Evolutionary Profile of Chronic Inflammatory Bowel Disease at Brazzaville University Hospital in 2023: A Case Series of 26 Patients
Author'(s): Ngami RS1,2*, Mikolélé Ahoui Apendi PC1,2, Mimiesse Monamou JF1,2, Mongo-Onkouo A1,3, ItouaNgaporo NA1,2, Motoula Latou PM1,2, Ngalessami Mouakosso M1, Adoua Céline Sandra1, Ibobi Mauria Gilga1, Deby Gassaye1,2 and Atipo Ibara BI1,2
1Gastroenterology and Internal Medicine Department, Brazzaville University Hospital, Republic of Congo.
2Faculty of Health Sciences, Marien Ngouabi University, Republic of Congo.
*Correspondence:
Ngami RS, Gastroenterology and Internal Medicine Department, Brazzaville University Hospital, Republic of Congo.
Received: 10 Feb 2024 Accepted: 15 Mar 2024 Published: 22 Mar 2024
Citation: Ngami RS, Mikolélé Ahoui Apendi PC, Mimiesse Monamou JF, et al. Evolutionary Profile of Chronic Inflammatory Bowel Disease at Brazzaville University Hospital in 2023: A Case Series of 26 Patients. Gastroint Hepatol Dig Dis. 2024; 7(1): 1-4.
Abstract
Chronic inflammatory bowel disease (IBD) is rarely described in sub-Saharan Africa. The aim of this study was to evaluate the evolutionary profile of a series of 26 cases of IBD at the Brazzaville university hospital in 2023.
Patients and Methods: This was a cross-sectional analytical study conducted in the Gastroenterology department of Brazzaville university hospital over a 13-year period. IBD was diagnosed on the basis of clinical (chronic diarrhoea, rectal discharge), morphological (intestinal parietal thickening), endoscopic (acute or chronic lesions) and histological criteria. Severe forms were defined by the fact of having a pancolitis and ano-perineal lesions. The Wilcoxon test was used to compare variables at a threshold of 0.05.
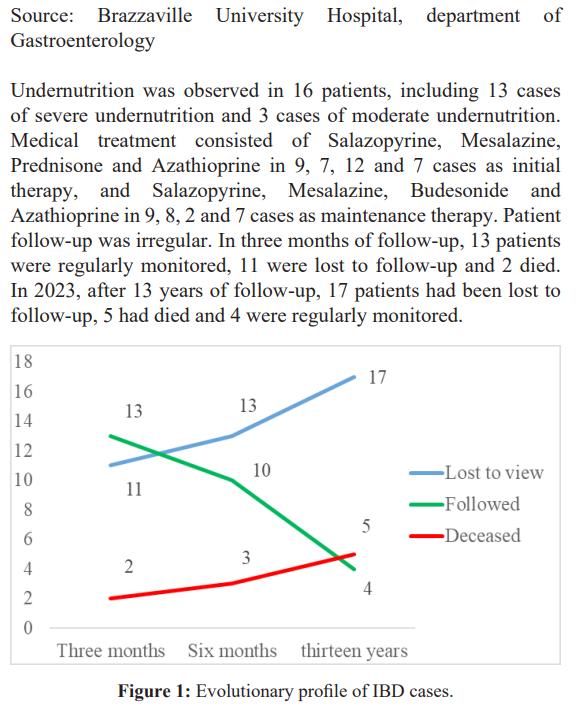
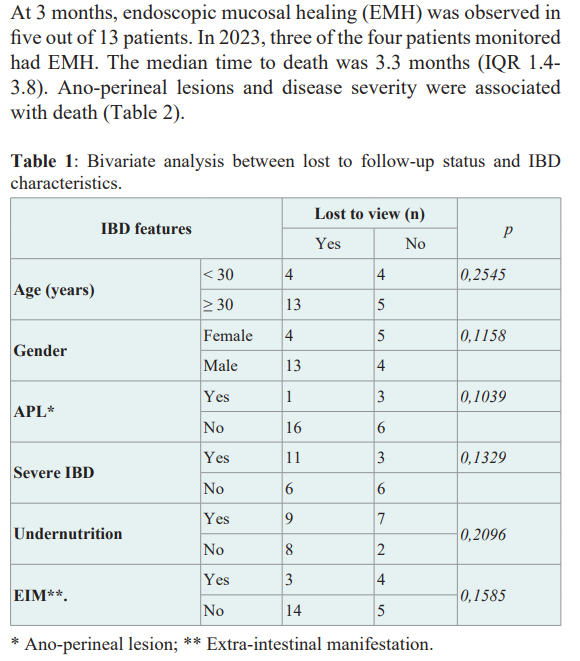
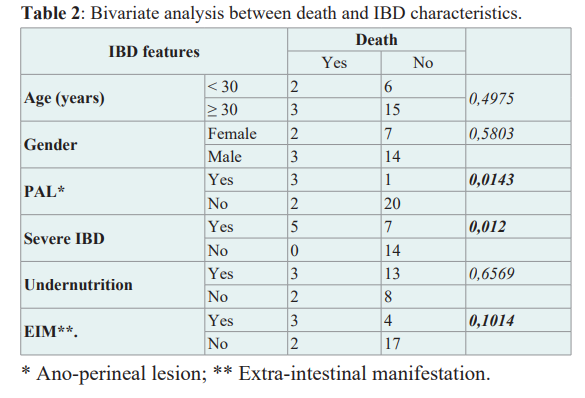
Results: A total of 26 patients were included, representing 0.2% of hospitalizations. The sex ratio was 1.9. The median age was 37 (IQR 24-51), and nine patients were under 30. IBD included Crohn's disease (CD), ulcerative colitis (UC) and indeterminate forms in 10, 8 and 8 cases respectively. The median duration of symptoms before diagnosis was 2.2 years (IQR 0.1-6). Twelve patients had a severe form, including two cases of severe acute colitis. Undernutrition was observed in 16 patients, including 13 cases of severe undernutrition. By 2023, 17 out of 26 patients had been lost to follow-up, 5 had died and 4 were regularly monitored. The median time to death was 3.3 months (IQR 1.4-3.8). The presence of ano-perineal lesions (p=0.0143) and disease severity (p=0.019) were factors associated with death.
Conclusion: Keeping IBD patients in the care circuit is a multidisciplinary challenge to reduce the proportion of patients lost to follow-up, and improving their management.
Keywords
Introduction
Chronic inflammatory bowel diseases are complex nosological entities of unknown cause, most often evolving in intermittent flare-ups [1]. They are more prevalent in northern European and American countries, with a north-south gradient. [2]. In sub- Saharan Africa, the prevalence of IBD is low, and the disease is little known, particularly among the general population. The lack of diagnostic resources and trained personnel partly explain the problems of IBD management in Africa. In Congo, an initial study carried out in 2015 described the epidemiological, diagnostic and therapeutic parameters of 9 cases over 13 years [3]. However, little is known about patient outcomes. The aim of this study was to assess the evolutionary profile of chronic inflammatory bowel disease at Brazzaville University Hospital in 2023.
Patients and Methods
We carried out a cross-sectional analytical study from September 2010 to October 2023, a period of 13 years, in the Gastroenterology and Internal Medicine Department of the Centre Hospitalier Universitaire (CHU) de Brazzaville. The study population consisted of patients hospitalized or followed-up for IBD, diagnosed on the basis of a combination of epidemiological (age, lifestyle, non-steroidal anti-inflammatory drugs), clinical (diarrhea, bloody emissions, abdominal pain, anemia, undernutrition), morphological (abdominal ultrasound and CT scan), endoscopic (gastroscopy, rectoscopy or ileocoloscopy) and histological (diffuse lymphoplasmacytic infiltrate of the chorion, polynuclear infiltrate and loss of mucosecretion in UC, epitheliogigantocellular granuloma without central necrosis in CD. We included all patients aged 18 and over, diagnosed with IBD and followed up in the department during the study period. Files suggesting IBD but containing no endoscopic examination were excluded. Progression profile included endoscopic mucosal healing, follow-up status, mean follow-up time, death, mean time to death and risk factors for death. Data were collected on a paper questionnaire, entered into Microsoft Excel 19 and analyzed using Epi info 7.2. The Fisher's exact test and the Wilcoxon test were used from a threshold of 0.05.
Results
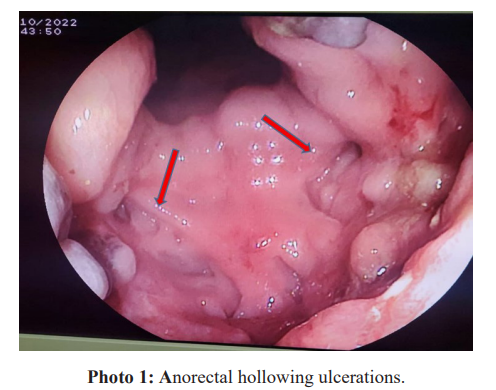
Over a 13-year period, we selected 26 cases of patients hospitalized and followed in the department for chronic inflammatory bowel disease (IBD) out of a total of 12,064 hospitalizations, representing a prevalence of 0.2%. There were 17 men and 9 women, giving a sex ratio of 1.9. The median age was 37 (IQR 24-51), and 9/26 patients were under 30. The IBD diagnosis was Crohn's disease (CD), ulcerative colitis (UC) and indeterminate forms in 10, 8 and 8 cases respectively. One case of co-morbidity of UC and human immunodeficiency virus infection was noted. In this case, histology was essential in the diagnosis of UC. The median duration of symptoms before diagnosis was 2.2 years (IQR 0.1-6). Twelve cases of severe colitis were diagnosed with deep anorectal ulcerations (photo 1), including two cases of severe acute colitis with profuse hematochezia.
Discussion
The prevalence of IBD in sub-Saharan Africa is difficult to assess. In Mali, 59 cases were reported in 3 years, representing 0.27 of hospitalizations and 6.1% of digestive pathologies, which was comparable to our study [4]. However, these authors included children in their study. Medhioub and colleagues noted an increase in the prevalence of IBD in patients over 60, but there was no difference in terms of clinical forms and surgery compared with younger patients [5]. Hassine and colleagues in Morocco and Siala et al. in Tunisia found that 13% and 14% respectively of people over 60 had IBD [6,7]. The average age was 48.2 ±18.4 years, with extremes of 10 and 89 years, and a female predominance in Mali. The epidemiology of IBD is different in children, with a predominance of CD (65%) compared with UC (35%); a male predominance in CD and a female predominance in UC [8].
In 2015, nine cases of CD were reported in Congo, compared with ten cases in 2023 [3]. The hospital prevalence of CD does not appear to be increasing in our country. Bougouma and colleagues in Burkina Faso reported 20 cases of ulcerative rectocolitis, while Diouf and colleagues in Senegal reported 32 cases of UC out of 2667 recto-sigmoidoscopies and colonoscopies, i.e. 1.2% of low digestive endoscopic examinations. Moderate forms were mainly observed in the elderly, i.e. 82.3% of the population [7]. Half of our patients had moderate forms but were young.
Medication for IBD has been on the rise for several years [9]. In our country, available treatments are limited to conventional therapies, which limits the aggressive management recommended in severe forms, or in severe acute colitis [1,10]. Two patients underwent emergency surgery for small bowel perforation peritonitis during CD.
Follow-up of IBD patients is difficult. In our series, 17/26 cases of loss of sight were observed. The reasons for this were not evaluated in this study. For some authors, the reasons for poor compliance included the relationship established with the physician, depression, subjective quality of life, health status evaluation and the therapeutic benefit/treatment burden ratio [11,12].
Mortality is high in IBD patients compared with the general population. Gismera and colleagues found a mortality of 5%, and mortality risk factors vary from study to study, but death was more often related to CD than UC for Nocerino and colleagues [13,14]. Ano-perineal lesions and disease severity were the risk factors for death observed in our series. Dia and colleagues in Dakar reported two cases of severe acute colitis treated by conventional means and with lethal evolution [15]. The lack of biotherapy could be considered a risk factor for death in our context. However, the single-center nature of this study may be a source of patient selection bias.
Conclusion
Keeping IBD patients on the care circuit is a multidisciplinary challenge to reduce the proportion of patients lost to follow- up, and improving the management of severe forms with non- conventional treatments should change the prognosis of IBD at Brazzaville University Hospital.
References
- Reyt V. Crohn’s disease and its treatment. Actual Pharm. 2019; 58: 44-48.
- Klotz C, Barret M, Dhooge M, et Hemorrhagic rectocolitis: diagnostic and therapeutic management. Presse Médicale. 2015; 44:144-149.
- Mimiesse JF, Deby-Gassaye, Atipo-Ibara BI, et al. Crohn’s disease: first description at Brazzaville University Hospital. J Afr Hépato-Gastroentérologie. 2015; 9: 73-75.
- https://www.bibliosante.ml/handle/123456789/4056
- Medhioub M, Khsiba A, Mahmoudi M, et al. Characteristics of chronic inflammatory bowel disease in the elderly. Rev Médecine Interne. 2023; 44: A234.
- Hassine A, Hammami A, Ben Ameur W, et al. Chronic inflammatory bowel diseases of the elderly: epidemio-clinical, therapeutic and evolutionary profile. Rev Médecine Interne. 2022; 43: A205.
- Siala A, Boudabous M, Chtourou L, et al. Epidemio-clinical profile of chronic inflammatory bowel disease in the elderly. Rev Médecine Interne. 2016; 37: A148.
- Gowze-Rousseau C, Fumery M, Savoye G, et al. John Libbey Eurotext - Hepato-Gastro & Digestive Oncology - Epidemiology and natural history of chronic inflammatory bowel disease in children. Hepato-Gastro Oncol Dig. 2018; 25: 895-902.
- Reenaers C, Louis E. New developments in the management of chronic inflammatory bowel disease. Rev Médicale Liège. 2022; 77: 323-329.
- Beaugerie Chronic Inflammatory Bowel Diseases (CIBD): what place for conventional treatments? Acta Endosc. 2008; 38: 359-374.
- Tahri N. Therapeutic compliance and chronic inflammatory bowel diseases. Presse Médicale. 2007; 36: 1236-1243.
- Banovic I, Gilibert D, Olivier M, et Compliance and some of its determinants in chronic inflammatory bowel disease (IBD). Prat Psychol. 2010; 16: 157-172.
- Saro Gismera C, Lacort Fernández M, Argüelles Fernández G, et Mortality and causes of death in patients with chronic inflammatory bowel disease in Gijón, Asturias (Spain). Rev Esp Enferm Dig. 1999; 91: 199-208.
- Nocerino A, Feathers A, Ivanina E, et al. Mortality Risk of Inflammatory Bowel Disease: A Case-Control Study of New York State Death Dig Dis Sci. 2019; 64: 1604-1611.
- Dia D, Cisse M, Diouf G, et Severe acute colitis: Two fatal cases in Dakar. Med Sante Trop. 2014; 24: 438-440.