead of unipolar electrode. The procedure was performed in two stades,diagnostic and operative.
The explorative or diagnostic phase started with the insertion of the fistuloscope through the external opening with a concomitant infusion of normal saline fluid to allow the opening of tract and clear the view. In some patients, we removed the scar tissue around the external opening. Then a single-wing proctoscope was inserted in the anus to find out the internal opening via the observation of the fistuloscope's light.
The operative Phase's aim was the complete debridement of the principal fistula tract as well as the closure of the internal opening with three absorbable 3-0 sutures followed by the application of 1cc of bioglue in spray form [2,4-6]. The debriment was first fulfilled with the endobrush then, by the radiofrequency thermocoagulation to ablate with the Fistura probe inserted by avoiding damaging adjacent structures (anal sphincter). This probe's insertion is done by withdrowing gradually the catheter 5 mm each 12 seconds relatively to the generated beeps sound. The energy used was in avarage 3000-5000 joules regulated with the foot pedale by the Surgeon. Then cleaning the ablated tract with normal peroxid of peroxyde solution and betadine solution.
Discussion
Anal Fistula is a chronic infected small tunnel between the anal or rectal canal and the the skin near the anus. Despite numerous tries over the last decades to improve surgical approach of anal fistula, it persistes to be a dilemma for patients as well as for surgeon-proctologist. Long-established surgical pespective like fistulotomy, lay-open procedure are succesful for simple and most distal fistulas in the rate of 95-100%. Nevertheless, when this above mentioned techniques are used for complex type of anal fistula, they are associated with inflated rate of postoperative issues in the terms of fecal incontinence, recurrence, depression related to incontinence. Draining seton decreases damaging anal sphincter however, it is associated with increased recurrence rate of fistula. Regarding cutting setons, they were the first surgical approach for complex anal fistula, it was stated that this technique could preserve the sphincter function. However, countless evidencies proved that the cutting setons are associated with fecal incontinence in the rate of 20,5% to 67%. Fibrin glue injection is a simple approach to treating complex anal fistula with minimal side effect,woefully its long-term sucess rate is only approximately 14%. To date, fibrin glue injection is generally used in combination with other surgical approaches [2,3]. Fistula plug is also a simple therapeutic approach with the reported healing rates ranging from 38,0 to 72,7%, although it has not been widely used because of the high cost [10,11]. TAFR is a sphincter-saving technique for complex anal fistula,but the recurrence rates are in the range of 7 to 49%. LIFT is another widely recognized sphincter-saving technique with a success rate of approximately 81,4%. This later is regarded by some authors as a procedure with challenge since it may jeopardize the blood supply of the anal sphincter and rectal mucosa [12,14]. In 2011, Wilhelm described a sphincter-preserving technique for anal fistula repair using a noval radical emitting laser probe,with healing rate of 81,8 % after a median follow-up of 7,4 months. The drawback of this technique is the difficulty associated with identifying the fistula's features such as the internal opening, the secondary tracts as well as abscess cavities [15,17-19].
Most of the current treatments for complex anal fistula are based on three main principles: identification of the fistula's tracts as well as the internal opening, complete destruction of the tracts, and preservation of anal sphincter function. However, some studies have shown that the key of fistula's healing lies in the sealed closure of the internal opening coupled with adequate drainage of fistula tract [13,16,18]. VAAFT is designed based only on these two key points: it provides real-time visualization of the anatomy so that surgeons can properly handle the internal opening and perform sufficient drainage of the debrided tract [7-9,14]. In the same perspective,we treated our 10 patients with anal fistula, by combining VAAFT to Fistura (a procedure using radiofrequency thermociagulation to treat anal fistula) similar to the principle of microwave. This minimally invasive technique seals the fistula tract without damaging the anal sphinter. Fistura induces ablation in 4 phsaes: Ionic agitation, Vaporization-dehydration of the tissue, thermal destruction, dehydration of the tissue and coagulation (Figure 1 a,b,c). We nick named this combination of video-assisted of anal fistula treatment with Fistura is nicnamed by our Department, E-RaFistura.
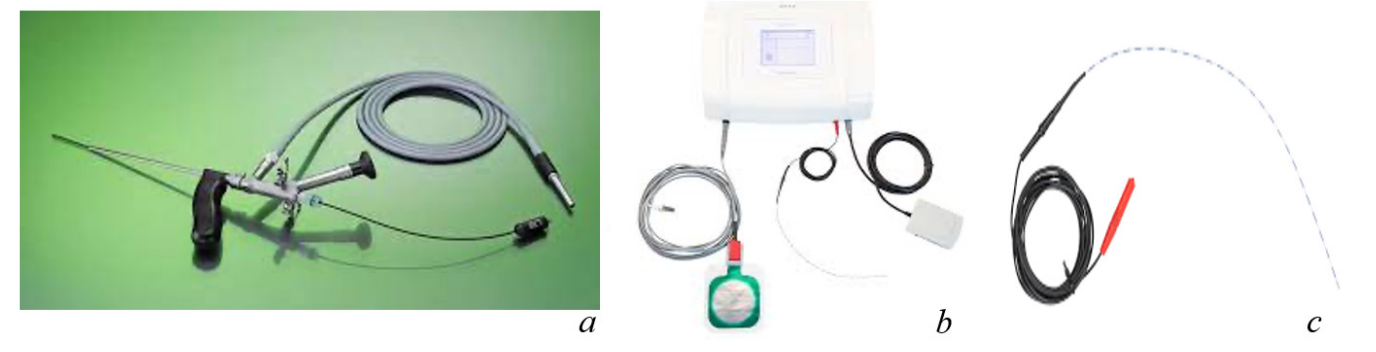
Figure 1 abc: a: Fistuloscope, b: Fistura's device, c: Probe of RFA.
Conclusion
According to our preliminary resultes of 3 months-follow-up, we expect that this new combination gives optimism in improving postoperative outcomes in the terms of reduction of reccurrence rate, as well as of fecal incontinence occurrence. Thus we encourage other center to use it on a big size sample with a long follow-up periode.
References
- Limura E, Giordano P. Modern management of anal fistula. World J Gastroenterol. 2015; 21: 12-20.
- Buchanan GN, Bartram CI, Phillips RK, et al. Efficacy of fibrin sealant in the management of complex anal Dis Colon Rectum. 2003; 46: 1167-1174.
- Alasari S, Kim NK. Overview of anal fistula and systematic review of ligation of the intersphincteric fistula tract (LIFT) Tech Coloproctol. 2014; 18: 13-22.
- Meinero P, Mori L. Video-assisted anal fistula treatment (VAAFT): A novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol. 2011; 15: 417–22.
- Walega P, Romaniszyn M, Nowak W. VAAFT: A new minimally invasive method in the diagnostics and treatment of anal fistulas – initial results. Pol Przegl Chir. 2014; 86: 7-10.
- Meinero P, Mori L, Gasloli G. Video-assisted anal fistula treatment: A new concept of treating anal fistulas. Dis Colon Rectum. 2014; 57: 354-359.
- Kochhar G, Saha S, Andley M, et Video-assisted anal fistula treatment. JSLS. 2014; 18: e2014.00127.
- Chowbey PK, Khullar R, Sharma A, et Minimally invasive anal fistula treatment (MAFT)-an appraisal of early results in 416 patients. Indian J Surg. 2015; 77: 716-721.
- Mendes CR, Ferreira LS, Sapucaia RA, et al. Video- assisted anal fistula treatment: Technical considerations and preliminary results of the first Brazilian Arq Bras Cir Dig. 2014; 27: 77-81.
- Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg. 1976; 63: 1-12.
- Ratto C, Litta F, Parello A, et Gore Bio-A(R) Fistula Plug: A new sphincter-sparing procedure for complex anal fistula. Colorectal Dis. 2012; 14: e264-269.
- Cintron JR, Abcarian H, Chaudhry V, et al. Treatment of fistula-in-ano using a porcine small intestinal submucosa anal fistula plug. Tech Coloproctol. 2013; 17: 187-191.
- Wilhelm A. A new technique for sphincter-preserving anal fistula repair using a novel radial emitting laser probe. Tech Coloproctol. 2011; 15: 445-449.
- Seow-En I, Seow-Choen F, Koh PK. An experience with video-assisted anal fistula treatment (VAAFT) with new insights into the treatment of anal fistulae. Tech Coloproctol. 2016; 20: 389-393.
- Schwandner Video-assisted anal fistula treatment (VAAFT) combined with advancement flap repair in Crohn’s disease. Tech Coloproctol. 2013; 17: 221-225.
- Chivate SD. Comment on Meinero and Mori: Video-assisted anal fistula treatment (VAAFT): A novel sphincter-saving procedure to repair complex anal fistulas. Tech Coloproctol. 2012; 16: 465-66.
- Prosst RL, Ehni W. The OTSC® Proctology clip system for anorectal fistula closure: The ‘anal fistula claw: Case report. Minim Invasive Ther Allied Technol. 2012; 21: 307–12.
- Gustafsson UM, Graf Excision of anal fistula with closure of the internal opening: functional and manometric results. Dis Colon Rectum. 2002; 45: 1672–1678.
- Tyler KM, Aarons CB, Sentovich SM. Dis Colon Rectum. Plant Radiofrequency treatment of tonsillar hypertrophy. Laryngoscope. 2002; 112: 2-20.