Knowledge and Attitude toward Bariatric Surgery among Family Medicine Residents in Riyadh City, Saudi Arabia
Author'(s): Abeer Alkhathlan*, Atheer Alhumid1, Hessah Alsayahi2, Malak Albalawi3 and Khalid Alamri4
Family Medicine Residency Program, King Fahad Medical City,Riyadh, Saudi Arabia.
*Correspondence:
Abeer Alkhathlan, Family Medicine Residency Program, King Fahad Medical City, Riyadh, Saudi Arabia.
Received: 04 Jul 2024 Accepted: 05 Aug 2024
Citation: Alkhathlan A, Alhumid A, Alsayahi H, et al. Knowledge and Attitude toward Bariatric Surgery among Family Medicine Residents in Riyadh City, Saudi Arabia. Diabetes Complications. 2024; 8(3); 1-10.
Abstract
Introduction: This study explores the knowledge and attitudes of family medicine residents in Riyadh, Saudi Arabia, towards bariatric surgery for obesity management. Given the high obesity rates and associated comorbidities, understanding healthcare professionals' perspectives is vital for enhancing patient care and referral practices.
Methods: A cross-sectional survey was conducted from April 2023 to March 2024, targeting family medicine residents in Riyadh's Cluster 2. The study assessed knowledge and attitudes regarding bariatric surgery's efficacy, safety, and referral standards. The study included actively practicing residents, while those outside Riyadh were excluded. Statistical analysis involved descriptive and inferential statistics to correlate knowledge and attitudes with demographic variables.
Results: The survey included 109 respondents, predominantly from King Fahad Medical City. Knowledge assessment revealed variable understanding: 85.32% correctly identified the safest surgical technique, while only 16.51% understood the impact on cancer risk. The average knowledge score was 6.56 ± 1.57, with a significant association between perceived and actual knowledge (P < 0.001). Attitudes were generally positive, with 85% acknowledging bariatric surgery's role in diabetes management. However, no significant correlation was found between knowledge levels and attitudes (P = 0.68). There was no significant difference in knowledge or attitudes based on gender or practice setting, though a notable disparity in attitudes emerged, with physicians in primary healthcare centers displaying more favorable views (P = 0.001) towards bariatric surgery compared to their hospital counterparts.
Conclusion: Family medicine residents in Riyadh show a promising openness towards bariatric surgery but exhibit gaps in specific knowledge areas. Targeted educational programs could bridge these gaps, potentially improving obesity management through informed referrals and support for bariatric surgery as a viable treatment option.
Keywords
Introduction
Increased Body mass index (BMI) is associated with several comorbidities, including type 2 diabetes mellitus, hypertension, dyslipidemia, obstructive sleep apnea, asthma, hypertrophic cardiomyopathy, gallstones, many types of cancer, psychological and social impairment [1,2]. As a result of higher absenteeism rates, productivity loss, and premature mortality, obesity is strongly associated with high mortality, diminished quality of life, and higher healthcare costs [3].
According to the World Health Organization (WHO), in 2022, 43% of adults aged 18 years and over were overweight and 16% were living with obesity [4]. In 2019, the Saudi Ministry of Health (MOH) published the most recent findings of the Saudi data from the World Health Organization’s World Health Survey (SAWHS). Reported data indicates that 20% of individuals in Saudi Arabia were classified as obese, with a greater prevalence observed among females (21%), residents of metropolitan areas (21%), and individuals lacking formal education (29%). Obesity rates rose with age, starting at 10% in the 18–29 age group and peaking at 20% in the 70–79 age group, then declining to 22% in individuals over 80 years old [5].
Research indicates that sustained weight loss has positive effects on preventing and resolving various health problems and improving quality of life [6]. Many studies have indicated that dieting and lifestyle changes rarely yield long-term results [7,8]. Therefore, bariatric surgery has emerged as a leading treatment option for obese patients. Bariatric surgery is now readily accessible in both community and academic settings as a weight loss treatment for severely obese individuals [9]. PCPs, hospitals, and insurers have utilized the 1991 NIH Consensus Statement as a benchmark for the selection criteria for bariatric surgery [10]. BMI and comorbidities determine bariatric surgery eligibility. Patients who have a BMI of 35 kg/m2 or above with obesity-related diseases such as type 2 diabetes, hypertension, OSA, and dyslipidemia, or 40 kg/m2 or higher without comorbidities, are surgical candidates. Patients between 18 and 60 who have failed conservative treatment are also candidates for bariatric surgery [10].
Despite its role in the management of obesity, several studies have shown that primary care physicians (PCPs) lack understanding and have misconceptions about bariatric surgery and its indications. This is particularly important since a multidisciplinary approach is necessary to manage obesity, and the treatment options can vary depending on many factors. Thus, appropriate knowledge regarding the various aspects of bariatric surgery is essential to ensure favorable long-term outcomes.
Despite a high prevalence of obesity among their patients, many primary care providers do not initiate discussions about weight loss options, citing concerns about patient qualifications and the risks of surgery [11]. Perlman and Auspitz discovered that PCPs had restricted knowledge and frequently felt uneasy while talking about or recommending patients for bariatric surgery [12,13]. In addition, another study showed that physicians expected a larger weight loss with pharmacotherapy than is realistic [14]. Major and Tork highlighted the importance of education and tools to enhance knowledge regarding bariatric surgery [15,16]. Balduf and Presutti proposed that PCPs with a deeper understanding of bariatric surgery standards and access to superior resources are more inclined to recommend patients for surgery and offer postoperative support [17,18]. These findings underscore the importance of targeted education and communication strategies to improve understanding and access to bariatric surgery. The current study aimed to assess the knowledge and attitudes of family medicine physicians towards bariatric surgery in Cluster 2, Riyadh, Saudi Arabia.
Methods
Study Design
A cross-sectional study was conducted to assess the knowledge and attitudes of family medicine physicians towards bariatric surgery in Cluster 2, Riyadh, Saudi Arabia. The study spanned from April 2023 to March 2024 and involved using a structured questionnaire to assess the respondents’ knowledge and attitude towards bariatric surgery. The study setting encompassed various healthcare facilities within Riyadh’s Cluster 2, including King Fahad Medical City, Primary Care Centers, and Prince Mohammad Bin Abdul-Aziz Hospital.
Participants and Recruitment
The study targeted family Medicine residents, all actively practicing within Riyadh’s Cluster 2 healthcare facilities. This inclusion criteria ensured a broad spectrum of medical professionals, covering both genders and a range of age groups, to comprehensively assess their knowledge and attitudes towards bariatric surgery.
The exclusion criteria were set to omit non-consenting physicians, those specialized in fields outside the study’s focus, practitioners operating outside the confines of Riyadh’s Cluster 2 or the city itself, and non-physician healthcare providers. Residents were randomly approached during working hours in clinics across Riyadh’s Cluster 2. The recruitment process was designed to ensure a diverse representation of specialties and practice settings.
Data Collection
The study questionnaire was divided into three sections. The initial section requested socio-demographic information from the physicians, including age, gender, area of practice, specialty, position, and years of practice. The knowledge section comprised thirteen case scenarios designed to evaluate the physicians’ understanding of bariatric surgery, covering patient eligibility criteria, preferred surgical techniques, and expected outcomes. All questions were multiple choice (MCQ) with only one possible correct answer per scenario. One Likert-scale question, on a scale from 1 (very unsatisfied) to 5 (very satisfied), was used to allow the respondents to self-assess their overall knowledge about surgical treatment of obesity. The final attitudes section contained four questions to assess the physicians’ perspectives on the efficacy, safety, and personal recommendations regarding bariatric surgery for treating obesity.
Sample Size Calculations
Given the exploratory nature of the research as a pilot study, the sample size was determined through a pragmatic approach rather than traditional statistical power analysis. This methodological choice acknowledges the pilot study’s primary goals to refine survey instruments, estimate population variance, and establish feasibility for a larger-scale study. Convenience sampling of physicians who were available and willing to participate during the study period was used to achieve meaningful insights while maintaining manageability in analysis. The collected responses from this initial cohort will be utilized to calculate effect sizes, facilitating a more accurate and statistically powered sample size determination for future studies investigating physicians’ perspectives on bariatric surgery in the region.
Knowledge and Attitude Scoring
Regarding knowledge, respondents were awarded one point for each correct answer and zero otherwise. The total score was calculated as the sum of the correct points with a maximum possible score of 12. Regarding attitude, respondents were awarded one point if they answered “yes” and zero otherwise.
Statistical Analysis
Statistical analysis was performed using R v 4.3. Counts and percentages were used to summarize categorical variables. The mean ± standard deviation (SD) and the medina/interquartile range (IQR) were used for continuous normal and non-normal variables, respectively. The Chi-square test of independence was used to assess the association between categorical variables. Unpaired t-test and One-way ANOVA were used to compare the knowledge and attitude scores between two and more than two groups,respectively. Spearman’s correlation was used to assess whether a statistically significant linear trend existed in the association between the different included variables. A p-value of <0.05 was considered statistically significant.
Ethical Considerations
The Institutional Review Board of King Fahad Medical City reviewed and approved the study protocol. Informed consent was obtained from all participating physicians prior to their involvement in the study, ensuring confidentiality and the right to withdraw at any point without repercussions.
Results
Socio-demographic characteristics of the respondents
The study involved a total of 109 respondents, all of whom were aged between 25 to 35 years. The distribution of males and females was balanced with 51 male participants (46.8%) and 58 female participants (53.2%). The majority of respondents, 103 out of 109 (94.5%), reported their area of practice as King Fahad Medical City (KFMC), with the remaining 6 (5.5%) working in Primary Health Care (PHC) centers, indicating a significant concentration of participants from a major healthcare institution. All respondents specialized in Family Medicine (FM) and had less than five years of experience.
Knowledge regarding Bariatric Surgery
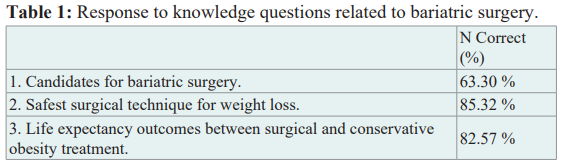
Results revealed a heterogeneous understanding across different areas (Table 1). Most respondents (85.32%) identified the safest surgical technique for weight loss. Conversely, only 16.51% knew the impact of obesity surgery on cancer risk. Other notable findings included a strong awareness of life expectancy outcomes between surgical and conservative obesity treatment (82.57%) and a good understanding of the BMI and comorbidities criteria for bariatric surgery consideration (75.23%). However, areas such as the most effective surgical procedure for reducing obesity-related comorbidities (24.77%) and the recommended safe period to avoid conception post-surgery (28.44%) revealed low knowledge among the respondents. Only one-third of respondents (32.11%) knew the mortality rate associated with Roux-en-Y gastric bypass, and one- half (55.05%) knew the suitable form of thromboprophylaxis after bariatric surgery.
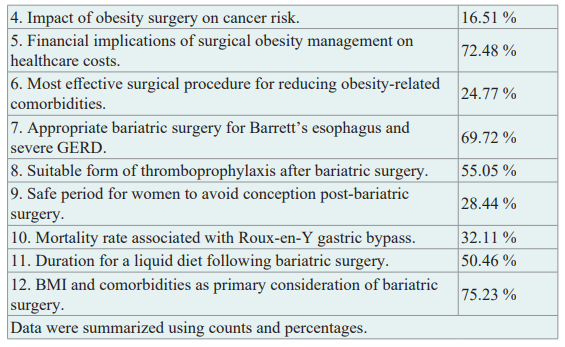
Regarding perceived satisfaction with knowledge, the majority of respondents, 61 (56.0%), were neutral, and 22 (20.2%) were unsatisfied. Very few respondents were very unsatisfied (3, 2.8%) or very satisfied (2, 1.8%) with their knowledge. The distribution of knowledge scores shows that the most common scores were 6, 7, and 8, with 29 (26.6%), 28 (25.7%), and 21 (19.3%) respondents, respectively, suggesting a moderate level of knowledge among the participants. Approximately 20% of the respondents scored < 6, and only 10% scored> 8. The average knowledge score was 6.56 ± 1.57 points, with 50% of the respondents scoring between 6 and 8 points. Interestingly, none of the respondents achieved a score of 11 or 12.
The graph represents a violin plot combined with a box plot and scatter plot elements, comparing perceived knowledge to actual knowledge scores. The violin plot aspect provides a density estimation showing where the data points are more common; the width of the shaded area represents the concentration of data points at different score levels, giving a visual sense of the distribution. Inside each violin, there is a box plot that indicates the interquartile range (IQR) with a line representing the median and ‘whiskers’ that might represent the range of the data, excluding outliers. Overlaid on this are points that may represent the individual knowledge scores of the respondents, with the red point highlighting the mean knowledge score for each level of perceived knowledge.
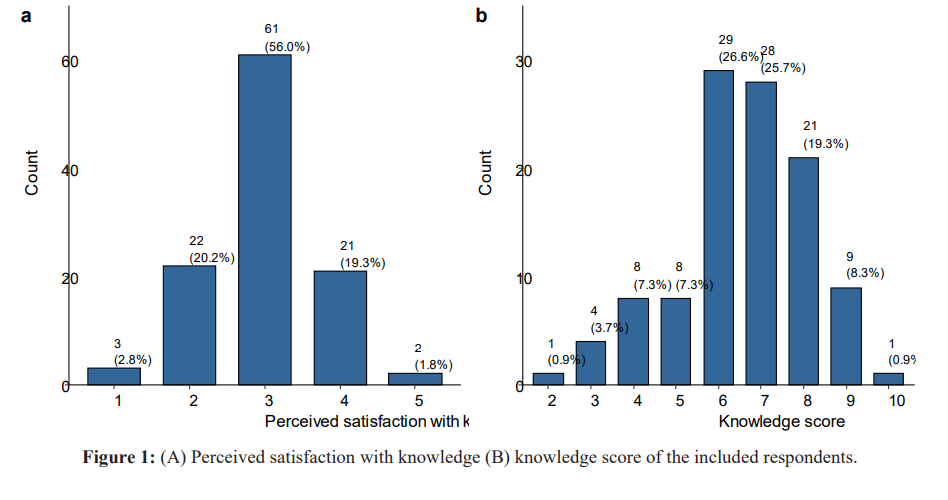
A statistically significant association was observed between perceived knowledge and the actual knowledge score (Figure 2, P < 0.001). Post-hoc pairwise comparisons showed that the average knowledge score was significantly different between satisfied respondents and those who were not satisfied (P = 0.02). In addition, a statistically significant linear trend was observed in the association between both domains (P = 0.004).
Attitude towards Bariatric Surgery
These responses (Figure 3) suggested confidence in the efficacy of bariatric surgery regarding its different applications. However, some questions showed a greater degree of uncertainty or opposition relative to the others. The majority of the included residents affirmed the role of bariatric surgery in managing diabetes, with 85% in agreement, while 74% recognized its effectiveness in achieving ideal weight loss, and 72% endorsed its safety and reliability for obesity and metabolic disease treatment. Only two-thirds (64%) would recommend bariatric surgery for individuals with class III obesity or related metabolic conditions.
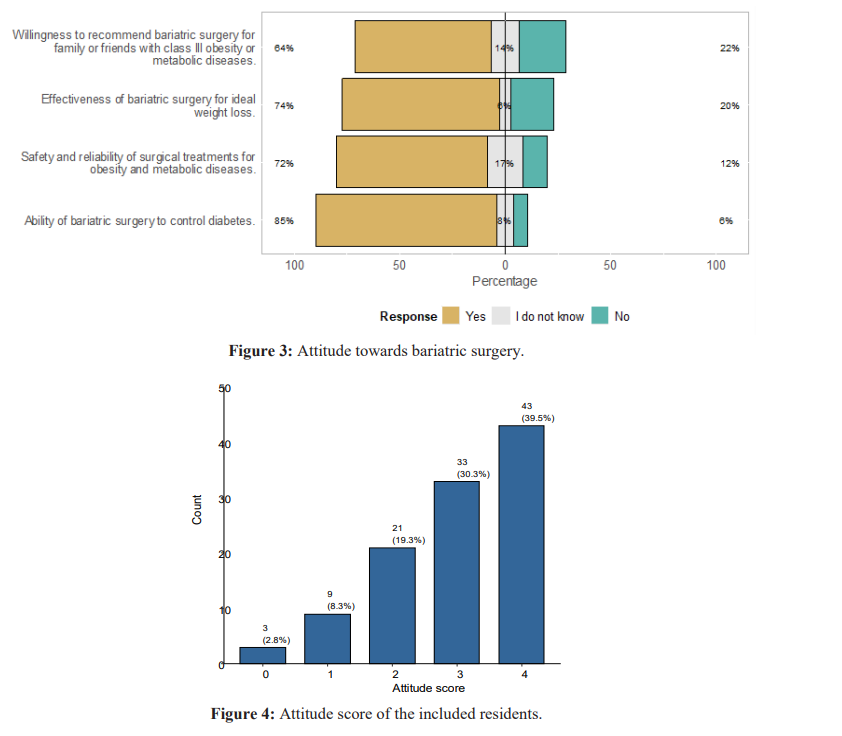
Results (Figure 4) suggest a generally positive attitude among most respondents, with a significant proportion holding favorable views. Most respondents (n = 43, 39.5%) scored the highest on the attitude scale (4), indicating a very positive attitude. Another third (n = 33, 30.3%) scored a 3, suggesting a moderately positive attitude. Fewer respondents scored a 2 (n = 21, 9.3%) and fewer a 1 (n = 9, 8.3%), showing a less favorable attitude. Only a minimal number (n = 3, 2.8%) scored a 0, indicating a negative attitude toward bariatric surgery.
Association between Knowledge, Attitudes, and Perceived Satisfaction with Knowledge
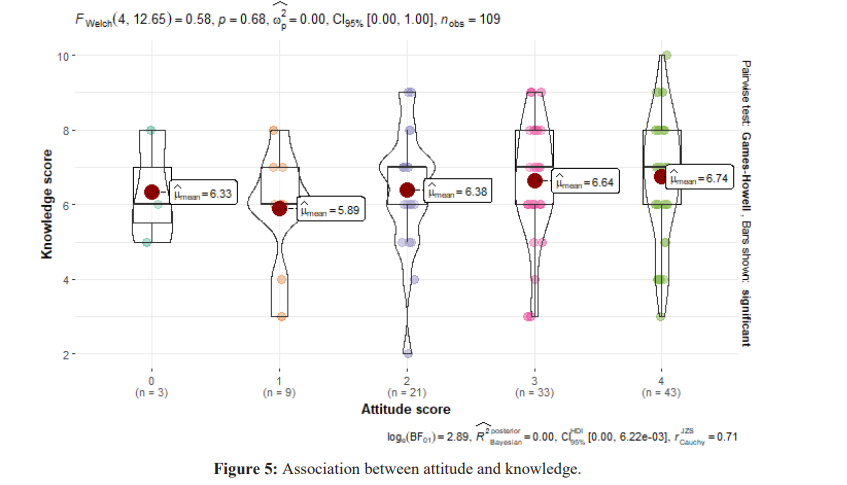
The graph represents a violin plot combined with a box plot and scatter plot elements, comparing perceived knowledge to actual knowledge scores. The violin plot aspect provides a density estimation showing where the data points are more common; the width of the shaded area represents the concentration of data points at different score levels, giving a visual sense of the distribution. Inside each violin, there is a box plot that indicates the interquartile range (IQR) with a line representing the median and ‘whiskers’ that might represent the range of the data, excluding outliers. Overlaid on this are points that may represent the individual knowledge scores of the respondents, with the red point highlighting the mean knowledge score for each level of perceived knowledge.
No statistically significant association was observed between attitude and knowledge towards bariatric surgery (P = 0.68). No statistically significant association was observed between attitude and knowledge (r = 0.145, P > 0.05).
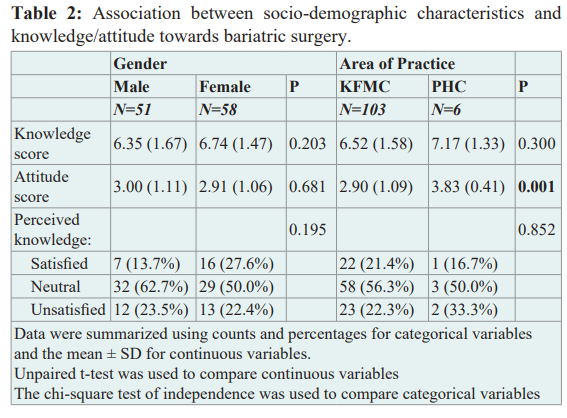
In the study, male physicians reported an average knowledge score of 6.35 + 1.67 compared to female physicians, who scored slightly higher, averaging 6.74 ± 1.47; however, this difference was not statistically significant (P = 0.203). When examining attitudes, males had an average attitude score of 3.00 ± 1.11, while females had a comparable score of 2.91 ± 1.06, with the difference again not being significant (P = 0.681). In terms of area of practice, physicians at King Fahad Medical City (KFMC) had an average knowledge score of 6.52 ± 1.58, and those in Primary Health Care (PHC) centers had a higher average score of 7.17 ± 1.33, but this difference was not statistically significant (P = 0.300). The attitude scores differed significantly, with KFMC physicians averaging 2.90 ± 1.09 and PHC physicians averaging higher at 3.83 ± 0.41 (P = 0.001). For satisfaction with perceived knowledge, the levels were higher among female physicians (27.6%) than male physicians (13.7%), with the majority being neutral for both genders and all practice areas. The proportions of those unsatisfied with their perceived knowledge were similar across genders and practice areas.
Discussion
Research has shown that obesity is linked to various harmful health conditions such as type 2 diabetes, hypertension, high cholesterol, asthma, and arthritis [19]. Obesity has been linked to more than 65 comorbidities, including coronary artery disease, type 2 diabetes mellitus, hypertension, hypercholesterolemia, several types of cancer, and other diseases [20]. Fortunately, long-term weight loss is linked to many of these health concerns’ prevention, relief, and resolution [21]. In light of these findings, bariatric surgery has emerged as a successful treatment for obese patients [22,23]. Unlike standard dieting methods that frequently do not produce lasting outcomes, individuals who undergo bariatric surgery typically lose an average of 20 to 30 kg and retain this weight reduction over time [24].
Although obesity substantially impacts patient care in all disciplines of medicine, physician and medical student education about obesity is limited [25,26]. These educational gaps may leave physicians inadequately prepared to address the needs of this substantial and growing portion of their patient population. The current study aimed to assess the knowledge and attitude of family medicine residents in Riyadh towards bariatric surgery. The study had the advantage of including a homogenous population of family medicine residents from multiple healthcare settings. In addition, few studies were conducted in Asia in contrast to other regions where many studies were conducted. The current study also included only family residents, unlike other studies that included only non-resident PCPs with varying experience levels.
The current study showed an average level of knowledge among the included respondents. The majority of respondents (~75%) also were not satisfied with their knowledge regarding bariatric surgery. The limited awareness of bariatric surgery and its indications among family medicine residents may impact their decision-making process, potentially affecting the referral of cases where such intervention is necessary. The consequences of this knowledge gap can be severe, emphasizing the critical nature of multidisciplinary teams and approaches in managing obesity. Effective management relies on various factors, including comprehensive lifestyle interventions, exercise, diet therapy, pharmacotherapy, and surgery. This underscores the importance of informed referrals to ensure that all patients receive appropriate care tailored to their specific needs [27,28].
In Canada, a study assessed the knowledge and perception regarding bariatric surgery among primary care physicians. Results showed that 71% of the included physicians referred no more than 5 % of their morbidly obese patients for surgery, and only one-third had the appropriate equipment and resources to manage obese patients. Moreover, only one-quarter felt comfortable explaining the procedural options to patients [12]. The study also showed that most physicians (92.5%) wanted more education about bariatric surgery, which reflects low perceived knowledge, similar to what was reported in the Canadian study. The two studies were similar: both reflected a positive attitude towards bariatric surgery, and 81.9% mentioned they would refer a family member for surgery [12].
Several studies were conducted in different regions to explore the knowledge and attitude of primary care physicians and family medicine practitioners in particular towards bariatric surgery. Results indicated a significant knowledge gap among family medicine physicians regarding bariatric surgery [29]. This gap was evident in their understanding of the role of bariatric surgery in treating obesity, patient selection, and postoperative care [12,13,18].
In the USA, another study showed that misconceptions about bariatric surgery exist in the family practice community despite the increasing frequency of these procedures. The study suggested that educational programs need to be designed to assist family practitioners in treating and referring obese patients. The low knowledge was also demonstrated by the fact that only 57% were comfortable explaining the procedure [13]. The need for educational programs to improve physician knowledge and competency in treating obesity, including bariatric surgery, was also emphasized in another study [30]. The low average knowledge score in the current study further augments these results.
In addition, the % of correct answers varied from 25% to 85%. The discrepancy in knowledge levels may be due to the limited research- based evidence on the advantages, drawbacks, and methods of bariatric surgeries, as highlighted by Aikenhead et al., who noted that inconsistencies in guidelines and evidence regarding bariatric surgery have a significant impact on the existing knowledge in this field [31].
Only two-thirds of the respondents correctly identified the candidates for bariatric surgery. The low knowledge regarding bariatric surgery indications could be explained by the lack of familiarity with the guidelines for bariatric surgery, a finding that was corroborated by many studies. For example, less than half of the included PCP reported reading or being familiar with the NIH criteria [17,32,33]. The knowledge has been shown to vary by region. Tork et al. found that 85% of primary care physicians in a private teaching hospital in the US agreed that a BMI > 35 kg/m2 and comorbidities were reasons for a surgical referral [16]. Outside the USA, Major et al. and Memarian et al. found that 81.8% of surveyed PCP in Poland and 73% of PCPs in Sweden were aware of the indications for a bariatric treatment or believed they had a solid understanding of referral criteria, respectively [15,34]. These results were similar to those reported in the current study and higher than those reported in Canada, where one-half were supportive of metabolic surgery for patients with diabetes who have a BMI < 35 kg/m2 [12].
Over half of the participating physicians correctly identified Low Molecular Weight Heparin (LMWH) as the right method of postoperative thromboprophylaxis for post-bariatric surgery. These findings might be linked to the extensive literature and expertise in nutrition, endocrinology, metabolism, bone density loss, normal flora growth, and other ongoing study areas. Approximately one-third of the participating physicians correctly identified the recommended length of conception avoidance for females who had bariatric surgery as 12-18 months, as advised by the American Association of Clinical Endocrinologists, the Obesity Society, and the American Society for Metabolic & Bariatric Surgery. The results align with those published by Alqahtani et al. [20], indicating that Saudi doctors had a limited understanding of the pregnancy avoidance period for women who had bariatric surgery [35].
In contrast to the low knowledge score, most respondents had a positive attitude towards bariatric surgery. The younger age of the included respondents could explain this. This was demonstrated in another study, which showed that younger primary care physicians are more likely to have received some obesity training than older PCPs. [30]. In addition, the relationship between knowledge and attitudes toward bariatric surgery among PCPs is complex and influenced by various factors, including their educational background, experience, and the perceived barriers to referral. Several studies have explored this topic, providing insights into why some PCPs may have positive attitudes towards bariatric surgery but still demonstrate low referral rates or inadequate knowledge about the procedure and its benefits, similar to what was reported in the current study [15]. These factors can significantly impact the care and treatment options provided to obese patients, including those with diabetes and a BMI < 35 kg/m2 [36,37]. Another study highlighted that primary care physicians tend to underprioritize obesity treatment and may overestimate the risks associated with bariatric surgery. This finding suggests that educational interventions targeting PCPs could address misconceptions about bariatric surgery’s effectiveness and safety [38].
The association between gender and knowledge regarding bariatric surgery was explored in several studies. In Germany, Egerer et al. found that male PCPs self-reported higher knowledge of bariatric procedures than females [39]. However, no such association was reported in the current study. This is similar to what was reported in another study in Saudi Arabia [36]. In addition, we observed no correlation between knowledge and attitude among residents. Two other studies reported a correlation between knowledge and attitude, although the correlation was weak and could be explained by the differences in the study populations and the large sample size in these two studies compared to the current one [34,36]. The lack of correlation between both parameters may also explain the discrepancy between the number of patients needing bariatric surgery and those referred, as observed in several studies [12,15].
Limitations
The current study had several limitations. First, It was exploratory, primarily serving as a pilot study without a statistically powered sample size, which may affect the strength and generalizability of its findings. Using convenience sampling could introduce bias, as it might not accurately represent the broader population of family medicine residents. The focus on a specific geographic region and a particular healthcare setting, primarily King Fahad Medical City, could limit the applicability of results to other areas or different healthcare environments.
Additionally, while contributing to a focused analysis, the study’s inclusion of family medicine residents excludes a broader spectrum of medical professionals who also manage obesity. Reliance on self-assessment for evaluating knowledge and attitudes might not fully capture actual understanding or practices related to bariatric surgery. Furthermore, its cross-sectional design captures only a snapshot, not accounting for how perceptions might evolve with ongoing medical education or changes in the medical community’s approach to obesity treatment. Expanding future research to address these limitations could enhance understanding and provide more comprehensive insights into the medical community’s perception of bariatric surgery.
Conclusion
Residents specializing in family medicine in cluster two of Riyadh City exhibited diverse levels of knowledge and positive attitudes toward bariatric surgery. Efforts should be made to increase family medicine residents’ understanding and awareness of the advantages, risks, methods, and reasons for bariatric surgery. This can be achieved by involving them in fundamental and advanced health education workshops, as well as courses focused on surgical treatment of obesity and metabolic issues.
References
- Martin-Rodriguez E, Guillen-Grima F, Martí A, et al. Comorbidity associated with obesity in a large population The APNA study. Obes Res Clin Pract. 2015; 9: 435-447.
- Lam BC, Lim AL, Chan S, et al. The impact of obesity a narrative review. Singapore Med J. 2023; 64: 163.
- Goettler A, Grosse A, Sonntag D. Productivity loss due to overweight and obesity A systematic review of indirect BMJ Open. 2017; 7: e014632.
- The World Health Organisation. Obesity and overweight. 2024. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- World Health Survey Saudi Arabia KSAWHA 2019 Final Report. Minist Heal. 2020; 1: 5-24.
- Haase CL, Lopes S, Olsen AH, et al. Weight loss and risk reduction of obesity-related outcomes in 0.5 million people evidence from a UK primary care database. Int J Obes. 2021; 45: 1249-1258.
- Park JY, Heo Y, Kim YJ, et al. Long-term effect of bariatric surgery versus conventional therapy in obese Korean patients A multicenter retrospective cohort Ann Surg Treat Res. 2019; 96: 283-289.
- Martins C, Strømmen M, Stavne OA, et al. Bariatric surgery versus lifestyle interventions for morbid obesity- Changes in body weight risk factors and comorbidities at 1 year. Obes Surg. 2011; 21: 841-849.
- Ellison SR, Ellison SD. Bariatric Surgery A Review of the Available Procedures and Complications for the Emergency Physician. J Emerg Med. 2008; 34: 21-32.
- Grundy SM, Barondess JA, Bellegie NJ, et Gastrointestinal surgery for severe obesity. Ann Intern Med. 1991; 115: 956-961.
- Lopez EKH, Helm MC, Gould JC, et al. Primary care providers attitudes and knowledge of bariatric surgery. Surg Endosc. 2020; 34: 2273-2278.
- Auspitz M, Cleghorn MC, Azin A, et al. Knowledge and Perception of Bariatric Surgery Among Primary Care Physicians a Survey of Family Doctors in Obes Surg. 2016; 26: 2022-2028.
- Perlman SE, Reinhold RB, Nadzam GS. How do family practitioners perceive surgery for the morbidly obese. Surg Obes Relat Dis. 2007; 3: 428-433.
- Glauser TA, Roepke N, Stevenin B, et Physician knowledge about and perceptions of obesity management. Obes Res Clin Pract. 2015; 9: 573-583.
- Major P, Stefura T, Jezierska-Kazberuk M, et al. The knowledge of Polish primary care physicians about bariatric surgery. Wideochirurgia I Inne Tech Maloinwazyjne. 2016; 11: 164-170.
- Tork S, Meister KM, Uebele AL, et al. Factors influencing primary care physicians referral for bariatric surgery. J Soc Laparoendosc Surg. 2015; 19: e2015.
- Balduf LM, Farrell Attitudes Beliefs and Referral Patterns of PCPs to Bariatric Surgeons. J Surg Res. 2008; 144: 49-58.
- Presutti RJ, Gorman RS, Swain Primary Care Perspective on Bariatric Surgery. Mayo Clin Proc. 2004; 79: 1158-1166.
- Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity diabetes and obesity-related health risk factors J Am Med Assoc. 2003; 289: 76-79.
- Guh DP, Zhang W, Bansback N, et al. The incidence of comorbidities related to obesity and overweight A systematic review and meta-analysis. BMC Public Health. 2009; 9: 88.
- Dhabuwala A, Cannan RJ, Stubbs RS. Improvement in comorbidities following weight loss from gastric bypass surgery. Obes Surg. 2000; 10: 428-435.
- Hoerger TJ, Zhang P, Segel JE, et al. Cost-Effectiveness of Bariatric Surgery for Severely Obese Adults With Diabetes. Diabetes Care. 2010; 33: 1933-1939.
- Maciejewski ML, Arterburn Cost-effectiveness of Bariatric Surgery. JAMA. 2013; 310: 742.
- Bessesen DH. Meta-analysis Surgical Treatment of Obesity. Yearb Endocrinol. 2006; 2006: 172-174.
- Bocquier A, Verger P, Basdevant A, et Overweight and obesity Knowledge attitudes and practices of general practitioners in France. Obes Res. 2005; 13: 787-795.
- Cade J, O’Connell S. Management of weight problems and obesity Knowledge attitudes and current practice of general practitioners. Br J Gen Pract. 1991; 41: 147-150.
- Montesi L, Ghoch M El, Brodosi L, et al. Long-term weight loss maintenance for obesity A multidisciplinary approach. Diabetes Metab Syndr Obes. 2016; 9: 37-46.
- Bischoff SC, Boirie Y, Cederholm T, et al. Towards a multidisciplinary approach to understand and manage obesity and related diseases. Clin Nutr. 2017; 36: 917-938.
- Rajeev ND, Samaan JS, Premkumar A, et al. Providers Knowledge and Perceptions of Bariatric Surgery a Systematic Review. Obes Surg. 2023; 33: 3571-3601.
- Stanford FC, Johnson ED, Claridy MD, et The Role of Obesity Training in Medical School and Residency on Bariatric Surgery Knowledge in Primary Care Physicians. Int J Family Med. 2015; 2015: 1-8.
- Aikenhead A, Lobstein T, Knai Review of current guidelines on adolescent bariatric surgery. Clin Obes. 2011; 1: 3-11.
- Avidor Y, Still CD, Brunner M, et al. Primary care and subspecialty management of morbid obesity Referral patterns for bariatric surgery. Surg Obes Relat Dis. 2007; 3: 392-407.
- Hirpara DH, Cleghorn MC, Kwong J, et al. Perception and Awareness of Bariatric Surgery in Canada a National Survey of General Surgeons. Obes Surg. 2016; 26: 1799-1805.
- Memarian E, Carrasco D, Thulesius H, et al. Primary care physicians knowledge attitudes and concerns about bariatric surgery and the association with referral patterns a Swedish survey study. BMC Endocr Disord. 2021; 21: 62.
- Alqahtani N, Alkhudairi S, Aljahli M, et al. Awareness and knowledge of the obstetric and gynecological impact of bariatric surgery among women in the Eastern Province of Saudi Arabia. J Fam Med Prim Care. 2019; 8: 3678.
- Alenezi AM, Thirunavukkarasu A, Alrasheed AK, et al. Primary Care Physicians Knowledge Attitude and Potential Referral Barriers towards Bariatric Surgery A Northern Saudi Study. Medicina. 2022; 58: 1742.
- Özgüç H, Narmanli M, Çirnaz H. Turkish primary care physicians attitudes and knowledge of obesity and bariatric surgery a survey Turkish J Surg. 2021; 37: 2660-2676.
- Funk LM, Jolles SA, Greenberg CC, et al. Primary care physician decision making regarding severe obesity treatment and bariatric surgery A qualitative Surg Obes Relat Dis. 2016; 12: 893-901.
- Egerer M, Kuth N, Koch A, et al. General practitioners knowledge about bariatric surgery is associated with referral practice to bariatric surgery centers. Int J Environ Res Public Health. 2021; 18: 10055.
