Implantable Venous Access System: Percutaneous approach at the Teaching Hospital of Point “G” in Bamako, Mali
Author(s): Togola Birama1,2*, Bengaly Bréhima2, Touré Cheick Ahmed Sekou2, Ouattara Drissa2, Ly Madani3, Coulibaly Bréhima1,2, Coulibaly Mahamadou2, Traoré Drissa1,2, Sanogo Souleymane2, S Diallo Siaka2, Ongoïba Nouhoun1,2
1Faculty of Medicine and Odonto-Stomatology of Bamako (FMOS).
2Surgery Department “B” in Point “G” Teaching Hospital of Bamako.
3Medical Hematology and Oncology Department in Point “G” Teaching Hospital of Bamako.
*Correspondence:
Dr. Birama Togola, Surgery Department “B” in Point “G” Teaching Hospital of Bamako. BP: 333, Tel (00223) 66782550, Mali.
Received: 27 May 2020; Accepted: 11 June 2020
Citation: Togola Birama, Bengaly Bréhima, Touré Cheick Ahmed Sekou, et al. Implantable Venous Access System: Percutaneous approach at the Teaching Hospital of Point “G” in Bamako, Mali. Cardiol Vasc Res. 2020; 4(2): 1-5.
Abstract
Purpose: The aim of this study was to evaluate indications, feasibility and complications of percutaneous approach for positioning implantable venous access system in the department of surgery “B”.
Materials and Methods: The files of all patients who have profited from an implantable catheter chamber for 3 years from 2013 to 2016 were re-examined and analyzed retrospectively. A clinical exam and a preoperative evaluation were systematically performed.
Results: During this period 45 patients profited for positioning implantable venous access system. They were 23 women and 22 men for mean age of 53.0 ± 16.2 years. The implantation was performed specially by percutaneous approach or surgical approach in failure. The main indications were for chemotherapy in cancer for 39 (86.7%) patients, a parenteral nutrition and central venous access for perfusion respectively for 3 (6.6%) patients. We used primarily percutaneous approach by puncture of the internal jugular vein for 39 cases (86.7%) and a surgical cephalic dissection for 6 patients (13.3%). All procedures were performed on right. The operational incidents were related to the difficulty of puncture for 7 patients (15.5%), of progression of the wire for 6 (13.3%) and carotid arterial puncture for 1 (2.2%) patients. We observed one case of failure of implantation. A chest X-ray was systematic after device installation. The evolution was favorable for all patients. For the medium and longterm outcomes, we observed 4 cases (8.8%) of infection including 2 local infection and 2 malignant hyperthermia considered as a septicemia. All procedures were performed in operating room and outpatient.
Conclusion: Implantable venous access system is important for management of oncology patients. The percutaneous approach is an alternative as elegant, fast and safe as the surgical access.
Keywords
Introduction
Percutaneous implantable chambers (CIP) or Port-A-Cath (PAC) or implantable catheter chambers (CCI) are long-term intravenous devices that have first appeared since 1980s [1]. Essential instrument for chemotherapy products, they are also useful for parenteral nutrition, long-term antibiotic therapy and even for transfusion of blood products. The installation of PortA-Cath (PAC) is an essential moment for the management of cancer combining worry, hope and comfort for the patient. This activity is regulated in Europe particularly in France by specific recommendations [2-4]. Several approaches are recommended but none has demonstrated its superiority [3,5]. Since 2009 in Mali, chemotherapy is free thanks to government efforts for population health improvement. Therefore, the placement of Port-A-Cath become a surgical activity contributing for quality of cancer care. The aim of our work was to evaluate the practice of placing implantable catheter chambers in terms of indications, percutaneous approach and its complications in the surgery department “B” of Teaching Hospital Point “G” in Bamako.
Materials and Methods
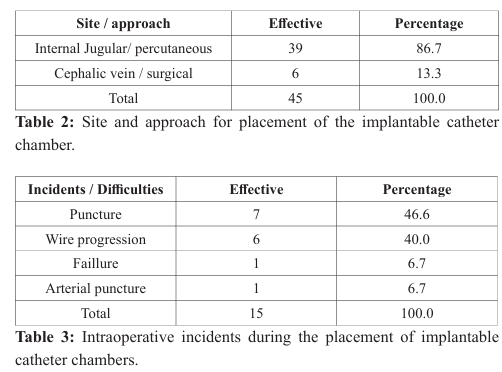
We conducted a descriptive and retrospective study over a period of 3 years from 2013 to 2016 in the department of surgery “B”. The files of patients who benefited from implantable implant were reviewed and analyzed. A consultation before the installation was systematically to choose the site, stop any anticoagulant treatment and to give explanations on the procedure. A standard preoperative hemostasis or biological assessment was performed. We operated in the operating room equipped with an image intensifier “Brilliance” and an outpatient room. All procedures were performed under local anesthesia by the same surgeon. Antibiotic prophylaxis was systematic. The device was rinsed with heparinized serum (Figure 1). The percutaneous approach by puncture of the internal jugular vein or the confluence vein was the first choice (Figures 2, 3, 4). If this approach was failed, a dissection of the cephalic vein was performed. Achieving good venous reflux and easy injection of heparinized serum through the chamber were considered for success. A chest X-ray was systematic after device installation (Figure 5). Data analysis was performed with Epi Info 2008 software version 3.5.1.

Results
During this period, 45 patients benefited from the placement of an implantable catheter chamber. There were 23 women for 22 men with a mean age of 53.0 ± 16.2 years with extremes of 28 years and 80 years. The main indications were anti-cancer chemotherapy for 86.7% patients, parenteral nutrition or a central venous access for infusion in respectively 6.6% of patients (Table 1).
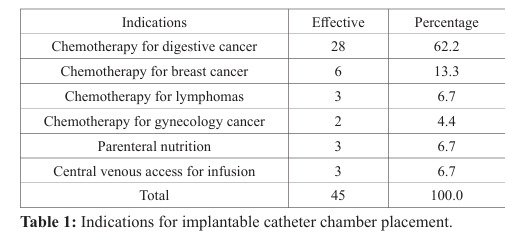
All procedures were performed on the right. The percutaneous approach was performed by puncture of the internal jugular vein in 86.7% and a surgical approach by dissection of cephalic vein in 13.3% (Table 2). The intraoperative incidents observed were difficulty of puncture in 7 patient (15.5%), a difficulty of progression of the guide wire 6 patients (13.3%) and an accidental carotid arterial puncture for 1 patient (2.2%) (Table 3). The mean time for surgery was 54.9 min ± 12.7 min. We implanted a size 7F in 12 patients and 9 F for 28 patients. We observed a case of installation failure. Immediate postoperative course was favorable in all patients. In medium and long- term outcome (8 and 14 month), we observed 4 cases (08.8%) of infection, respectively 2 cases of local infection following a skin necrosis by subcutaneous extravasation of the chemotherapy drugs and 2 cases of unexplained malignant hyperthermia in a resuscitation patient and a patient with stomach cancer.
Discussion
The start of anti-cancer chemotherapy is an important moment for the patient. It requires an effective and practical venous approach. Thus to preserve the peripheral venous capital and improve patient comfort, the implantable catheter chambers (ICC) by accessing the central venous system appeared in 1982 in France for the long-term treatment of neoplastic conditions. Except this main indication, the Port-A-Cath (PAC) can serve as a venous access for parenteral nutrition, transfusion of blood products or rehydration in patients in poor general condition. In the absence of a palliative care center we were asked a few times for the installation of implantable chambers in case of difficulty in taking a peripheral venous access.
Although not essential, some surgeons or practitioners ask perform a hemostasis assessment after an interrogation and clinical examination as well in our study. This surgical activity was generally performed under local anesthesia unless contraindicated. Installation of Port-A-Cath (PAC) was a technique practiced by different specialists (Surgeons, Anesthesiologists, Radiologists…). According to the recommendations of the High Authority of Health (HAS) of France, published in 2005, the choice of the vein to puncture was left to the surgeon provided that it emanates from the superior cave system [3]. Several approaches have been described with advantages and disadvantages without any demonstrated superiority [5]. For most authors, the easy, safe and effective surgical dissection approach with fewer contraindications is considered to be the reference [6]. Currently, percutaneous approach was an attractive and elegant alternative allowing direct access to the deep venous system of the superior vena cava. Two veins can be punctured, the internal jugular vein and the subclavian vein.
According to some authors, the data on the risks of bad catheter positioning, carotid puncture and pneumothorax during the puncture procedure are discordant [7, 8]. Lovino et al. [8] in their prospective study showed more pneumothorax after a puncture of the subclavian vein. The risk of rupture of the catheter in the costo-clavicular forceps known as the "Pinch off" associated with the risk of pneumothorax means that several authors prefer the approach of the internal jugular vein [9-11].
As practiced by Le Ray Ferrière I et al. [10] and C Peillon [11] the percutaneous puncture of the internal jugular, direct, simple, easy and fast in the hands of an experienced has our preference compared to the cephalic access. This puncture, most often performed "blind", requires a perfect knowledge of anatomical landmarks [12]. The preference for the right side is explained by anatomical reasons. It also depends on the etiologies and the availability of the image intensifier. Puncture difficulties in some obese patients with short necks as in redux can be improved by the use of portable ultrasound systems. Prospective studies have shown the advantage of echo guidance for puncture compared to the conventional technique in the placement of an implantable catheter chamber [10, 13, 14].
The absence of this device in our practice can explain the difficulties of vein puncture or arterial complication. In Europe and especially in Great Britain, echo guidance is compulsory during catheterization of the internal jugular vein [15]. The difficulty in advancing the wire was a reason for changing first approach. We observed a case of pose failure despite the percutaneous puncture of the internal jugular and the dissection of the cephalic. It was an elderly, tired with a poor general condition. We think it is important that the surgeon controls at least three different venous approaches so to protect the venous capital and secured patient.
The complications or immediate peri-postoperative difficulties described by Peillon C et al. [11], such as hematoma or pneumothorax are known. They relate to some specific approaches. The absence of this type of complication in this study could be explained by the predominance of the percutaneous approach but also for a good dissection and hemostasis of the compartment of the implantable chamber. The presence of the image intensifier was reduced these complications. Infection is the main and most redoubted complication. It very often occurs at a distance from the operating room, which suggests that it is linked to the use or handling of the implantable chamber. A study by the French national alert network for investigations and surveillance of nosocomial infections (Raisin) [16] did not find any difference between the different puncture sites on the rate of nosocomial infection during the central access venous. According to some authors, its rate remains low, less than 1% [17].
In this study, local infections were caused by extravasation of drugs with skin necrosis. The two cases of malignant hyperthermia in the absence of isolated germs were considered to be related to PortA-Cath. Device ablation was performed in these cases associated to probabilistic broad-spectrum antibiotic. No germ was identified with the culture of device. The prevention of these infections requires strict compliance with the rules of asepsis from the operating room and the treatment room. Mechanical complications such as venous thrombosis, rupture with migration of the catheter for vena cava or in right atrium widely described in the literature wasn’t observed [18,19].
These outcomes would be related to internal percutaneous jugular approach considered to have low complications. The position of the distal end of the catheter was considered a major risk factor for thrombosis. Studies have shown that the rate of venous thrombosis in an implantable catheter chamber can reach 40 to 50% when the distal end of the catheter is above the level of the carina [20, 21].
Thus a standard recommendation was made by consensus: "the distal end of the central venous catheter should be located at the junction of the superior vena cava and the right atrium". Also it is necessary to have a means of controlling the position of the catheter intraoperatively during the placement of a chamber either by an intraoperative fluoroscopy or a control radiograph made before skin closure. The end of the catheter should project about 2 vertebral bodies under the bronchial bifurcation. Echo guidance and amplifier are necessary and essential instruments for the placement of an implantable catheter chamber. To improve the quality of care and patient safety, the acquisition of these devices is a mandatory condition for any implantation center.
Conclusion
The Port-A-Cath (PAC) is a necessity in oncology. As the number of cancer patients increases, we are forced to train and retrain to meet the demand for quality care from these increasingly demanding patients. The internal jugular vein percutaneous approach appears to have the best “quality price” ratio in terms of technical feasibility / complications, particularly on the right side.
References
- Niederhuber JE, Ensminger W, Gyves JW, et al. Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery. 1982; 92: 706-712.
- National Agency for Health Assessment (ANAES). Assessment of professional practices in healthcare establishments - Assessment of the quality of use and monitoring of implantable catheter chambers. 2000.
- High Authority for Health (HAS) France. Assessment of the quality of use and monitoring of implantable catheter chambers. 2005.
- www.afsos.org: French-speaking association for supportive oncological care. Letter no 2, June 2009.
- Biffi R, Orsi F, Pozzi S, et al. Best choice of central venous insertion site for the prevention of catheter-related complications in adult patients who need cancer therapy: a randomized trial. Ann Oncol. 2009; 20: 935-940.
- Schuld J, Richter S, Moussavian MR, et al. A totally implantable venous access device - Implantation in general or local anesthesia? A retrospective cost analysis. Zentralbl Chir. 2009; 134: 345-349.
- Ruesch S, Walder B, Tramer MR. Complications of central venous catheters: internal jugular versus subclavian access, a systematic review. Crit Care Med. 2002; 30: 454-460.
- Lovino F, Pittiruti M, Buononato M, et al. Central venous catheterization: complications of different placements. Ann Chir. 2001; 126: 1001-1006.
- Bazelly B. Pre-pectoral perfusion site: placement by direct puncture of the subclavian vein. J Chir. 2005; 142: 240-243.
- Le Ray Ferrières I, Guinier D. 2D guidance Ultrasound for the installation of implantable chambers. Journal of Surgery. 2009; 146: 528-531.
- Peillon C, Melki J, Baste JM, et al. How I install an implantable chamber (CIP). Progress in Urology- FMC. 2013; 23: 129-132.
- Valverde A. Implantable chamber placement by percutaneous supraclavicular approach. Journal of Surgery. 2007; 144: 323-326.
- Hind D, Calvert N, McWilliams R, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003; 327: 361.
- Dimitrios Karakitsos, Nicolaos Labropoulos, Eric De Groot, et al. Real-time ultrasound-guided catheterization of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006; 10: 162.
- National Institute for clinical excellence. NICE technology appraisal guidance No 49: guidance on the use of ultrasound locating devices for placing central venous catheters. London: NICE September 2002.
- Olivier M, Héritaud F, Maugeat S. CCLIN Nord, REA Raisin 2005 monitoring results.
- French Society of Hospital Hygiene (SF2H). Prevention of infections associated with implantable catheter chambers for venous access. Professional recommendations by formal consensus of experts. Hygienes. 2012; 20: 1-80.
- Balestreri L, De Cicco M, Matovic M, et al. Central venous catheter-related thrombosis in clinically asymptomatic oncologic patients: a phlebographic study. Eur J Radiol. 1995; 20: 108-111.
- Hassane Kabiri EI, Massine El Hammoumi, Akram Traibi, et al. Catheters With Implantable Chamber: Report of a Series of 970 Cases. Pan African Medical Journal. 2012; 12: 72.
- Luciani A, Clement O, Halimi P, et al. Catheter-related upper extremity deep venous thrombosis in cancer patients: a prospective study based on Doppler US. Radiology. 2001; 220: 655-660.
- Cadman A, Lawrance JAL, Fitzsimmons L, et al. To clot or not to clot? That is the question in central venous catheters. Clin Radiology. 2004; 59: 349-355.