Epidemiological and Clinical Profile of Irritable Bowel Syndrome among Medical Students in Conakry
Author'(s): Diallo Mamadou Sarifou1,2*, Youssouf Oumarou3, Kanté Boubacar2, Diallo Abdourahmane N'Djouria4, Diallo Kadiatou1,2, Wann Thierno Amadou2,5, Diallo Djenabou1,2, Bah Mamadou LamineYaya2,5, Diakhaby Mamadou5, Kanté Mamadou Aliou5, Sylla Djibril2,5 and Soro Dramane6
1Hepato-gastroenterology Department of the Donka National Hospital CHU Conakry, Guinea.
2Faculty of Health Sciences and Techniques, Gamal Abdel Nasser University, Conakry, Guinea.
3Bangui Community University Hospital Center, Internal Medicine Department, Bangui, Central African Republic.
4SOS Hepatitis Guinea.
5Internal Medicine Department of the Donka National Hospital CHU Conakry, Guinea.
6Hepato-Gastroenterology Department of the Cocody University Hospital Center, Abidjan, Ivory Coast.
*Correspondence:
Dr. Mamadou Sarifou DIALLO, Hepato-gastroenterology Department Donka National Hospital CHU Conakry, Guinea, Tel: 00224628690551.
Received: 05 Mar 2024 Accepted: 11 Apr 2024 Published: 19 Apr 2024
Citation: Diallo M Sarifou, Youssouf Oumarou, Kanté Boubacar, et al. Epidemiological and Clinical Profile of Irritable Bowel Syndrome among Medical Students in Conakry. Gastroint Hepatol Dig Dis. 2024; 7(2): 1-5.
Abstract
Introduction: Irritable bowel syndrome (IBS) represents a real public health problem. It is a gastrointestinal disorder characterized by chronic abdominal pain and intestinal transit abnormalities, in the absence of identifiable organic substrate. It is a clinical entity whose prevalence, impact on the quality of life of individuals and the health costs generated are significant. The aim of this study was to determine the prevalence of irritable bowel syndrome, clinical aspects, triggering and/or aggravating and calming factors in medical students.
Methods: This was a descriptive cross-sectional study. It was carried out from June 8, 2023 to December 8, 2023, i.e. a period of six (06) months. The study took place in the faculties of medicine of the Gamal Abdel Nasser University of Conakry and the University of La Source and meeting the criteria of Rome IV.
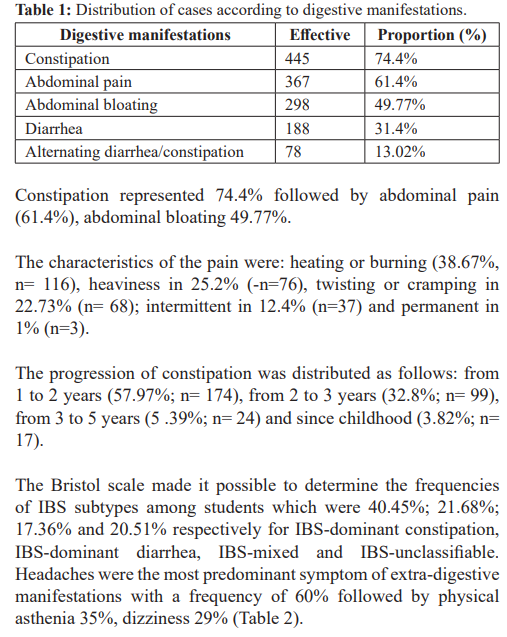
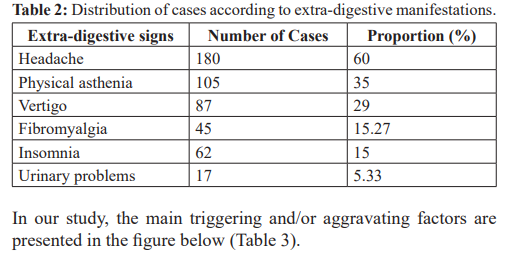
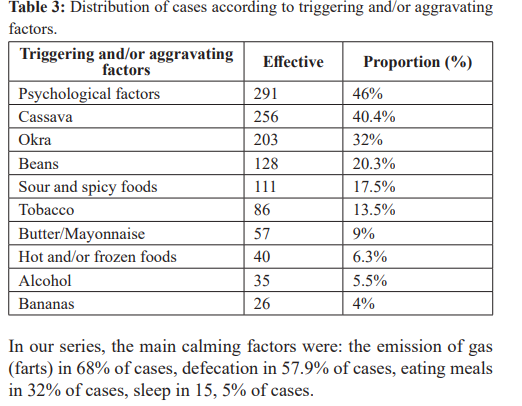
Results: Three hundred cases of IBS out of 633 surveyed, representing a prevalence of 47.4%, were recorded. There was a male predominance with a M/F sex ratio of 2.13. The average age was 22.51 years with extremes of 18 and 35 years. The main clinical signs were constipation in 74.4%, abdominal pain (61.4%), abdominal bloating 49.77%, diarrhea 31.4% and alternating diarrhea/constipation 13.02%. The most frequent extradigestive manifestations were: headaches 60%, physical asthenia 35% and dizziness 29%. The main triggering factors were: psychological factors 46% and dietary factors (cassava 40.4%, okra 32%, beans 20.3%). The calming factors were: the emission of gas (farts) in 68% of cases, defecation in 57.9% of cases, eating meals in 32% of cases, sleep in 15.5% of cases.
Conclusion: IBS is a public health problem that impairs the quality of life of those affected. Abdominal pain, constipation and abdominal bloating constitute the symptomatic triad. Stress is a triggering factor for the symptoms.
Keywords
Introduction
Irritable bowel syndrome (IBS), which is a very common and often debilitating chronic illness, is part of the new name “disorders of interactions of the brain-intestine axis” formerly called “functional intestinal disorders” (TFI)) [1].
IBS is manifested by the chronic occurrence of digestive symptoms such as abdominal pain, bloating, constipation or diarrhea or an alternation of the two, without the intestine showing a visible lesion [2]. The Rome IV criteria, established by consensus of a multinational group of experts in the field of gut-brain interaction disorders, can be used to diagnose IBS and for research purposes [3].
Although its etiology is still unknown, several physical and psychological factors have been cited to contribute to its pathogenesis such as stress, anxiety and abnormal attitudes towards the disease, which worsen the conditions of patients [4,5]. Irritable bowel syndrome (IBS) represents a real public health problem. Prevalence estimates vary considerably internationally [6]. It represents the first reason for consultation in gastroenterology (24 to 45%) and 5 to 10% of consultations with general practitioners and is a daily concern for the doctor due to the constant complaints of these patients [7].
IBS symptoms can significantly affect patients' quality of life, and studies have shown that patients would be willing to give up 10 to 15 years of life expectancy for an immediate cure or accept a risk of death of 1% with a medication that could cure their symptoms [8]. IBS represents a significant burden on healthcare systems worldwide. Direct medical costs attributed to IBS in the United States, excluding prescription and over-the-counter medications, are estimated at $1.5 to $10 billion per year [9]. High levels of health resource utilization, testing that is often unnecessary or performed too frequently, and significant regional variation in testing and treatment further contribute to significant direct and indirect costs [10]. Medical students are often more stressed than other population groups due to the restrictive academic environment.
Through this study, we wanted todetermine the prevalence of irritable bowel syndrome, clinical aspects, triggering and/ or aggravating and calming factors among medical students in Conakry.
Material and Methods
We conducted a cross-sectional, descriptive study. It was carried out from June 8, 2023 to December 8, 2023, i.e. a period of six (06) months. The study took place in the medical faculties of the Gamal Abdel Nasser University of Conakry (UGANC) and the Université la Source (US). We targeted all students regularly enrolled in the two medical faculties during the study period and present at the time of the survey.
Included in our study were all students of all ages, genders and origins from the Faculty of Medicine of the Gamal Abdel Nasser University of Conakry and La Source University presenting with irritable bowel syndrome without treatment having agreed to participate in this study and meeting the Rome IV criteria.
Not included in this study were those who did not wish to answer the questionnaires, those who were absent during the survey, those with an organic intestinal pathology (colorectal cancer, chronic inflammatory bowel disease of any type of disease). Crohn's disease or ulcerative colitis, a celiac disease) in progress which can give symptoms similar to those of irritable bowel syndrome and those with a gynecological pathology which can mimic intestinal symptoms.
Rome IV criteria
Recurrent abdominal pain occurring on average, at least one day per week in the last three months with at least two of the following criteria:
- Associated with defecation;
- Associated with a change in stool frequency;
- Associated with a change in stool consistency (shape or appearance)
Criteria met within the last three (3) months with onset of symptoms at least six (6) months before diagnosis.
Data collection was done using an individual survey form established for this purpose.
Sampling: the questionnaire was distributed to all those who were present and who had given informed consent for participation in the study.
The variables studied were: age, sex, symptoms (abdominal pain, diarrhea, constipation, alternating diarrhea/constipation, abdominal bloating, belching), extra-digestive manifestations (headache, insomnia, anxiety, fibromyalgia, dyspareunia, urinary disorders), triggering and/or aggravating factors (psychological factors: stress, anxiety, dietary factors) and calming factors (sleep, defecation, meals, belching, farts).
We carried out an interview, the respondents voluntarily completed the pre-established form; clarifications were provided according to the questions asked to the respondents.
The data analysis was carried out on the Epi info 6.0.4 French version software, the analysis on the SPSS 12.0 software. The comparison was made using the Chi square test. The significance threshold at 5%.
In this study we respected ethical considerations in particular; the moral and physical integrity of the person, the free and voluntary consent of the person, the confidentiality of the results and the anonymity of the people interviewed and the possible desire to withdraw from the person investigated without prejudice.
Results
During the study period, 300 cases of IBS out of a total of 633 students questioned, representing a prevalence of 47.4%, were recorded.
The average age was 22.51 years with extremes varying from 18 to 35 years. The age group of 21-29 years was the most affected with a frequency of 94.0% (n=282) followed by those less than or equal to 20 years (5.80%, n= 17) and those ≥ 30 years (0.2%; n=1). Males represented 68.1% compared to 31.9% females, the M/F sex ratio is 2.1
Discussion
The limitations of this study were: the absence of certain students, there was a risk that some of the respondents' responses would be erroneous.
In our series the prevalence of IBS among medical students in Conakry was 47.4%. This high prevalence could be explained by the fact that medical students are in a period of permanent stress. Our results are clearly superior to those found by Sehonou et al. in Benin [11] and Fallah et al. In Pakistan [12] who reported respective prevalences of 14% and 28.3% among medical students. However, they remain close to those observed by Ibrahim et al. [13] in Saudi Arabia among medical students at Prince Abdelaziz University in Saudi Arabia which was around 31.8%.
This difference could be explained by the use of diagnostic criteria and sampling techniques which vary from one study to another. The average age of our participants was 22.51 years with extremes varying from 18 to 35 years. The age group of 21-29 years was the most affected with a frequency of 94.0% (n=282) followed by those less than or equal to 20 years in 5.80% of cases (n=17). This result is superimposable to the data of Sehonou et al. in Benin [11] and Fallah et al. in Pakistan [12] who noted respective average ages of 21.6 years and 22 years. The predominance of these age groups could be explained by the fact that they correspond to the usual age of students at university. The distribution of our cases according to sex showed a male predominance of 68.1% compared to 31.9% females, the M/F sex ratio is 2.13 in favor of men. Our results are identical to those reported by Okeke et al. [14] and Husain et al. [12] who found a higher prevalence of IBS in men than in women in their studies. Our results are different from those reported by Sehonou et al. Sehonou et al. in Benin [11] who noted a female predominance. This male predominance in our series could be explained by the fact that in Guinea the schooling rate of boys is higher than that of girls on the one hand and certain socio-cultural practices in particular early marriage of girls, The origin of the abandonment of studies by many girls and also family occupations which ensure that they are unable to pursue higher education on the other hand.
From a clinical point of view, the most frequently encountered signs were constipation 74.4% followed by abdominal pain (61.4%), abdominal bloating 49.77%, diarrhea 31.4% and alternating diarrhea/constipation in 13.02% of cases (Table 1).
Abdominal pain was noted in Cameroon by Tzeuton et al. [15], in 83% of cases followed by constipation 68%; gas emission 56% and bloating 49%. Likewise in Guinea, Sarifou DM et al. [16] found the main clinical signs to be: abdominal pain (92.21%), constipation (84.17%), heartburn (31.65%), abdominal bloating. (28.64%), diarrhea (11.55%) and alternating diarrhea/constipation (0.87%)
On the other hand, Frexinos et al. [7] reported in France a predominance of gas emission (59%), followed by abdominal pain (48%); feeling of poor digestion (40%); constipation (35%); diarrhea (28%); bad breath (22%) and incomplete evacuation of stools (19%). The duration of constipation was very variable and was distributed as follows: from 1 to 2 years (57.97%; n= 174), from 2 to 3 years (32.8%; n= 99), from 3 to 5 years (5.39%; n= 24) and since childhood (3.82%; n= 17). This long history of constipation could be explained by the chronicity of these disorders, the lack of knowledge of the triggering and/or aggravating factors and the insufficiency of treatment.
Warming or burning was the type of abdominal pain most frequently encountered in our series (38.67%, n=116), heaviness in 25.2% of cases (n=76), twisting or cramping in 22.73% of cases (n= 68); intermittent in 12.4% of cases (n=37) and permanent in 1% of cases (n=3).
Our results are different from those reported by Siproudhis et al.[17] in 2002 in France who found a predominance of the sensation of heaviness and heaviness (53.7%), followed by cramps (31.5%) and burning (24.1%). Headaches dominate the extra-digestive manifestations at 60% followed by physical asthenia 35%, dizziness 29%, fibromyalgia 15.27%, insomnia 15% and urinary disorders 5.33%. The multiplicity of these extra signs digestive causes colopaths to consult several services through traditional therapists and witch doctors without success [16]. These results are identical to those reported by Sarifou DM et al. [16] who noted in their study as extra digestive comorbidities of the insomnia 50.25%, headaches in 30.40%, chronic fatigue in 22.36%, fibromyalgia in 22.86% of cases, anxiety in 32.16% and urinary disorders in 10 80% of cases. Likewise in a French study, Ducrotté et al. [2] also reported extra-digestive comorbidities of IBS with respective frequencies of 50.75% for fibromyalgia, 30.56% for dysuria, 30.50% for chronic fatigue and 30.50% for headaches.
The distribution of our cases according to the triggering factors shows a predominance of psychological factors at 46%, followed by dietary factors (cassava 40.4%, okra 32%, beans 20.3%, acidic and spicy foods 17.5%; Table 3). Patients often notice themselves a temporal connection or exacerbation of symptoms related to diet. The predominance of psychological factors among students could be explained by the multiplicity of sources of stress: long course schedules, overwork, the desire to succeed at all costs, lack of money and especially the loss of a loved one who financed the studies. This predominance of psychological factors was noted by Coffin B; [18] in France which had 53.4%, stress and 47.5% meals as the cause of IBS. Similarly, Spiroudhis et al. [17] reported a predominance of psychological factors in 67% of cases. The often distressing chronicity of TFI and anxiety could explain this predominance of psychological factors by sometimes making these patients cancerophobic; some patients speak of bewitchment in the African context. It appears from this study that nutritional factors play an undeniable role in the manifestations of IBS [16].
IBS and psychological disorders are frequently associated. A study by Khoshkrood et al. [19] in 2009 in Iran showed that 55.8% of the causes of TFI were associated with stress. Furthermore, in Saudi Arabia, Ibrahim et al. [13] had reported that 40.10% of students with IBS were anxious and 41.9% had morbid depression. Emission of gas (farts) in 68% of cases, defecation in 57.9% of cases, eating meals in 32% of cases, sleeping in 15.5% of cases relieved the pain of our respondents. These calming factors conform to the definition of irritable bowel syndrome according to the Rome IV criteria.
Conclusion
Irritable bowel syndrome constitutes a public health problem that impairs the quality of life of subjects. Irritable bowel syndrome is relatively common in the working population. It is common among medical students in Conakry. Psychological and dietary factors were the triggering factors for IBS and the course was often chronic. Abdominal pain, transit disorder and abdominal bloating constituted the symptomatic triad. Emission of gas and defecation relieved the pain of our respondents. Irritable bowel syndrome has a high prevalence in our survey area and presents many similar characteristics to those in other countries.
References
- Drossman DA, Hasler Rome IV-Functional GI Disorders of Gut-Brain Interaction. Gastroenterology. 2016; 150: 1257- 1261.
- Ducroté P, Dapoigny M, Bonaz B, et Symtomatic efficacy of beidellitic montmorillonitis in irritable bowel syndrome: A randomized, controlled trial. Food Pharmacol Ther. 2005; 21: 435-444.
- Mearin F, Lacy BE, Chang L, et al. Bowel Disorders. Gastroenterology. 2016; 150: 1393-1407.
- Han SH, Lee OY, Bae SC, et Prevalence of irritable bowel syndrome in Korea: population-based survey using the Rome II criteria. J Gastroenterol hepatol. 2006; 21: 1687-1692.
- Camilleri M. Peripheral mechanisms in irritable bowel syndrome. SO N Engl J Med. 2012; 367: 1626-1635.
- Lovell RM, Ford Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroentreol Hepatol. 2012; 10: 712-721.
- Frexinos J, Delvaux M, Lagier E. Irritable bowel syndrome. The Practitioner’s Review. 1998; 48: 2257-2260.
- Drossman DA, Morris CB, Schneck S, et al. International Survey of patients with IBS: symptom characteristics and their severity, health status, treatments, and risk taking to achieve clinical benefit. J Clin Gastroenterol. 2009; 43: 541-550.
- Canavan C, West J, Card T. Review article: the economic impact of the irritable bowel Food Pharmacol Ther. 2014; 40: 1023-1034.
- Tuppin P, Rivière S, deutsch D, et al. Burden of drug use for gastrointestinal disorders in France: a national study using reimbursement data for 57 million inhabitants. Therap Adv Gastroenterol. 2019; 12: 17562848-19853790.
- Sehonou J, Dodo Clinical profile and factors associated with irritable bowel syndrome among medical students in Cotonou, Benin. Pan Afr. Med. J. 2018: 31: 123.
- Naeem SS, siddiqui UE, Kazi AN, et al. Prevalence and factors associated with irritable bowel syndrome among medical students of Karachi, Pakistan: across sectional BMC Remarks Res. 2012; 50: 255.
- Ibrahim NKR, Battarjee WF, Almehmadi SA. Prevalence and predictors of irritable bowel syndrome among medical students and interns in King abdul Aziz University, Jeddah. Libyan J Med. 2013; 8: 21287.
- Husain N, Chaudhry IB, Jafri F, et A population-based study of irritable bowel syndrome in a non-Western population. Neurogastroenterol Motil. 2008; 20: 1022-1029.
- Tzeuton C. Functional digestive disorders in the African context. Actaendoscopy. 2000; 30: 579- 585.
- Sarifou DM, N’Djouria DA, Tidiane DA, et Epidemiological Profile of Persistent Functional Disorders at the Conakry University Hospital. European Scientific Journal, ESJ. 2024; 20: 243-255.
- Siproudhis L, Michel Delvaux, Stanislas Chaussade, et al. Doctor-patient relationship in irritable bowel syndrome. Gastroenterol Clin Biol. 2002; 26: 1125-1133.
- Coffin B. Visceral sensitivity and functional digestive disorders. Clinical significance and therapeutic perspectives. Clinical and biological gastroenterology. 2009; 33: S9-S16.
- Khoshkrood-Manssoori B, Pourhoseingholi MA, Safaee A, et al. Irritable bowel syndrome: A population-based study. J Gastrointest Liver Dis. 2009; 18: 413-418.