Hepatocellular Carcinoma Arising From Viral B Cirrhosis at the Chu De L'amitie Sino-Centrafricain in Bangui
Author'(s): Boua-Akelelo NP1*, Youssouf O2, Ignaléamoko Word NE1, Mofini E1, Elowa JB1, Bessanguem B1, Komaria H1, Armand2, Yangba Kalebanga AOT1, Service G3 and Camengo Police SM1
1Service d'Hépato-Gastroentérologie CHU de l'Amitié Sinocentrafricaine, Bangui.
2Department of Internal Medicine CHU Communautaire, Bangui.
3Department of Internal Medicine CHU Maman Elisabeth Domitien, Bimbo.
*Correspondence:
Boua Akélélo, Service d'Hépato-Gastroentérologie CHU de l'Amitié Sino-centrafricaine, Bangui, Tel: 0023675392430.
Received: 30 Apr 2024 Accepted: 04 May 2024 Published: 12 May 2024
Citation: Boua-Akelelo NP, Youssouf O, Ignaléamoko Word NE, et al. Hepatocellular Carcinoma Arising From Viral B Cirrhosis at the Chu De L'amitie Sino-Centrafricain in Bangui. Gastroint Hepatol Dig Dis. 2024; 7(2): 1-5.
Abstract
Introduction: Hepatocellular carcinoma (HCC) is a public health problem. It is the most frequent cause of death in patients with decompensated cirrhosis [1].
Objective: To help improve the management of hepatocellular carcinoma (HCC).
Patients and Methods: We conducted a cross-sectional analytical study covering the period from 1er January 2020 to 31 October 2022 in the Hepato-Gastroenterology Department of the Centre Hospitalier Universitaire de l'Amitié Sino-centrafricaine (CHUASC) in Bangui. We included in the study patients of both sexes aged at least 18 years with a diagnosis of HCC due to hepatitis B virus (HBV). Patients were divided into two groups (HCC without cirrhosis and HCC with cirrhosis). The study variables were epidemiological, clinical, biological and morphological. Data were entered and analysed using Epi Info version 7 software. The Chi2 test was used for comparison, with a significance level of p ? 0.05.
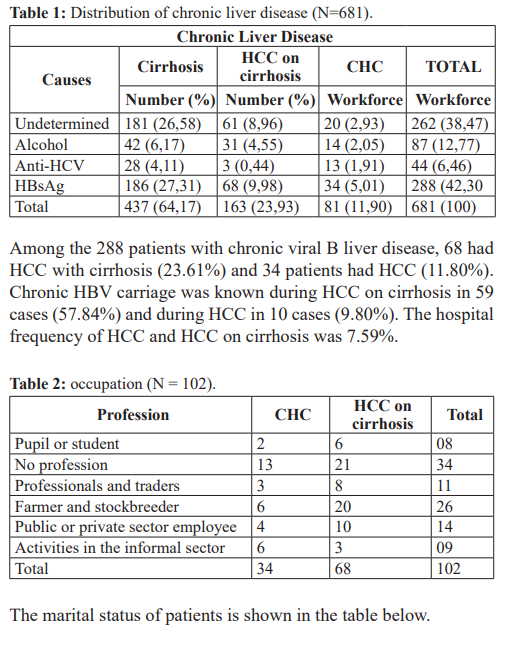
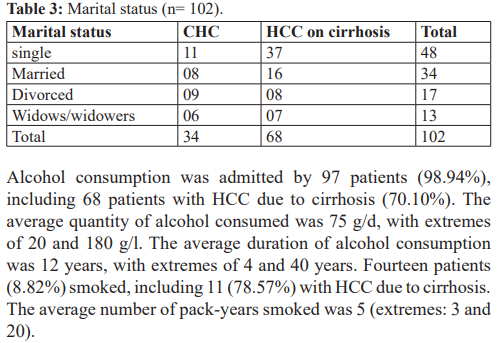
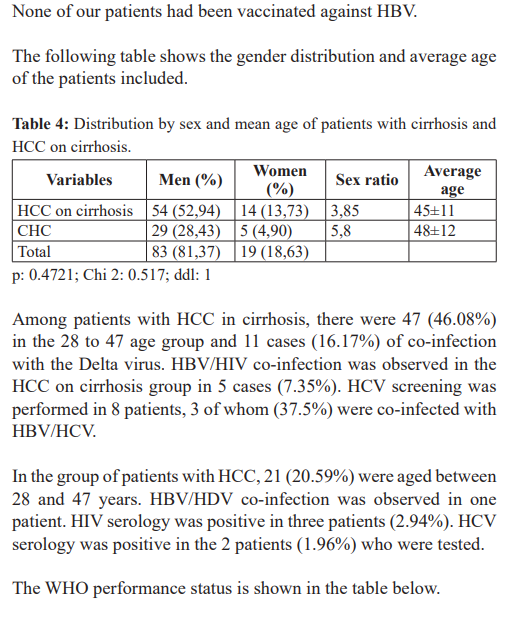
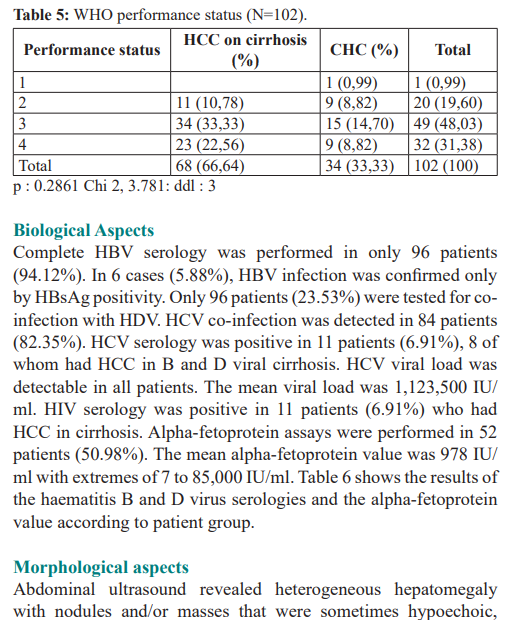
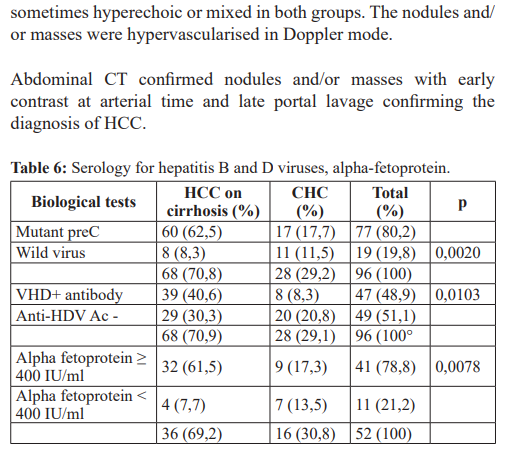
Results: During the study period, 1344 patients were hospitalised, of whom 681 had chronic liver disease (51%), 288 cases (42.30%) had cirrhosis and/or HCC due to HBV. The hospital incidence of HCC and HCC on cirrhosis was 7.59%. We identified 68 patients (23.61%) with HCC due to cirrhosis (sex ratio: 3.85) and 34 patients (11.80%) with HCC without cirrhosis (sex ratio: 5.8). The mean age of patients with HCC on cirrhosis was 45±11 years and that of patients with HCC without cirrhosis was 48±12 years. In both groups, half of the patients had WHO performance status 3. The alpha-fetoprotein value was ≥ 400 IU/ml in 61.5% of patients with HCC in cirrhosis and in 17.3% of patients with HCC without cirrhosis. Morphologically, the liver was enlarged, multiheteronodular and hypervascularised on Doppler ultrasound and abdominal CT. According to the BCLC (Barcelona-Clinic Liver Cancer) classification, patients with HCC in cirrhosis were stage C in 9 cases (13.23%) and stage D in 59 cases (88.14%). The Okuda classification used to assess the severity of HCC in the 34 patients classified them as stage 2 in 11 cases (32.35%) and stage D in 23 cases (67.65%).
Conclusion: HCC occurs very frequently in young adults with viral B cirrhosis. It is diagnosed late in patients with several nodules that do not allow curative treatment.
Keywords
Introduction
Hepatocellular carcinoma can occur in a healthy liver or in a liver previously damaged by HBV (Hepatitis B Virus). HCC is the most frequent cause of death in patients with decompensated cirrhosis [1]. There is now no doubt that chronic HBV infection exposes patients to the risk of HCC [2]. According to the WHO, more than 91 million Africans are living with hepatitis B or C [3]. The high prevalence of HBV carriage in sub-Saharan Africa classifies the region as highly endemic [4,5]. In this region of Africa, the prevalence of HBV varies from country to country. It is 11% in Senegal [6], 13.5% in Chad [7] and 16.14% in Mali [8]. In the Central African Republic, depending on the population studied, prevalence varies from 10.6% to 19.8% [9-13]. In the Maghreb, on the other hand, the highest HBV prevalence is reported in Algeria (2-8%) and Libya (5.8%) [14]. Chronic infection can progress to cirrhosis and then HCC. However, it can also progress from chronic infection to HCC without cirrhosis. In the West, HCC is discovered early during cirrhosis monitoring [15]. In sub-Saharan Africa, however, HCC is discovered late [16]. In Bangui, HCC accounts for 20.2% of HCC complications [17]. The aim of this study was to describe the epidemiological, clinical, biological and prognostic characteristics of HCC arising from viral B cirrhosis.
Method Patients
Between 1st January 2020 and 31 October 2022, a period of one year and ten months, we conducted a cross-sectional analytical study in the Hepato-Gastroenterology (HGE) department of the Centre Hospitalier Universitaire de l'Amitié Sino-centrafricaine (CHUASC) in Bangui. Data collection was retrospective from 1er January 2020 to 31 March 2022 and prospective from 1st April 2022 to 31 October 2022. Our study population consisted of patients hospitalised in the HGE (Hepato-Gastro-Enterology) department during the study period. We consecutively included patients aged at least 18 years, of both sexes, with a diagnosis of hepatocellular carcinoma (HCC) due to hepatitis B virus (HBV). Patients were divided into two groups: HCC with cirrhosis and HCC without cirrhosis. The diagnosis of HCC due to cirrhosis was based on clinical and biological signs of hepatocellular insufficiency (HCI); clinical, ultrasound and endoscopic signs of portal hypertension (PH); in the case of a palpable liver, a large, hard, woody, stony liver with an irregular surface, tender or painful at the lower edges, whether or not associated with elevation of alpha-fetoprotein ≥ 400 IU/ml on biology, the presence of a heterogeneous liver with masses and/or nodules on ultrasound and the presence of hypervascularised liver lesions on abdominal computed tomography at arterial time and late portal lavage. HBV was incriminated if the following serological markers were detected: positive HBS antigen, positive HBV viral load. If HBsAg was positive, co-infection with HDV was sought. Our sample was of convenience. Data were collected using an individual direct-administration survey form. Information was obtained from medical records, patients and hospital registers. The variables studied were sociodemographic, clinical, biological, morphological and prognostic characteristics. Data were analysed using Epi info 7 software. We used the pearson chi² test with a significance level of 5% for comparison. The BCLC and Okouda classifications were used to assess prognosis and the WHO classification to assess the general condition of our patients.
Results
Epidemiological aspects
Of the 1344 patients hospitalised during the study period, 681 had chronic liver disease (51%). The table below shows the different types of chronic liver disease observed.
Morphological aspects
Abdominal ultrasound revealed heterogeneous hepatomegaly with nodules and/or masses that were sometimes hypoechoic, sometimes hyperechoic or mixed in both groups. The nodules and/ or masses were hypervascularised in Doppler mode.
Abdominal CT confirmed nodules and/or masses with early contrast at arterial time and late portal lavage confirming the diagnosis of HCC.
Prognostic aspects
Patients with HCC in cirrhosis had severe hepatocellular insufficiency (class B) in 27 cases (39.70%) and very severe hepatocellular insufficiency in 41 cases (60.30%).
According to the BCLC classification, patients with HCC in cirrhosis were stage C in 9 cases (13.23%) and stage D in 59 cases (88.14%). The Okuda classification used to assess the severity of HCC in the 34 patients classified them as stage 2 in 11 cases (32.35%) and stage 1 in 23 cases (67.65%).
Discussion
The limits of the study
The diagnosis of cirrhosis and HCC was made on clinical, biological and morphological grounds without recourse to liver biopsy. It is accepted that when epidemiological, clinical, biological, radiological and endoscopic evidence concurs, the diagnosis of cirrhosis can be made without necessarily resorting to a HSP for histological analysis, or by using other non-invasive means [18]. Non-invasive tests for fibrosis, in particular blood tests and elastometry, now make it possible to confirm significant fibrosis without recourse to PBH. Abdominal CT is becoming an examination that allows positive diagnosis of HCC without recourse to PBH for histological analysis. The significant elevation of alpha-fetoprotein in our HCC patients was also an argument in favour of the diagnosis. However, our study provided data that should be compared with those of other authors. HCC accounts for 35.83% of chronic liver disease, 14.99% of which is due to HBV. The hospital frequency of HCC and HCC in cirrhosis is 7.59%. This is higher than the 4.7% reported in a previous study in the department [19]. Heavy alcohol consumption admitted by 97 patients in our series and co-infection with HDV in 47 (48.9) patients could be factors in the progression of the disease towards complications. In our study, HCC occurred in 66.64% of patients with cirrhosis. HCC accounted for 20.2% of cirrhosis complications in 2011 [17]. In Italy, the authors reported that 93.1% of HCC occurred in cirrhosis [20]. In the USA, most HCC occurs in cirrhosis [21]. Other European authors have reported that HCC is the cause of death in 54 to 70% of cases in patients with compensated cirrhosis [22]. In a French study, the incidence rate of HBV-related HCC was higher than that of HCV-related HCC [23]. In Cotonou, the authors observed HCC in cirrhosis in 42.3% of cases [24] and 54.3% of cases [25]. However, in Marrakech, the authors recorded 72.3% of cases of HCC in cirrhosis [26]. All this bears witness to the frequency of HCC in cirrhosis. Regular and rigorous monitoring of cirrhosis should enable early diagnosis of HCC. HBV remains the leading cause of cirrhosis and/or HCC in Bangui [17,19], in other sub-Saharan African countries [5,7,8,16,24-27,29] and in India [28]. In Italy [20] and Marrakech [26], the hepatitis C virus came before HBV. These results testify to the role of chronic HBV and HCV infection in the genesis of HCC [30]. Alcohol consumption, found in previous studies in Bangui [17,19] and reported in other studies [25,28] with varying frequencies, could be one of the factors favouring the progression of liver disease. The male predominance observed in our series corroborates the data in the literature [20-23,25-29]. The mean age of our patients with HCC due to cirrhosis (45 ± 11 years) was slightly lower than that of patients with HCC without cirrhosis (48 ± 12 years). The mean age of our patients is decreasing. It was 50 ± 16 years in a previous study [19]. It is lower than the mean age reported by authors in Cotonou, which is 53 ± 16.3 years [25], but similar in another study (42.6 years) [29]. In Ouagadougou, the mean age of 43.9 ±11.8 years is similar to ours [31]. However, in Marrakech, the authors found a mean age of 59 years [26]. In sub- Saharan Africa, HCC occurs very early. This could be linked to the fact that sub-Saharan Africa is located in a zone of high HBV endemicity and that in most cases, B viral infection goes undetected and is diagnosed at the stage of complications. The mean alpha- fetoprotein value in our patients was 978 IU/ml. Elevation of alpha-fetoprotein was also reported by authors in Cotonou [25], Marrakech [26] and Ouagadougou [31]. Alpha-fetoprotein also remains the marker for the diagnosis of HCC during monitoring of cirrhosis. The multi-nodular appearance of the liver found in our study has also been reported by other authors [25,26,29,31]. The presence of multiple nodules does not offer patients the possibility of radical treatment. The majority of our patients with HCC in cirrhosis were in stage D BCLC. In Marrakech [26] and Cotonou [25], the authors reported that 50% of patients were at stage D and more than 50% at stage C. HCC is often diagnosed at an advanced stage, making curative treatment impossible.
Conclusion
HCC remains a public health problem, due to its frequency and late diagnosis, with no possibility of radical treatment. It is important to raise public awareness, screen for chronic viral infections and manage patients who are chronic carriers of hepatotropic viruses. Vaccination remains an effective means of reducing the incidence of liver disease.
Ethical approval
Declaration for human rights: Participants: This study was approved by the ethics committee and the principles of the Declaration of Helsinki were followed.
Authors' contributions
All the authors contributed to the conduct of this work. They also declare that they have read and approved the final version of the manuscript.
References
- Fattovich G, Stroffolini T, Zagni I, et Hepatocellular Carcinoma in Cirrhosis: Incidence and Risk Factors. Gastroenterology. 2004; 127: S35-S50.
- Sallie R, Di Bisceglie AM. Viral hepatitis and hepatocellular Gastroenterol Clin North Am. 1994; 23: 567-579.
- https//afro.who.int/fr/news/99-millions-dafricains-infectes-par-lhepatite-b-ou-c
- Kramvis A, Kew MC. Epidemiology of hepatitis B virus in Africa, its genotypes and clinical associations of genotypes. Hepatology 2007; 37: S9-S19.
- Kew MC. Epidemiology of HBV infection and HBV related hepatocellular carcinoma in Africa: Natural history and clinical ISBT Science series. 2006; 1: 84-88.
- Mbaye PS, Ranaudineau Y, Diallo A, et al. Hepatitis C virus and hepatocellular carcinoma in Dakar: case-control study. Médecine 2000; 60: 47-52.
- Mahamat moussa A, Mahamat H, Adoum NA, et Seroprevalence of AgHbs in patients with liver cirrhosis and hepatocellular carcinoma in Ndjamena, Chad. Annales de l'Université de Bangui Série D. 2017; 3: 24-28.
- Diarra M, Konate A, Dembele M, et Hepatocellular carcinoma: epidemiological and evolutionary aspects. Médecine d'Afrique Noire. 2006; 53: 23-28.
- Komas NP, Vickos U, Hübschen JM, et al. Cross-sectional study of hepatitis B virus infection in rural communities, Central African Republic. BMC Infectious Diseases. 2013; 13: 286.
- Komas NP, Baï-Sepou S, Manirakiza A, et al. The prevalence of hepatitis B virus markers in a cohort of students in Bangui, Central African Republic. BMC Infectious Diseases. 2010; 10: 226-231.
- Camengo Police SM, Longo JDD, Mbeko Simaleko M, et al. Prevalence of HBsAg among sex workers in Bangui. Annales de l'Université de Bangui, Série 2015; 1: 43-46.
- Packo DSS, Tomlbaye FO, Conde A, et al. Epidemiological and clinical characteristics of blood donors co-infected with HIV and HBV at the Bangui national blood transfusion Health and Science Disease. 2022; 23: 46-48.
- Camengo Police SM, Mbeko Simaleko M, Mossoro Kpinde CD, et al. Prevalence of HBsAg among male homosexuals in Médecine d'Afrique Noire. 2013; 60: 513-518.
- Lahlali M, Abid H, Lamine A, et al. Epidemiology of viral hepatitis in the Greater Maghreb. La Tunisie Médicale. 2018; 96: 606-619.
- Nordenstedt H, White DL, El-Serag The Changing Pattern of Epidemiology in Hepatocellular Carcinoma. Digestive Liver Disease. 2010; 42: S206-S214.
- Nikiema Z, Sawadogo A, Kyelem CG, et al. Hepatocellular carcinoma in the African environment of Burkina Faso: contribution of ultrasound in 58 The Pan African Medical Journal. 2010; 10.
- Camengo Police SM, Koffi B, Boua-Akelelo NP, et Complications of cirrhosis at the Amitié University Hospital in Bangui. Médecine d'Afrique Noire. 2014; 61: 537-542.
- https://www.has-sante.fr/upload/docs/application/pdf/diagnostic_cirrhose_-_recommandations.pdf
- Camengo Police SM, Service G, Boua-Akelelo NP, et The Epidemiological, Clinical, Biological and Morphological Characteristics of Primitive Liver Cancers in Bangui. Open Journal of Gastroenterology. 2020; 10: 97-105.
- Stroffolini Etiological factor of hepatocellular carcinoma in Italy. Minerva Gastroenterol Dietol. 2005; 51: 1-5.
- Bahaa Eldeen Senousy Ismail, Roniel Cabrera. Management of liver cirrhosis in patients with hepatocellular carcinoma. Chin Clin Oncol. 2013; 2: 1-19.
- Sangiovanni A, Del Ninno E, Fasani P, et Increased survival of cirrhotic patients with a hepatocellular carcinoma detected during surveillance. Gastroenterology. 2004; 126: 1005-1014.
- Mwamba-Kalambayi P, Etienne A, Chirpaz E, et Comparative study of the frequency of hepatitis b and c in people newly diagnosed with hepatocellular carcinoma in metropolitan France and overseas departments and regions, 2015-2019. BEH. 2022; 3: 85-94.
- Sehonou J, Kodjoh N, Sake K, et Liver cirrhosis in Cotonou, Republic of Benin: clinical aspects and factors related to death. Med Trop. 2010; 70: 375-378.
- Kpossou AR, Gnangnon FHR, Seidou F, et Epidemiological, clinical, paraclinical and therapeutic aspects of hepatocellular carcinoma in Cotonou. Med Afr Noire. 2020; 6710: 537-545
- Fatima Pratic, Houda Ouarrach, Zouhour Samlani-Sebbane, et al. Hepatocellular carcinoma: epidemiological, clinical and therapeutic profile at Marrakech University Hospital (about 76 cases). Hegel. 2017; 7: 195-200.
- Bossali F, Koumou Okandze L, Katende S, et Seroprevalence of hepatitis B in patients with cirrhosis and patients with hepatocellular carcinoma in Pointe-Noire from 2005 to 2008. J Afr Hépatol Gastroentérol. 2011; 5: 2-5.
- Kumar M, Kumar R, Syed S Hissar, et Risk factors analysis for hepatocellular carcinoma in patients with and without cirrhosis: a case-control study of 213 hepatocellular carcinoma patients from India. J Gastroenterol Hepatol. 2007; 22: 1104-1111.
- Zombre NMS, Coulibaly A, Somda SK, et Primary liver cancers in B viral cirrhosis at the Centre Hospitalier Universitaire Yalgado Ouedraogo Ouagadougou (CHUYO): epidemiological, diagnostic and evolutionary aspects. Annale de l'Université Joseph KI-ZERBO Série D. 2019; 023: 243-253.
- Bosch FX, Ribes J, Borras J. Epidemiology of primary liver Semin Liver Dis. 1999; 19: 271-85.
- Some EN, Some OR, Somda S, et Primary liver cancer in Ouagadougou, Burkina Faso: is the hepatitis B virus still the main player? Sciences et techniques. Sciences de la santé. 2019; 42: 33-42.