Impact of Clinicoepimiological Characteristics on the Outcome of Neo Adjuvant Concurrent Chemo Radiation in Locally Advanced Rectal Cancer Patients
Author'(s):Wafaa A. Elnemrawy1*, Hany M. Abd Elaziz2, Ramy R. Ghali2 and Nesreen A. Mosalam2
1Nasser Institute for Treatment and Research, Egypt.
2Faculty of Medicine, Ain Shams University, Egypt.
*Correspondence:
Wafaa A. Elnemrawy, Clinical Oncologist in Nasser Institute for Treatment and Research, Egypt, Tel: 01093811030.
Received: 08 January 2019; Accepted: 21 January 2019
Citation: Wafaa A. Elnemrawy, Hany M. Abd Elaziz, Ramy R. Ghali, et al. Impact of Clinicoepimiological Characteristics on the Outcome of Neo Adjuvant Concurrent Chemo Radiation in Locally Advanced Rectal Cancer Patients. Cancer Sci Res. 2019; 2(1); 1-9.
Abstract
Background: The treatment of locally advanced rectal cancer (LARC) is subject to continuous change due to better diagnostic tools, radio therapeutic techniques and chemotherapeutic agents. Careful consideration of primary tumor, regional lymph node and distance metastasis will improve the survival of rectal cancer with the selection of proper therapy. Widespread use of neoadjuvant therapy has all contributed to decrease the rate of local recurrence, raise the quality of life and the probability of overall survival.
Aim of the Work: to correlate clinico-epdemiological factors of LARC patients receiving neoadjuvant concurrent chemo radiotherapy (NACRT) with disease -free survival (DFS) and overall survival (OS).
Patients and Methods: In this retrospective study, data collected from files of 100 patients with LARC assessed using colonoscopy, enhanced computed tomography, and or magnetic resonance imaging, between Jan 2010 and December 2016 in oncology department of Ain Shams faculty of medicine and Nasser institute of treatment and research. The patients received long course radiotherapy (45-50.4 Gy/1.8-2 Gy) combined with concurrent chemotherapy. Surgery was done after NACRT, which had been abdominoperineal resection (APR), low anterior
resection (LAR), exploration. Data collected retrospectively by reviewing of medical records (hard copy records, pre-treatment radiology, radiotherapy documentation, surgical and pathology reports, and follow up clinic records). Ethics committee of Ain Shams faculty of medicine approved the study.
Results: This study showed younger age presentation of our population with median age 44yr. Median of locoregional recurrence free survival of the study group is18ms with 95 %CI. Median of distant metastasis free survival of the study group is 15ms ± 3.45 with 95% CI. Median DFS of study group was 12ms with 95% CI. Median overall survival of study group was 48ms with 95% CI while 5-year OS not reached. The study showed that grades of rectal cancer having statistically difference with DFS and OS with P value 0.009 and hazard ratio 1.919 with 95% CI. Types of surgery (LAR, APR and exploration) had statistically significant difference and impact on DFS and OS with P value 0.044 and hazard ratio 1.646 with 95% CI. y-pathological nodal staging had statistically significant difference on DFS and OS with P value 0.042 and hazard ratio 1.633 with 95% CI. Pathological response that achieved after CCRT having statistically significant difference on DFS and OS with P value 0.048 and hazard ratio 1.323 with 95%CI.
Conclusion: Assessment of LARC patients before selection type of therapy is very critical to select whom patient will gain functional preservation at the time of surgery and increase probability of overall survival. The study showed younger age presentation of our population with median age 44yr that may refers indirectly to more clinico-epidemiological difference than other population. Therefore, it is critical to undergo further studies in these specific age groups.
Keywords
Introduction
Colorectal cancer is the fourth most frequently diagnosed cancer and the second leading cause of cancer death in the United States [1].
It accounts for over 9% of all cancer incidence and accounts for about 8.5% of all cancer related mortality [2]. Despite the observed improvements in the overall colorectal cancer incidence rate, a retrospective cohort study of the Surveillance, Epidemiology, and End Results (SEER) CRC registry found that the incidence of colorectal cancer in patients younger than 50 years has been increasing. The authors estimate that the rectal cancers will increase by 124.2% for patients 20 to 34 years by 2030. The cause of this trend is unknown [1].
According to the results of the National Population-Based Registry Program of Egypt 2008-2011, these data showed that ASR of 6 and 4.9 per 100, 000 in men and women respectively. The incidence represents 3.2% of all cancers in both sexes. 1070rectal cancer cases suspected within 2020 (568 males and 505 females with male to female ratio (1.1:1) [3].
Locally advanced rectal cancer (LARC) has often developed postoperative local recurrence. Widespread use of neoadjuvant therapy has all contributed to decrease the rate of local recurrence, raise the quality of life and the probability of overall survival [4].
In an effort to reduce further the incidence of margin positivity, local recurrence and improve survival of rectal cancer, preoperative neoadjuvant radiotherapy with or without chemotherapy has been introduced as adjuvant to total mesorectal excision (TME). A number of trials have reported reduced local recurrence rates and a potential survival advantage associated with preoperative radiotherapy [5].
It also needs to judge and consider the balance between the higher recurrence rate and the higher sphincter-preserving rate. In addition, the evaluation of the efficacy of neoadjuvant radio chemotherapy should be as enough as possible. It needs to maximally improve the accuracy of evaluation [6].
Long-course chemo radiotherapy, in contrast to short course, is associated with a significant tumor response and down staging in high risk rectal cancer patients while short course is reserved to intermediate risk ones [4].
The aim of the work
This is a retrospective study aiming to correlate clinico- epdemiological factors of LARC patients with outcomes of (NACRT) regarding disease -free survival (DFS) and overall survival (OS).
Patients and methods
Retrospective study designed to assess the outcome of (NACRT) for LARC patients, regarding clinico epidemiological factors (patients’ factors, disease factors and treatment factors) through correlation with DFS and OS.
Data collection
Data collected from files of 100 patients with stage II and III disease assessed using colonoscopy, enhanced computed tomography, and or magnetic resonance imaging, between Jan 2010 and December 2016 in oncology department of Ain Shams faculty of medicine and Nasser institute of treatment and research. The patients received long course radiotherapy (45-50.4 Gy/1.8-2 Gy) combined with concurrent chemotherapy.
Surgery was done after NACCRT which had been abdominoperineal resection (APR), low anterior resection (LAR), exploration. Data were collected retrospectively by reviewing of medical records (hard copy records, pre-treatment radiology, radiotherapy documentation, surgical and pathology reports, and follow up clinic records). Ethics committee of Ain Shams faculty of medicine approved the study.
Inclusion criteria of the treated patients
- Age is more than 18 and less than
- ECOG is less or equal to
- Rectal cancer diagnosed by lower GIT Endoscopy and
- Locally advanced rectal cancer proved by ultrasound, CT and MRI of abdomen and pelvis.
- No evidence of metastasis at time of
- Patients received neoadjvant concurrent chemoradiotherapy then underwent surgery.
Exclusion criteria of the treated patients
- Age is less than 18and more than 80
- ECOG is more than
- Evidence of metastasis at time of
- Patients previously had other malignancy expect skin
- Patients previously received chemotherapy or
Collected data cheek list form was used Data collection and analysis
The collected data had been revised, coded, tabulated and SPSS Software system (version 11.0; Chicago, IL) was used for statistical analysis. Continuous variables were presented as the median and range. The univariate analysis data were assessed using the Yates chi-square test. The Cox regression model (logistic regression analysis) was used for multivariate analysis. DFS and OS were analyzed using the log-rank test and was plotted as Kaplan–Meier curves.
Statistical analysis
Recorded data analyzed using the statistical package for social sciences, version 20.0 (SPSS Inc., Chicago, Illinois, USA). Quantitative data expressed as mean± standard deviation (SD).
Qualitative data expressed as frequency and percentage.
The following tests are done:
- Kaplan-Meier Survival Analysis: is a descriptive procedure for examining the distribution of time-to-event variables.
- Log rank test to compare time-to-event variables by levels of a factor variable.
- Cox regression model (logistic regression analysis) used for multivariate analysis.
- The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant as the following:
- Probability (P-value)
- P-value <0.05 was considered
- P-value <0.001 was considered as highly
- P-value >0.05 was considered
Results
The study shows: that study population comprised of 100patients, distributed as (52 men and 48 women) with median age, 44 years) with performance status < or equal to two. Thirteen patients (13%) achieved complete pathological response whose pathology was free tumor cells in resected primary tumor and lymph nodes.
Fifty-four patients (54%) achieved partial response while 12 patients (12%) progressed on CCRT. Fifty-nine of patients (59%) had loco-regional recurrence and Forty-one of patients (41%) had no loco-regional recurrence with median of loco-regional recurrence free survival of the study group is18ms with 95% CI. Forty-six of patients (46%) had distant metastasis and 54% of patients had no distant Metastasis with median of distant metastasis free survival of the study group is 15ms ± 3.45 with 95% CI. Median DFS of study group was 12ms with 95%CI. Median overall survival of study group was 48ms with 95% CI while 5-year OS not reached.
This study shows that there is no statistically significant difference between patient's demographic characteristics and DFS. This study also shows that disease parameters had no impact and no statistical significance on DFS except grading of the tumor as in univariate analysis. The study showed statistically significant difference between grades of the tumor with DFS as DFS in patients with grade I had not reached, while in Grade II and III, was 18 and 12ms respectively (P value<0.002).
This study shows there was no statistically difference between doses of long course radiation on DFS of the study and so type of concurrent chemotherapy on DFS while type of surgery had impact and statistically significant difference on DFS. As patients underwent LAR had median DFS 18ms versus those underwent APR or exploration (15ms and 6ms respectively with (p value<0.0016).
This study shows no statistically difference between patients with or without functional preservation after surgery on DFS, while shows highly statistically significant difference between different y pathological T staging, N staging, LVI, PNI and pathological response with DFS. As DFS of patients with pathologically T0 staging was not reached while in those with positive T staging, was 12ms regarding the end of study with (p value <0.00042). DFS was also not reached in patients with pathologically N- had while it was 12ms in those with N+ with (p value <0.0001) and so patients with negative LVI, PNI had median DFS 27ms versus 12ms in those with positive LVI, PNI with (p value <0.024).
DFS was also not reached in Patients with complete pathological response versus other groups with (p value <0.001).
The study showed that there is no statistically significant between patient's demographic characteristics and overall survival. And so that disease parameters had no impact and no statistical significance on overall survival except grading of the tumor as in univariate analysis, the study showed statistically significant difference between grades of the tumor and overall survival as grade I had median survival 45ms versus 36ms, 24ms of Grade II and III respectively with (P value< 0.003). Even after multivariate analysis, it remained significant with (P value< 0.009).
Type of surgery had impact and statistically significant difference on overall survival. As patients underwent LAR had median survival 48ms versus those underwent APR or exploration (36ms and 12ms respectively with (p value <0.001). In multivariate analysis, type of surgery is independent prognostic factor that should strongly considered in treatment these patients. The study also showed significant statistically difference between different y pathological T staging, N staging, LVI, PNI and pathological response with overall survival. As patients with pathologically T0 staging had median survival 48ms versus 6ms in those with T4 with (p value <0.001).
As patients with pathologically N0 had median survival 33.6ms versus 16.5 in those with N2 with (p value <0.001) and so patients with negative LVI, PNI had median overall survival 36ms versus 24ms in those with positive LVI, PNI with (p value <0.024). Patients with complete pathological response, had highest median overall survival versus other groups with (p value <0.001).
Multivariate analysis of the study showed that grades of rectal cancer having statistically difference with overall survival with P value 0.009 and hazard ratio 1.919 with 95% CI. Types of surgery (LAR, APR and exploration) had statistically significant difference and impact on overall survival with (P value 0.044) and hazard ratio 1.646 with 95% CI. y pathological nodal staging had statistically significant difference on overall survival with (P value 0.042) and hazard ratio 1.633 with 95% CI. Pathological response that achieved after CCRT had statistically significant difference on overall survival with (P value 0.048) and hazard ratio 1.323 with 95%CI.
These parameters are independent prognostic factors and considered during management of patients with locally advanced rectal cancer.
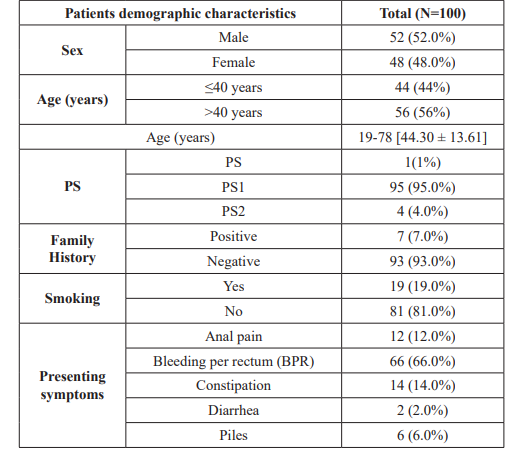
Table 1: Patients demographic characteristics distribution of the study group.
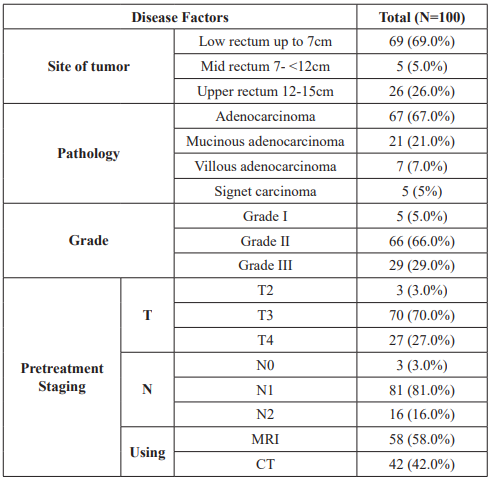
Table 2: Disease factors distribution of the study group.
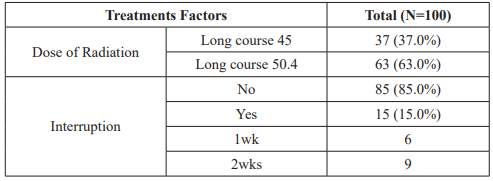
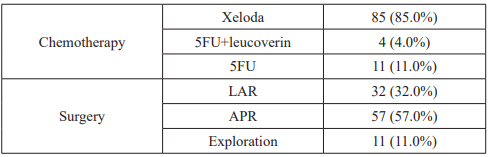
Table 3: Treatments factors distribution of the study group.
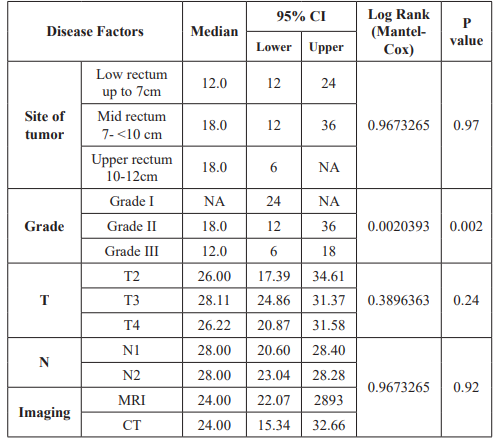
Table 4: Relation between disease factors and DFS.
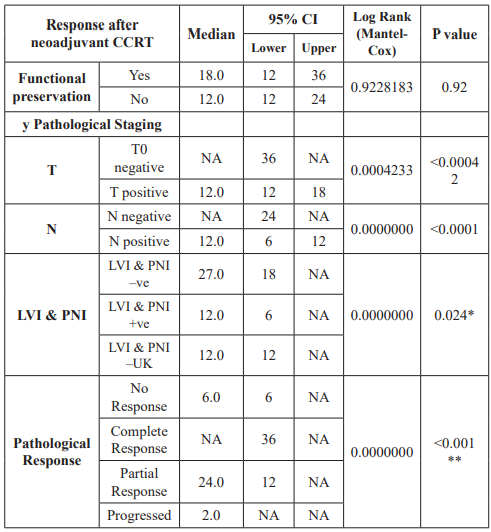
Table 5: Relation between DFS and responses after neoadjuvant CCRT.
This table shows no statistically difference between patients with or without functional preservation after surgery on DFS, while shows significant statistically difference between different y pathological T staging, N staging, LVI, PNI and pathological response with DFS. As DFS of patients with pathologically T0 staging was not reached while in those with positive T staging, was 12ms regarding the end of study with (p value <0.00042). DFS was also not reached in patients with pathologically N- had while it was 12ms in those with N+ with (p value <0.0001) and so patients with negative LVI, PNI had median DFS 27ms versus 12ms in those with positive LVI, PNI with (p value <0.024). DFS was also not reached in Patients with complete pathological response versus other groups with (p value <0.001).
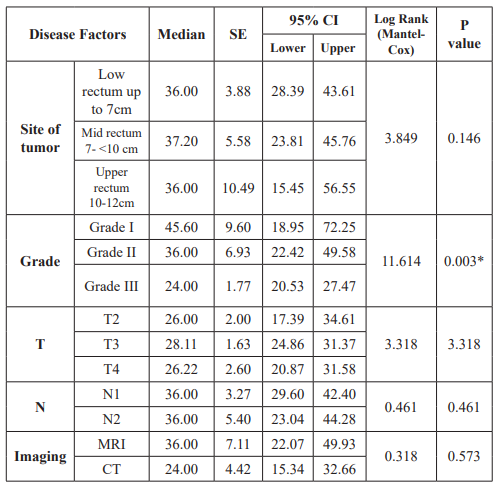
Table 6: Shows relation between disease factors and overall survival.
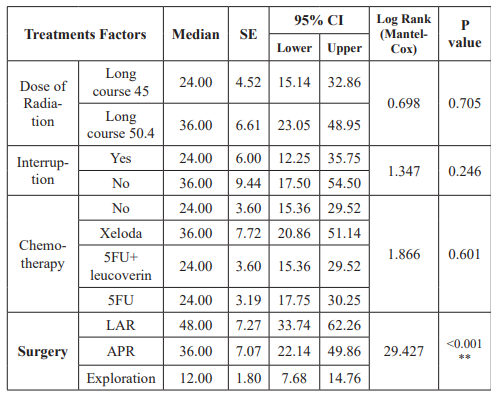
Table 7: shows relation between treatment factors and overall survival.
This table shows there was no statistically difference between doses of long course radiation on overall survival of the study and so type of concurrent chemotherapy on overall survival while type of surgery had impact and statistically significant difference on overall survival. As patients underwent LAR had median survival 48ms versus those underwent APR or exploration (36ms and 12ms respectively with (p value <0.001). type of surgery is independent prognostic factor that should be considered in treatment these patients.
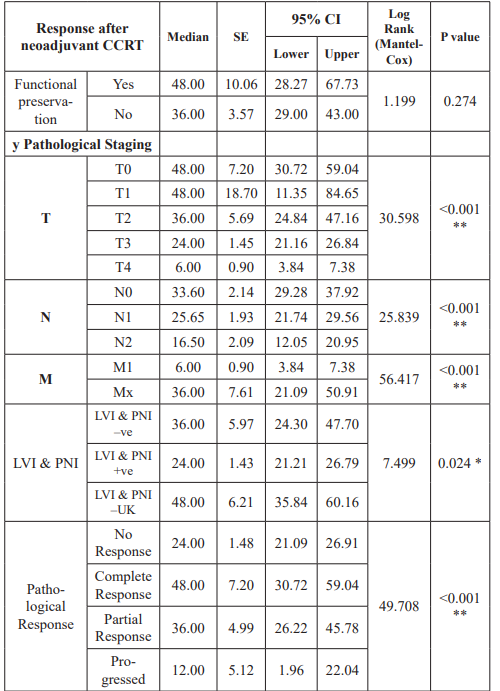
Table 8: Relation between overall survival and responses after neoadjuvant CCRT.
This table shows no statistically difference between patients with or without functional preservation after surgery on overall survival, while shows significant statistically difference between different y pathological T staging, N staging, LVI, PNI and pathological response with overall survival. As patients with pathologically T0 staging had median survival 48ms versus 6ms in those with T4 with (p value <0.001). As patients with pathologically N0 had median survival 33.6ms versus 16.5 in those with N2 with (p value <0.001) and so patients with negative LVI, PNI had median overall survival 36ms versus 24ms in those with positive LVI, PNI with (p value<0.024). Patients with complete pathological response, had highest median overall survival versus other groups with (p value <0.001).
as Zhao et al, evaluated 100 patients of rectal cancer receiving neoadjuvant chemoradiotherapy then curative surgery at
Liaoning Cancer Hospital and Institute. (70%male-and 30% female). The median age was 60.5 (26–81 years) [9]. Both studies showed no statistically significant difference between patient’s parameters (age, sex,) with overall survival and DFS.
The median age in our study was younger than the previous studies. This may be due to unique features of the pathogenesis of colorectal cancer in Egypt as evidenced from the epidemiologic studies where the percentage of colorectal cancer became high in patients less 40yrs [10].
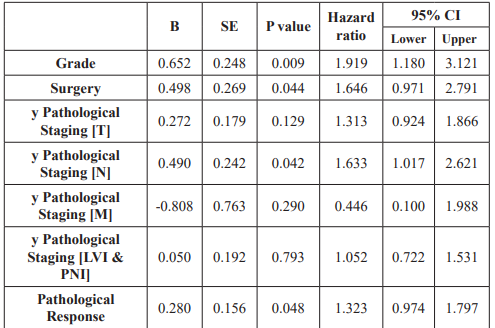
Table 9: Multivariate analysis of independent predictors through overall survival in all patients.
This table shows the parameters that had statistically significant difference with overall survival in the study. Multivariate analysis of the study showed that grades of rectal cancer having statistically difference with overall survival with P value 0.009 and hazard ratio 1.919 with 95% CI. Types of surgery (LAR, APR and exploration) had statistically significant difference and impact on overall survival with P value 0.044 and hazard ratio 1.646 with 95% CI. y pathological nodal staging had statistically significant difference on overall survival with P value 0.042 and hazard ratio 1.633 with 95% CI. Pathological response that achieved after CCRT had statistically significant difference on overall survival with P value 0.048 and hazard ratio 1.323 with 955 CI. These parameters are independent prognostic factors and considered during management of patients with locally advanced rectal cancer.
Discussion
Colorectal cancer accounts for over 9% of all cancer incidence and accounts for about 8.5% of all cancer related mortality [1].
Prognostic models play important role in 21st century medicine for knowing which factors predict outcomes, clinicians gain insight into the biology and natural history of the disease. Treatment strategies may be optimized based on the outcome risks of the individual patient [7].
Population of this Study were distributed as (52 % men and 48% women) with median age, 44 years). Performance status was(1) in 95% of patients. While in Lee et al. [8] study that include 123 Chinese patients distributed according to sex :77.2% male and 22.8% female with median age 57yr (range 27 to 79yr) with 79.7%of patients with performance status one.
Both studies are in line, as both showed no statistically differences between previous patients’ parameters with overall survival and DFS.
This study also showed disagreement with Zhao et al. [9] study regarding distribution of (age and sex) among study population.
This study is in line with Twu C and his colleagues [11] study that conducted 46 patients with locally advanced rectal cancer who received CCRT distributed as male (51.2%) and female (48.7%) with median age 55+/- 13yr. Both studies showed no statistically significant difference between patient’s parameters (age, sex,) with overall survival and DFS.
This study showed predominance of low rectal tumor represented (69%) of patients while med and high were 5%and 26% respectively among study population while Lee et al, [8] showed predominance of med rectal cancer (68%).
This difference in site of tumor as Lee et al. [8] divided tumor as low (0 to </= 5), med (>5 to 10) and high (>10). While in this study, we considered rectal cancer as low (up to 7cm from anal verge), med (>7 to 12cm from anal verge) and high (>12 to 15cm from anal verge) according to anatomical classification of rectum by Nougaret S, et al. (12). but both studies are in line as both showed no statistically difference between site of the tumor with overall survival and DFS.
This study is not in line with Sauer et al. [13] study, in preoperative chemo radiotherapy arm that included 404 patients. According to site of tumor, low, med and high rectal tumors represented 29%, 47% and 21%of patients. Sauer et al, study showed predominance of med rectal cancer (47%) that is different from our study result that documented high percent of low rectal cancer (69%) as they depended on different classification of rectal cancer. Both studies are in line, as both showed no statistically difference between site of the tumor with overall survival and DFS.
This study is in line with Ge´rard et al. [14] study that conducted on 598 patients through 56 institutions in arm that received capcitabine. As Ge´rard et al. divided patients regarding site of tumor, to lower rectal cancer 69.6% (up to 6cm from anal verge) and upper rectal cancer 30.4% (>6cm from anal verge). Both studies are in line, as both showed no statistically difference between site of the tumor and overall survival.
This study showed predominance moderate differentiated adenocarcinoma (67%) and statistically difference with overall survival with (P value< 0.003) that showed agreement with Lee et al. [8] study that showed impact of grade on overall survival in multivariate analysis with (P value< 0.014).
This study also documented statistically significance between grades of tumor with DFS that showed disagreement Lee et al. [8] study that showed no impact of grade on DFS.
This study is in line with Kuan et al. [15] study that predominance of moderate differentiated tumor (Grade 2) 60% and showed impact of grade on overall survival in multivariate analysis with (P value< 0.001) [15].
This study is in line with Ge´rard et al. [14] study that predominance of moderate differentiated tumor (Grade 2) 51.2%, Both studies are not in line as Ge´rard et al, study showed no statistically significant difference regarding histological grade on overall survival and DFS. This difference may be due to small sample size(100) compared to large sample size (598) of Ge´rard et al. [14].
This study showed patients distributed regarding pre-operative staging as T3 (70%) and T4 (27%) while nodal involvement (97%) and N0 (3%).
This study is slightly dissimilar to Lee, et al. [8] study showed patients distributed according to preoperative staging of primary tumor and nodal involvement: T3 and T4 represented as 86.2%, and 13.8% respectively while nodal involvement as N-ve (28.5%) and N+ve (71.5%).
This difference was as most patients included in this study, presented with bulky tumor and stage III, while Lee et al. [8] study population were stage II and III.
Both studies showed no statistically significant differences between preoperative staging (TN) with overall survival and DFS.
This study is in line with Ge´rard et al. [14] study showed preoperative staging of primary tumor and nodal involvement: T2 and (T3and T4) represented as 7.9%, 92.1% respectively while nodal involvement as N-ve (29.3%) and N+ve(70.7%) [14].
This study is in line with Ge´rard et al. [14] as showed no statistically significant differences between preoperative staging (T N) with overall survival.
This study is in line Belluco et al. [16] study that Showed no statistically significant differences between pretreatment staging (N) with 5yr OS and DFS. This study showed no statistically significant between treatment factors (dose of radiotherapy and type of chemotherapy) with overall survival and DFS.
This study is similar with Lee et al. [8] study results. This study is in line with Sineshaw et al. [17] study that showed that no statistically significant between radiotherapy doses on OS and DFS among locally advanced patients and so type of concurrent chemotherapy (5FU versus capcitabine).
This study is in line with Ngan et al. [18]. Showed that no statistically significant between radiotherapy doses on OS and DFS among locally advanced patients. This study is similar to Bujko et al. [19]. study that showed that no statistically significant differences between radiotherapy doses of long course radiotherapy on OS and DFS among locally advanced patients and so type of concurrent chemotherapy.
This study showed that 89% of patients underwent TME (LAR 32% and APR 57%) and 11% of patients underwent exploration. This study showed better OS and DFS in patients underwent TME with longer median OS and DFS in LAR than in APR and exploration with (P value 0.044) in multivariate analysis.
This study is in line with Lee et al. [8]. that showed 93% of patients underwent TME (LAR 70.9% and APR 22.7%) while 5.6% of patients were inoperable at time of surgery. Lee et al. study showed better OS and DFS in patients underwent TME especially with LAR.
This study is in line with Valentini et al. [20] study that showed all patients underwent TME (LAR 57% and APR 38%) and statistically significant difference regarding type of surgery with DFS and overall survival with (p value <0.001). This study showed disagreement with Belluco et al. [16] study that documented 80% of patients underwent total mesorectal excision (LAR 79.3% and APR 20.6%) and 20% underwent fullthickness local excision (LE) and showed no statistically differences between type of surgery on DFS and overall survival.
Predominance of APR in our study more than previous studies as sphincter-preserving surgery is difficult and depends on multiple factors (age, co morbidities, tumor bulkiness and surgical expertise).
This study showed that LVI and so PNI were positive in 20% of patients and negative in 27% of patients and were unknown in 53% of patients. This study showed that PNI and LVI had statistically significance on DFS but no impact on OS in multivariate analysis This study is not in line Zhao et al. [9] study regarding percentage of LVI and PNI among patients Zhao et al. showed LVI and so PNI were positive in 14% of patients and negative in 86% of patients.
This difference was present because LVI and PNI were unknown in 53% of study population, but regarding positive patients of our study; its percentage is not extremely far from the result of the Zhao et al. [9]. This study is in line with Zhao et al. [9] study, showed that PNI and LVI had impact on DFS while there is no statistically significance on OS in multivariate analysis.
This study showed 13% of patients achieved cPR and 54% achieved partial response. This study showed that pathological response (P value 0.048) had impact and statistically significant difference on DFS and OS in multivariate analysis.
This study showed agreement with Lee et al. [8] study that showed cPR and partial response occurred in 10.5% and 51% of patients respectively, Lee et al. showed statistically significant difference regarding pathological response with DFS but no impact on OS.
This study is in line with Kuan et al. [15] study that showed cPR occurred in 13.6% and showed statistically significant difference regarding pathological response with overall survival with (p value 0.001).
This study is in line with Juan Ren, et al. [21] study that was a review of Neoadjuvant Chemo radiotherapy for LARC patients and Showed statistically significant difference between pathological response on overall survival and DFS and percent of cPR was 11:16% in different included studies in review as (Sweden Brandengen (2008) with cPR 16% (P value .04), FFCD9203 (2006) with cPR 11.4% (p value 0.001).
This study showed agreement with Belluco et al. [16] as showed statistically significant difference between pathological response on DFS and OS with (p value 0.011). However, in our study percent of patients that achieved cPR was 13% that was less than in Belluco et al. (20%) may be due to small sample size compared to large sample of Belluco et al. [16].
This study is in line with Martin and Winter [22] study: meta- analysis of outcomes to neoadjuvant chemoradiotherapy for rectal cancer and showed statistically significant difference between pathological response on DFS and OS. Percent of cPR was 10:50% in different included studies in review as (Avallone et al., (2011) with cPR 38 %, Kim et al, (2011) with cPR 13.8 % and Valentini et al., (2008) with cPR 10.3%).
This study is in line with Ge´rard et al. [14] study showed 13.9% of patients achieved cPR and statistically significant difference regarding pathological response with overall survival.
This study showed agreement with Sua´rez et al. [23] study that documented complete pathological response was observed in (14.2%) patients and poor response was in 85% of patients and showed that pathological response (P value 0.048) had impact and statistically significant difference on DFS in univariate analysis and OS in multivariate analysis.
This study showed 13% of patients achieved pathological T0 and 87% of patients with malignant cells in their 1ry tumor pathology and statistically difference between pathological T staging with DFS and no impact on OS in multivariate analysis.
This study showed agreement with Lee et al. [8] that showed statistically significance of pathological T0 on DFS in univariate analysis and no impact on OS in multivariate analysis. This study is in line with Wolthuis A, et al. [24] study showed 22% of patients achieved pathological T0 and no statistically difference regarding pathological T staging with overall survival. Small percent in our study is due to small sample size (100 patients) compared to large size (356 patients) of Wolthuis A, et al.
This study is in line with Ge´rard et al. [14] study showed 14.2% of patients achieved pathological T0 and no statistically difference regarding pathological T staging with overall survival. This study showed 44% of patients achieved y pathological N0 and statistically significant difference regarding y pathological N staging with overall survival in univariate analysis with (p value 0.001) and remain significant after multivariate analysis with (p value 0.042).
This study showed agreement with Lee et al. [8] study showed statistically significant regarding pathological y N with DFS in univariate analysis and OS with (p value .018) in multivariate analysis.
This study show agreement with Belluco et al. [17]. Study Showed statistically significant difference between pathological N staging with DFS and OS. In our study, y pathological TN showed statistically significant difference with overall survival in univariate analysis, however multivariate analysis showed that pathological N staging remains significant, is independent prognostic factor, and is in line with Belluco et al. [17].
Conclusion
In conclusion well assessment of LARC patients before selection type of therapy is very important to select whom patient will benefit from NACRT, will gain functional preservation at the time of surgery and increase probability of overall survival. The study showed younger age presentation of our population with median age 44yr that may refers indirectly to more clinico-epidemiological difference than other population. Therefore, it is critical to undergo further studies in these specific age groups.
References
- Siegel R, Ma J, Zou Z, et Cancer statistics 2014. CA Cancer J Clin. 2018; 64: 9-29.
- Tabaries S, QuelletV, HsuB, et al. granulocyte immune infilteration are essential for efficient formation of breast and colorectal cancer. Breast cancer Res. 2015; 17: 45.
- Amal S, Hussein M, Nabiel N, et al. Cancer Incidence in Egypt: Results of the National Population-Based Cancer Registry Journal of Cancer Epidemiology. 2014; 18.
- Joshua S, Julio Advances and Challenges in Treatment of Locally Advanced Rectal Cancer. J Clin Oncol. 2015; 33: 1797-1808.
- Belluco C, Paoli A, Canzonieri V, et Long-Term Outcome of Patients with Complete Pathologic Response after Neoadjuvant Chemoradiation for cT3 Rectal Cancer: Ann Surg Oncol. 2011; 18: 3686-3693.
- Benson A, Venook A, Bekaii-Saab T, et al. NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2015; 13: 719-728.
- Edge, SB, Byrd, DR, Compton CC, et al. AJCC (American Joint Committee on Cancer). Cancer Staging Manual, 8th edition. CA Cancer J Clin. 2017; 67: 93-99.
- Lee S, Chi Leung Chiang Francis Ann, Shing Lee, et al. Outcome of neoadjuvant chemoradiation in MRI staged locally advanced rectal cancer: Retrospective analysis of 123 Chinese patients. J Formos Med Assoc. 2018; 117: 825-832.
- Zhao J, Jian Xu, Rui Zhang. Clinical and Prognostic Significance of Pathological and Inflammatory Markers in Mucinous Rectal Cancer Patients Receiving Neoadjuvant Chemoradiotherapy and Curative Surgery. Med Sci Monit. 2017; 23: 4826-4833.
- Andrew R, Hongmei N. Epidemiology of colorectal cancer. Int J Mol Epidemiol Genet. 2016; 7: 105-114.
- Twu C, Wang H, Chen J, et al. Neoadjuvant ConcurrentChemoradiotherapy in Treating Locally Advanced Rectal Cancer. J Chin Med Assoc. 2009; 72: 179-182.
- Nougaret S, Rouanet P, Bibeau F, et The use of MR imaging in treatment planning for patients with rectal carcinoma: have you checked the “DISTANCE”? Radiology. 2013; 268: 330-344.
- Sauer R, Susanne Merkel, Rainer Fietkau, et al. Comparison of Two Neoadjuvant Chemoradiotherapy Regimens for Locally Advanced Rectal Cancer: Results of the Phase III Trial ACCORD 12/0405-Prodige 2. American Society of Clinical Oncology. 2010; 28: 1638-1644.
- Kuan F, Hsuan Lai C, Ying Ku H, et al. The survival impact of delayed surgery and adjuvant chemotherapy on stage II/ III rectal cancer with pathological complete response after neoadjuvant chemoradiation. Int J Cancer. 2017; 140: 1662-1669.
- Belluco C, Forlin M, Olivieri M, et Long-term outcome of rectal cancer with clinically (EUS/MRI) metastatic mesorectal lymph nodes treated by neoadjuvant chemoradiation: role of organ preservation strategies in relation to pathologic response. Annals of surgical oncology. 2016; 23: 4302-4309.
- Sineshaw M, Jemal A, Charles R, et Changes in Treatment Patterns for Patients With Locally Advanced Rectal Cancer inbthe United States Over the Past Decade: An Analysis From the National Cancer Data Base. Cancer. 2016; 122; 1996-2003.
- Ngan S, Burmeister B, Goldstein D, et Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group Trial 01.04. Journal of Clinical Oncology. 2012; 30: 3827-3833.
- Bujko K, Nowacki M, Michalski W, et al. Long-term results of a randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Br J Surg. 2012; 93: 1215-
- Valentini V, van Stiphout R, Lammering G, et Nomograms for predicting local recurrence, distant metastases, and overall survival for patients with locally advanced rectal cáncer on the basis of European randomized clinical triáis. J Clin Oncol. 2011; 29: 3163-3172.
- Juan Ren, Yi Li, Ji Wang, et al. A Review of Neoadjuvant Chemoradiotherapy for Locally Advanced Rectal Int.
- Biol. Sci. 2016; 12: 1022-1031.
- Martin S, Winter Systematic review and meta-analysis of outcomes following pathological complete response to neoadjuvant chemoradiotherapy for rectal cancer. Br J Surg. 2012; 99: 918-928.
- Sua ´rez J, Vera R, Bale EM, et al. Pathologic response assessed by Mandard grade is a better prognostic factor than down staging for disease-free survival after preoperative radiochemotherapy for advanced rectal cancer. Colorectal Disease. 2008; 10: 563-568.
- Wolthuis AM, Penninckx F, Haustermans K, et al. Outcome standards for an organ preservation strategy in stage II and III rectal adenocarcinoma after neoadjuvant chemoradiation. Annals of surgical oncology. 2011; 18: 684-690.