Factors Associated with the Refusal of Vaccination Against COVID-19 Among Students of The Faculty of Health Sciences of Congo
Author'(s): Ange clauvel Niama1 , Yvonne Valérie Yolande Mavoungou1, Gilbert Ndziessi1,2, Kévine Ikoungou1, Chéripin Ngamille1, and Sophie Bayonne1
1 Faculty of Health Sciences, Congo.
2 Centre for Public Health Emergency Operations, Congo.
*Correspondence:
Yvonne Valérie Yolande MAVOUNGOU, Faculty of Health Sciences, Marien Ngouabi University, Brazzaville, Congo.
Received: 04 Apr 2022; Accepted: 26 Apr 2022; Published: 02 May 2022
Citation: NIAMA AC, MAVOUNGOU YVY, NDZIESSI G, et al. Factors Associated with the Refusal of Vaccination Against COVID-19 Among Students of The Faculty of Health Sciences of Congo. Clin Immunol Res. 2022; 6(1): 1-6.
Abstract
Background: COVID-19 is responsible for high morbidity and mortality. Vaccination is the main response strategy. Vaccination coverage remains low. This study investigated the factors for refusal of COVID-19 vaccination among health sciences students.
Methodology: This was an analytical cross-sectional study conducted from July to October 2021. The cluster method was used and the Schwartz formula was used to obtain the minimum sample size. Socio-demographic, socio-cultural and vaccination status variables were collected. Statistical analysis was performed with Epi Info 7.2.2.6 software. The significance level was set at 5%
Results: A total of 423 students were included. Vaccination coverage was 12.77%. The rate of students refractory to vaccination was 45.62%. Females were in the majority (54.40% vs 54.60%). The factors associated with refusal of the COVID-19 vaccination in our study were: lack of knowledge of the vaccines available in Congo (ORa=1.601 [1.009-2.539]; p=0.0453), perception of the uselessness of the vaccine (ORa=6.055 [3.646-10.055]; p < 0.0001) and the unavailability of the vaccine the student wishes to receive (ORa=2.652 [1.365-5.152]; p = 0.004).
Conclusion: This study reveals low vaccination coverage and almost half of the students were refractory to vaccination against COVID-19. Awareness and involvement of students in health sciences who are public health actors are necessary to improve this vaccination coverage.
Keywords
Abbrivation
*OR a = Odd Ratio adjusted.
Introduction
Since its discovery in December 2019, the SARS-CoV-2 virus, which causes the 2019 coronavirus disease named COVID-19, has been responsible for 4.2 millions deaths worldwide by the end of July 2021 [1]. In Congo, the first confirmed case of COVID-19 was reported on 14th March 2020. As of 30th July 2021, 13216 confirmed cases of COVID-19 had been reported and 178 deaths were reported [2]. Of those affected by COVID-19, 14% to 19% are hospitalised and 3% to 5% are admitted to an intensive care unit [3]. Those over 60 years of age and those with co-morbidities such as diabetes, hypertension, heart disease, chronic lung disease and cancer are at risk of severe forms or death [4]. In young people, COVID-19 also has health implications [5]. In response to this concern, the Congolese government has taken measures to limit the spread of the virus. Initially, a state of health emergency was declared. This included house arrest, curfew, closure of borders, closure of bars, churches, restaurants, schools and universities. In terms of health, preventive measures were the preferred response strategies, including physical distancing, compulsory wearing of masks and regular hand washing. These measures proved to be insufficient [6]. Vaccination in a second phase reinforced the initial measures and is the priority response strategy proposed by the WHO. Vaccination against COVID-19 began on March 23rd 2021, with priority given to at-risk groups. It was extended to the entire adult population on May 4th 2021.
The promotion of vaccination among young people should be a priority because they are a potential vector population for the virus [7]. Among young people, the students of the Faculty of Health Sciences are important public health actors. This is especially true since their lives revolve around their families, their place of study and the health care centres where they spend their practical training. Their attitude towards vaccination may influence the behaviour of those around them and of other members of society on whether or not they should be vaccinated. Thus, a better understanding of the factors that motivate the refusal of vaccination would make it possible to propose effective measures to improve vaccination coverage against COVID-19. It is to this end that this study was conducted with the objective of highlighting the factors associated with refusal of the COVID-19 vaccination among health sciences students in Congo.
Methodology
Type and Period of study
This was an analytical cross-sectional study conducted from 15th July to 15th October 2021.
Study setting
The study took place at the Faculty of Health Sciences the Université Marien Ngouabi de Brazzaville (UMNG) in Congo, which is one of the eleven institutions of the UMNG. It offers training in the field of health sciences, namely medicine and four paramedical courses including public health, biomedical sciences, midwifery and nursing.
Study population
Target population: The target population for our study was students enrolled at the Faculty of Health Sciences.
Inclusion criteria: Enrolled students who were at least 18 years of age and willing to participate in the study were selected to participate in the survey.
Non-inclusion criteria: Student doctors enrolled in a specialised diploma course were not included in the study because their training site is not the Faculty of Health Sciences.
Sampling
The two-stage cluster sampling method was used. A first random draw consisted of selecting three training paths from the five (05) offered at the Faculty of Health Sciences. A second random draw consisted of obtaining two academic levels within these pathways. The number of students interviewed per pathway was estimated according to the proportion of the total health sciences student body.
Sample size
The minimum sample size was calculated with the Daniel SCHWARTZ formula presented below.
N≥ (Z_(α/2)^2×p×(1-p))/d^2
N = required sample size
Zα/2: Confidence level, whose standard value at a 95% level = 1.96 at the 5% threshold
p = frequency of vaccine refusal chosen to be 50%; d = precision = 5% or 0.05
The required sample size according to the Schwartz formula was: N= ((1.96)² x 0.5x(1-0.5))/((0.05 )²) = 384 students as the minimum number of study subjects.
Data collection and variables studied
Data collection was based on an anonymous paper questionnaire. The dependent variable was the "refractoriness" of the student. The independent variables were : socio-demographic variables, socio-cultural variables and vaccine variable.
Operational definitions
Vaccinated person: a person who reports having received at least one dose of COVID-19 vaccine.
Unvaccinated person: a person who reports never having received at least one dose of COVID-19 vaccine.
Vaccine Refractory Person: a person who reports never having received at least one dose of COVID-19 vaccine and who refuses to receive at least one dose of the vaccine.
Ajzen's Theory of Planned Behaviour categorised the behavioural variables into the following groups (8) :
- Attitude towards the behaviour : this is the individual's perception of the behaviour;
- Subjective norms : this is the social pressure or influence of society on the behaviour as perceived by the individual ;
- Perceived behavioural control : this is the individual's experience on the ease or difficulty of performing a behaviour.
Data capture and analysis
Data entry and analysis were carried out using Epi-Info7.4.2 software. Categorical variables were expressed as absolute values and frequencies. Pearson's Chi-square or Fischer's tests, where appropriate, were used for comparison. Quantitative variables were expressed as mean and standard deviation. The Student's t test or ANOVA test was used to compare them. Top-down stepwise logistic regression was performed to identify factors associated with students' refusal of vaccination. Odds ratios (OR) and their 95% confidence intervals were calculated to assess the strength of association between the different variables. The significance threshold used was p-value <0.05.
Ethical considerations
The implementation of this study was carried out after obtaining permission from the Faculty of Health Sciences Ethics Committee. Confidentiality, anonymity and informed consent were respected.
The data collected was used only for the purpose of this research. The rights of respondents were respected, particularly those relating to freedom of opinion.
Results
Characteristics of the study population
A total of 423 health sciences students were surveyed. There were 215 women (50.83%) and 208 men (49.17%). The mean age was 22 years 3.3 (18-49). The median age was 22 years. 410 students were single (96.93%), 11 were in a relationship (2.60%) and 02 were married (0.47%). Of the students surveyed 343 (81.09%) lived with their parents and 80 (18.91%) lived alone.
Vaccination coverage and characteristics of refractory students 54 students (12.77%) reported being vaccinated against COVID-19 and 369 students (87.23%) reported not having received a COVID-19 vaccine. Of the 423 students surveyed, 193 students (45.62%) were resistant to vaccination. Among the group of resistant students, 188 were single (97.41%), four were cohabiting (2.07%) and one was married (0.52%). Of these, 145 were enrolled in the Medicine stream (75.13%), 19 in the Public Health stream (9.84%) and 29 in the Biomedical Sciences stream (15.03%).
Educational background, gender and refusal of vaccination against COVID-19 in univariate analysis
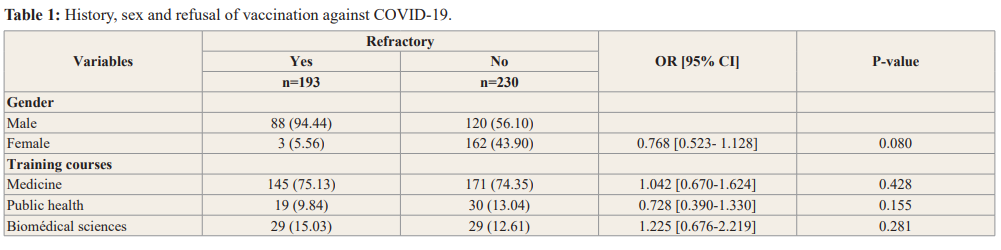
As no variable was discriminated, there was no statistically significant association between background, gender and vaccination refusal see table 1.
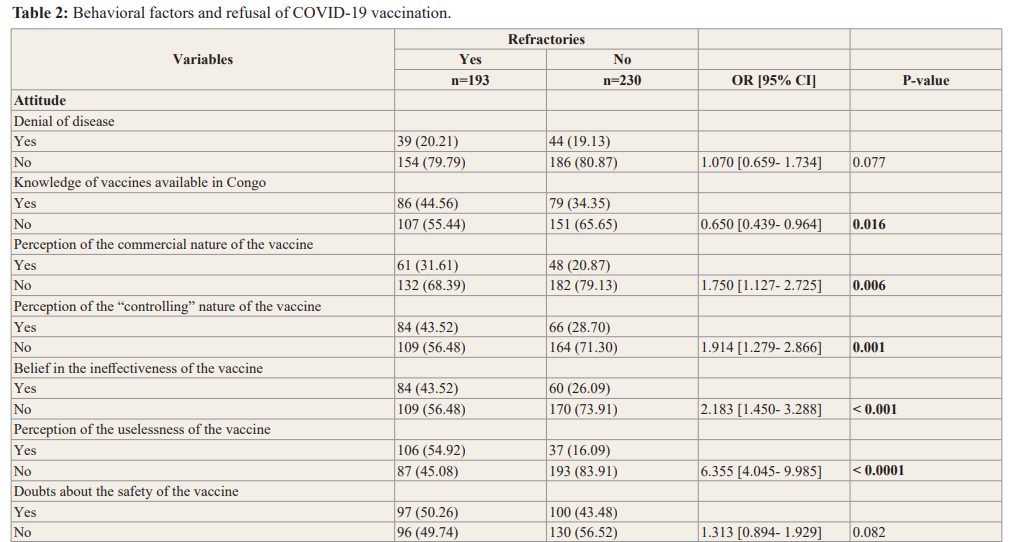
In univariate analysis, the factors significantly associated with refusal of COVID-19 vaccination among health sciences students were: knowledge of available vaccines, perception of the commercial nature of the vaccine, perception of the "controlling" nature of the vaccine, belief in the ineffectiveness of the vaccine, perception of the uselessness of the vaccine, fear of side-effects, and non-availability of desired vaccines in table 2.
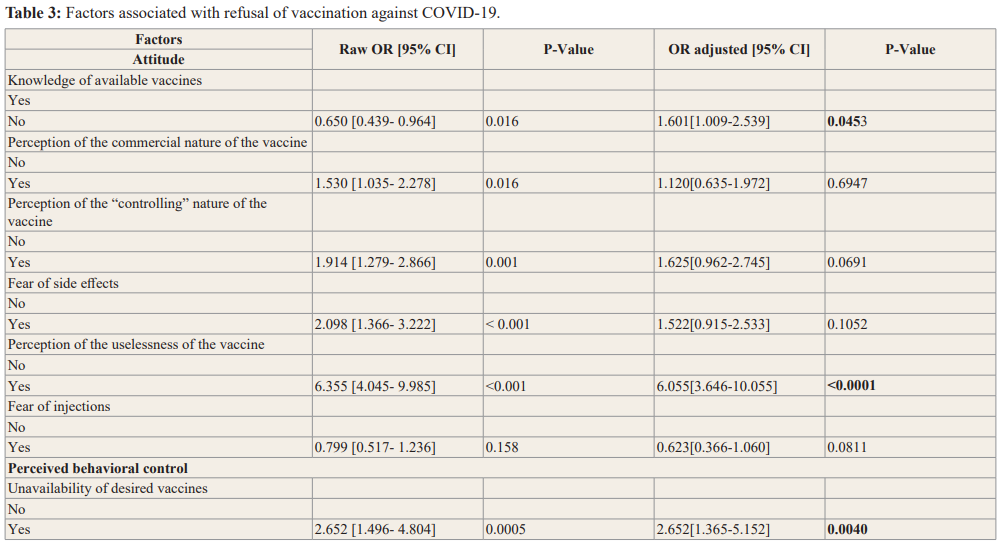
Multivariate analysis of factors for refusal of vaccination against COVID-19
Multivariate analysis showed that lack of knowledge of the vaccines available in Congo (p=0.0453), perceived uselessness of the vaccine (p < 0.0001) and unavailability of the vaccine the student wanted to receive (p = 0.004) were significantly associated with refusal of the COVID-19 vaccination at the Faculty of Health Sciences (Table 3).
Discussion
COVID-19 vaccination coverage among health sciences students
Our study reveals that 12.77% of Faculty of Health Sciences students are vaccinated against COVID-19. Vaccination coverage of health sciences students is low compared to the vaccination target that Congo has set itself, namely "to vaccinate 60% of the population by the end of 2022". This coverage was close to the national vaccination coverage estimated at 10.82% of the Congolese population [9]. In the USA, Diesel and Baack report respectively a vaccination coverage against COVID-19 of 38.3% among adults aged 18 to 29 years and 34% among adults aged 18 to 39 years [10,11]. Low vaccination coverage among young adults is also noted in Brazil, where 5% of people aged 20-39 years were vaccinated in May 2021 compared to 80% of people aged 60-69 years [12].
Rate of students refusing to be vaccinated against COVID-19 The present study shows that 45.62% of health sciences students were resistant to COVID-19 vaccination. This should be of concern with regard to the role that health science students could play in promoting COVID-19 vaccination. The high rate of refusal of COVID-19 vaccination is also reported in Michigan in the USA, 44.2% of dental students and 47% of medical students were resistant to vaccination [13,14]. In medical schools in India, the rate of refusal to vaccinate against COVID-19 was lower, estimated at 10.3% [15]. In the initial epicentre of the pandemic, Wuhan, China, 58.2% of students in six health sciences training institutions expressed reluctance to receive COVID-19 vaccination [16]. These data illustrate that refusal to vaccinate against COVID-19 remains a weakness in achieving health goals in many countries.
Characteristics of COVID-19 vaccine-refractory students
The majority of health sciences students who refused to be vaccinated against COVID-19 were in the 20-24 age group (74.61%). A predominance of females was noted (54.40%). These findings are consistent with those of other studies conducted in health sciences training institutions [13,14].
Factors associated with refusal of the COVID-19 vaccination
In general, the decision whether or not to be vaccinated to prevent

infection depends on several factors. A meta-analysis using data from 149 countries identified the following factors: perceived importance of the vaccine, perceived safety of the vaccine, confidence in the efficacy of the vaccine and accessibility of the vaccine [17].
The present study did not find evidence that gender was involved in attitudes towards COVID-19 vaccination. The opposite results were found by Faezi et al. who found that female gender was statistically associated with refusal of COVID-19 vaccination [18]. The factors associated with refusal of COVID-19 vaccination in our study were lack of knowledge of the vaccines available in Congo (ORa=1.601 [1.009-2.539]; p=0.0453), perceived uselessness of the vaccine (ORa=6.055 [3.646-10.055]; p < 0.0001), and unavailability of the vaccine the student wishes to receive (ORa=2.652 [1.365-5.152]; p = 0.004).
Attitudes influencing vaccine refusal have been studied in several parts of the world. In Nigeria, low knowledge of COVID vaccines was reported to influence COVID-19 vaccine refusal in the university setting [19]. A multicentre study including the Democratic Republic of Congo, Benin, Mali, Uganda, Brazil
and some Asian countries shows that fear of side effects and lack of confidence in the efficacy of the COVID-19 vaccine were associated with vaccine refusal [20]. In academic settings, India and Nigeria, doubt about the efficacy of the vaccine and concerns about vaccine safety are the main factors associated with refusal of COVID-19 vaccination [15,20].
In our research, doubt about vaccine efficacy was not associated with refusal of COVID-19 vaccination in multivariate analysis.
Our work shows that not believing in Coronavirus disease does not influence vaccine intention. In Nigeria, it is reported that disbelief in the existence of COVID-19 negatively influenced the vaccination decision in the university setting [20].
Nearly a third of health sciences students (35.46%) believe that the COVID-19 vaccine is a means of controlling the world's population. This perception has no influence on the refusal of vaccination. This is not the case in the study by Bono et al. which shows that, in the African countries mentioned above, refusal to vaccinate was associated with a belief that the COVID-19 vaccine was designed to harm the population [19].
Our study shows that fear of vaccine side effects does not influence vaccine intention. The opposite was found in Kingston, USA, where fear of side effects was associated with vaccine refusal among students at a pharmacy school [21].
The lack of association between religious beliefs and refusal to vaccinate against COVID-19 contradicts the finding in Malaysia where religion was a factor negatively influencing vaccine intention [22].
These results argue in favour of behaviour change communication interventions for health sciences students who are the future doctors and managers of the health system in the Republic of Congo. Several communication strategies, including social networks, should be used to reach this audience in order to protect them from COVID-19 and reduce the spread of this pandemic through their involvement in prevention.
Conclusion
This study showed low vaccination coverage against COVID-19 among health sciences students and revealed that almost half of the students were resistant to vaccination. Improving interest in COVID-19 vaccination, addressing the problems of accessibility and availability of vaccines could avoid the factors of refusal of COVID-19 vaccination.
References
- https://covid19.who.int/
- Organisation Mondiale de la Santé. SITREP n° 165 du 30 juillet 2021 [Internet]. Disponible à l’URL SITREP_N_165- COVID-19-CONGO_DU_30_JUILLET 2021 pdf who.int. Consulté le 02 aout. 2021.
- Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocoln prospective observational cohort study. BMJ. 2020; 369.
- Lu L, Zhong W, Bian Z, et al. A comparison of mortality-related risk factors of COVID-19 SARS and MERS a systematic review and meta-analysis. J Infect. 2020; 81: e18-e25.
- Guedes da Silva Junior FG, E Silva Sales JC, de Souza Monteiro CF, et Impact of COVID-19 pandemic on mental health of young people and adults a systematic review protocol of observational studies. BMJ Open. 2020; 10: e039426.
- Bistoquet M, Hermabessiere S, Villard O, et al. Evaluer l’efficacité des mesures barrières pour limiter la transmission nosocomiale du SARS-CoV-2 étude EMBELLIE. Med Mal Infect. 2020; 50: S64.
- Huang L, Zhang X, Zhang X, et al. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16-23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing J Infect. 2020; 80: e1-e13.
- Ajzen The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991; 50: 179-211.
- https://afro.who.int/sites/default/files/2021-11/SITREP_N_198-COVID-19-CONGO_DU_19_ NOVEMBRE.pdf.
- Diesel J, Sterrett N, Dasgupta S, et COVID-19 Vaccination Coverage Among Adults - United States December 14, 2020- May 22, 2021. Morb Mortal Wkly Rep CDC. 2021; 70: 922-927.
- Baack BN, Abad N, Yankey D, et COVID-19 Vaccination Coverage and Intent Among Adults Aged 18-39 Years United States March-May 202. Morb Mortal Wkly Rep CDC. 2021; 70: 928-933.
- Kupek E. Low COVID-19 vaccination coverage and high COVID-19 mortality rates in Brazilian elderly. Rev Bras Epidemiol. 2021; 24: e210041.
- Mascarenhas AK, Lucia VC, Kelekar A, et Dental students' attitudes and hesitancy toward COVID-19 vaccine. J Dent Educ. 2021; 85: 1504-1510.
- Lucia VC, Kelekar A, Afonso NM. COVID-19 vaccine hesitancy among medical J Public Health. 2021; 43: 445-449.
- Jain J, Saurabh S, Kumar P, et COVID-19 vaccine hesitancy among medical students in India. Epidemiol Infect. 2021; 149: e132.
- Gao X, Li H, He X, et al. COVID-19 Vaccine Hesitancy Among Medical Students The Next COVID-19 Challenge in Wuhan Disaster Med Public Health Prep. 2021; 9: 1-6.
- De Figueiredo A, Simas C, Karafillakis E, et al. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake a large scale retrospective temporal modeling Lancet. 2020; 396: 898-908.
- Faezi NA, Gholizadeh P, Sanogo M, et al. Peoples' attitude toward COVID-19 vaccine acceptance and social trust among African and Middle East countries. Health Promot Perspect. 2021; 11: 171-178.
- Uzochukwu IC, Eleje GU , Nwankwo CH, et al. COVID-19 vaccine hesitancy among staff and students in a Nigerian tertiary educational institution. Ther Adv Infect Dis. 2021; 8: 1-12.
- Bono SA, Villela EF, Siau CS, et al. Factors Affecting COVID-19 Vaccine Acceptance: An International Survey among Lowand Middle-Income Vaccines. 2021; 9: 515.
- Silva J, Bratberg J, Lemay COVID-19 and influenza vaccine hesitancy among college students. J Am Pharm Assoc. 2021; 61: 709-714.
- Syed Alwi SAR, Rafidah E, Zurraini A, et A survey on COVID-19 vaccine acceptance and concern among Malaysians. BMC Public Health. 2021; 21: 1129.