Knowledge of Direct Oral Anticoagulants (DOACS) and Limits of Their Prescription: Survey of Cardiologists, Intensivists, Neurologists and Pulmonologists in Senegal
Author(s): Sarr Simon Antoine1*, Keita Fatoumata1, Aw Fatou1, Mingou Joseph Salvador1, Diouf Youssou1, Diop Khadimu Rassoul1, Beye Serigne Mor2, Ngaidé Aliou Alassane3, Bodian Momar1, Ndiaye Mouhamadou Bamba1, Mbaye Alassane3, Kane Adama2, Diao Maboury1 and Kane Abdoul4
1Cardiology Unit, Aristide Le Dantec Hospital, Dakar.
2URF2S Saint Louis.
3HOGGIP Hospital, Dakar.
4Cardiology Unit, Dalal Jamm Hospital, Dakar
*Correspondence:
Sarr Simon Antoine, Cardiology Unit, Aristide Le Dantec hospital, Dakar, Senegal, Tel: +221 775423125.
Received: 10 Nov 2023; Accepted: 17 Dec 2023; Published: 22 Dec 2023
Citation: Sarr S Antoine, Keita Fatoumata, Aw Fatou, et al. Knowledge of Direct Oral Anticoagulants (DOACS) and Limits of Their Prescription: Survey of Cardiologists, Intensivists, Neurologists and Pulmonologists in Senegal. Cardiol Vasc Res. 2023; 7(6): 1-4.
Abstract
Introduction: Direct oral anticoagulants (DOACs) constitute a first-line therapy in non-valvular atrial fibrillation and venous thromboembolic disease. The aim of this study was to evaluate the prescription of DOACs among cardiologists, neurologists, intensivists and pulmonologists.
Patients and Methods: We conducted a cross-sectional, descriptive study from June 1, 2023 to July 1, 2023, a period of one month. All cardiologists, neurologists, intensivists and pulmonologists who agreed to participate in the study were included. The parameters studied were related to the characteristics of the population, to knowledge and also DOACs prescribing. Data were collected using a pre-established survey questionnaire in paper and electronic format via Google form.
Results: We included 218 subjects. Cardiologists were more represented (70.48%). The majority of specialists (70.77%) had between 0 and 5 years of experience. Among the subjects included, 33% claimed to have never had formal training about DOACs. The need for additional training was strongly expressed (85%).
We found that 95% prescribed DOACs. The monthly frequency prescription was most often 1 to 2 times (40%). More than 3 out of 10 specialists prescribed DOACs for atrial fibrillation, pulmonary embolism and other situations. The reasons for replacing an AVK with a DOAC were dominated by the problem of compliance with VKAs and the absence of INR control using DOACs (54.7%). The reasons for replacing a DOAC with a VKA were dominated by the high cost of DOAC treatment (77.5%). The limitations of prescribing DOACs were dominated by the high monthly cost (66%), patient preference (14%), and specialist distrust of DOACs (6%). Concerning the compared cost of DOACs versus VKA, 33% of the population considered the cost of DOACs treatment equivalent to that of the overall cost of VKA treatment. Most specialists (99%) stated that their patients were satisfied with DOAC treatment.
Conclusion: Direct oral anticoagulants (DOACs) are underused in Senegal due to their high cost but also due to lack of awareness linked to insufficient continuing training.
Keywords
Introduction
Anticoagulants have become essential drugs in medical practice. After the discovery of heparin and vitamin K antagonists a century ago, that of direct oral anticoagulants, around twenty years ago, constituted a considerable advance [1,2]. Their marketing for around ten years has been motivated by the promise of an improvement in the patient's quality of life, a reduction in morbidity and mortality and at least equivalent effectiveness than VKAs [3-6]. Currently, direct oral anticoagulants are represented by a direct anti-IIa antithrombin: dabigatran and by several direct anti- Xa: rivaroxaban, apixaban, edoxaban in addition to Bétrixaban currently under development [7]. DOACs constitute a first-line treatment to prevent stroke in non-valvular atrial fibrillation and in the treatment of venous thromboembolic disease. Despite all these indications, safety of use and better quality of life, the prescription of DOACs does not seem optimal [8]. In Africa, the problem of cost adds to these reluctances and constitues an additional obstacle. In Senegal only rivaroxaban has been available since 2014. In a study focusing on atrial fibrillation in 2017, DOACs were only used in 0.59% of cases. The same observation was made regarding venous thromboembolism in 2021, DOACs were only prescribed in 14% of cases [9]. It was in this context that we carried out this survey, the aim of which was to assess the prescribing of AODs among cardiologists, neurologists, intensivists and pulmonologists.
Patients and Methods
To achieve this objective, we conducted a cross-sectional, descriptive study from June 01, 2023 to July 01, 2023. The study population consisted of cardiologists, intensivists, neurologists and pulmonologists. All public and private practitioners who agreed to take part in the study were included. The parameters studied were related to the characteristics of our study population (distribution according to specialty, place of practice, number of years of experience), to knowledge of DOACs (training received, monthly cost compared with VKAs, existence of antidotes) and also to DOACs prescribing (monthly frequency, change of anticoagulant, prescription limits). Data were collected using a pre-established survey questionnaire in paper and electronic format via Google form. Data were entered and analyzed using Excel 2013 software. They were presented in percentages and illustrated in the form of histograms, pie charts and tables.
Results
A total of 218 subjects were included, the majority of whom were public practitioners (87.4%). Cardiologists were more represented (70.5%). Neurologists, pulmonologists and intensivists accounted for 4.3%, 8% and 17.2% respectively. The majority of specialists (70.8%) had between 0 and 5 years' experience. Those with more than 20 years' experience accounted for 4% of the study population. In addition, there were two (02) specialists with over 25 years' experience. Regarding training received in DOACs, 33% of the subjects stated that they had never had any formal training.
Whatever the specialty, the need for additional training was strongly expressed (85%). We found that 204 specialists (95%) prescribed DOACs. The monthly frequency of prescription was most often 1 to 2 times (40%) (Figure 1).
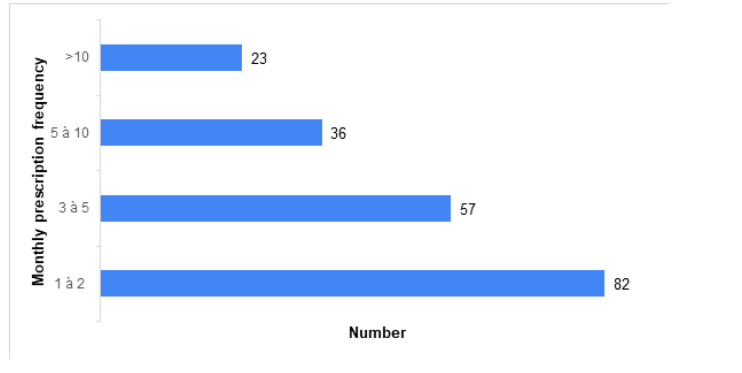
Figure 1: Monthly prescription frequency of DAOCs in our population.
More than 3 out of 10 specialists (34%) prescribed DOACs for atrial fibrillation, pulmonary embolism and other conditions (venous thrombosis, prevention of thromboembolic events); 19,5 prescribed it only for pulmonary embolism). A total of 155 specialists (75%) said they had already replaced VKA with DOAC. Reasons were given in 75% of cases. They were dominated by compliance problems with VKAs and lack of INR control when using DOACs (54.7%) (Figure 2).
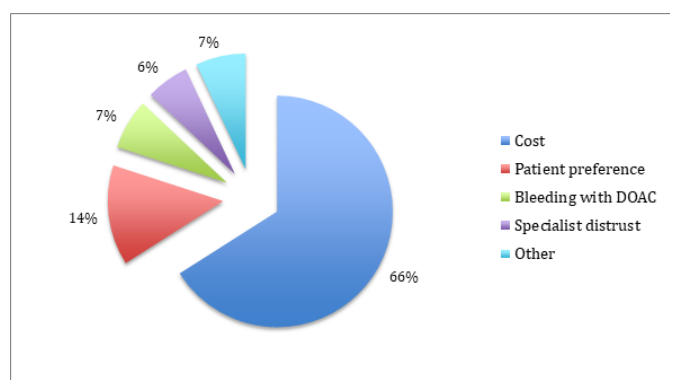
Figure 2: Reasons for replacing VKA for DOACs.
In a other hand, 116 specialists (56.6%) had already replaced a DOAC with a VKA. The reasons were dominated by the high cost of DOACs treatment (77.5%), thromboembolic complications (6.25%) and bleeding events due to DOACs (6.25%). Limitations to DOACs prescription were dominated by high monthly cost (66%), followed by patient preference (14%) and specialist distrust (6%) (Figure 3).
Regarding the cost DOACs versus VKAs, 33% judged the overall treatment costs to be equivalent. On the other hand, 29 others (14%) felt that the cost of DOACs treatment was five times higher than that of VKA treatment (Table 1).
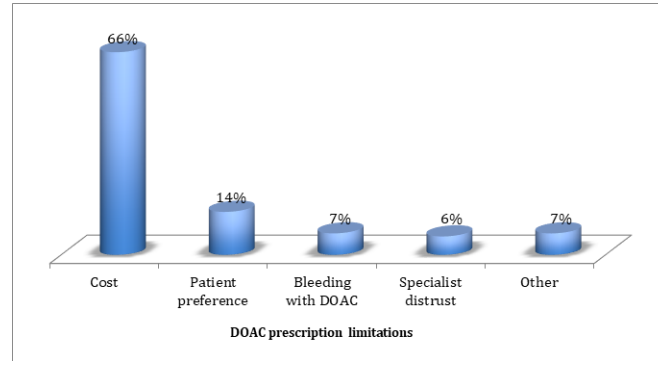
Figure 3: DOACs prescription limitations.
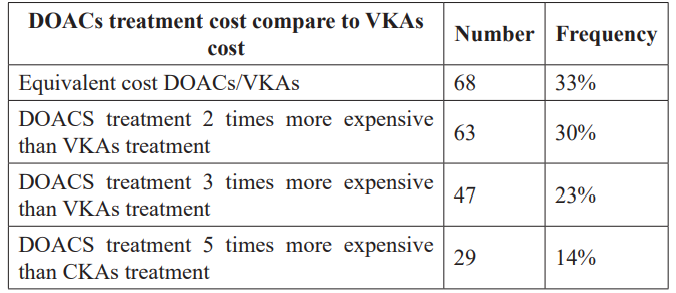
Table 1: DOACs treatment cost compared to VKAs treatment according to our study population.
Au total of 99% of specialists said that their patients were satisfied of the treatment in terms of antidote knowledge, 54.02% stated that antidotes for DOACs existed.
Comments
Our sample was dominated by cardiologists. They are supposed to be the main prescribers of DOACs. However, their predominance may have constituted a bias in this study.
We found insufficient training on DOACs and a need for additional information. This could be linked to the fact that there is no continuing training program for doctors in Senegal like, for example, in France. In fact, it has become compulsory in France since the 2016 health system modernization law dedicated to health professionals. Law n°2016-41 of January 26, 2016 of the public health code, article L. 4021-1 of which states that “Continuing professional development (CPD) aims to maintain and update knowledge and skills as well as improving practices. It constitutes an obligation for health professionals”[10].
In our results, we reported a low frequency of prescription of DOACs (1 to 2 times in 40% of cases). Previous studies showed the use of direct oral anticoagulants (DOACs) in less than 1% of cases in atrial fibrillation and 14% in venous thromboembolism [9].
The limitations of prescribing DOACs were dominated by the high monthly cost. In fact, the monthly cost of DOACs treatment in Senegal is 53 euros that means 50% of the minimum wage. However, as in many countries in sub-Saharan Africa, few people have health insurance. In addition, when comparing the direct cost of AVK and AOD, there is a strong difference. In Uganda, for example, a 5 mg tablet of warfarin costs about $0.2, which is significantly less than the $2 to $4 needed to buy a 15 mg tablet of rivaroxaban [11]. However, this aspect should be qualified for several reasons. The first is that VKA requires frequent measurement of the INR, which constitutes an additional cost as well as hospitalization costs, medical costs for review of treatment or management of side effects. As a result, some studies have even shown almost identical costs or even in favor of DOACs. A recent Pouvourville study which compared the cost-effectiveness ratio between the four DOACs and VKAs showed that DOACs are in fact less expensive than VKAs, apart from rivaroxaban which remains the most expensive (below €20,000 per Quality-Adjusted Life Year (QALY) for VKAs. Apixaban and dabigatran at a dose of 150 mg presented the most favorable ratios [12]. The second reason is the quality of anticoagulation with VKAs evaluated by the “time in therapeutic range” (TTR). As examples, the TTR of patients treated on an outpatient cohort for non-valvular atrial fibrillation at the Abidjan Cardiology Institute (ICA), and in the Cameroonian cardiological environment revealed averages of 44.1% and 52% respectively. Therefore less than 60% corresponding to inadequate anticoagulation and/or the occurrence of an ischemic or hemorrhagic event [13,14]. All this should encourage the prescription of DOACs in our conditions. Especially since in practice, measuring the INR is only possible in large cities. In the years to come, these drugs will potentially be produced in generic form at a cost much lower than today. This will most likely have a significant impact on the prescription of DOACs, especially since their widely proven safety and effectiveness place them in the front line in the treatment of atrial fibrillation and venous thomboembolic disease [3,15-17].
Conclusion
DOACs are insufficiently known among some doctors in Senegal. This, in addition to their high cost, constitutes the main obstacles to their prescription. Continuing education and cost reduction could allow patients to benefit from these drugs, which are on the front line of treatment of atrial fibrillation and venous thromboembolism.
References
- Handin The History of Antithrombotic Therapy: The Discovery of Heparin, the Vitamin K Antagonists, and the Utility of Aspirin. Hematol Oncol Clin North Am. 2016; 30: 987-993.
- Wardrop D, Keeling The story of the discovery of heparin and warfarin. Br J Haematol. 2008; 141: 757-763.
- Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised Lancet Lond Engl. 2014; 383: 955-962.
- https://www.ansm.sante.fr/Dossiers/Les-anticoagulants/Les-anticoagulants-en- France-Etudes-et-surveillance/(offset)/0
- Feuring M, Schulman S, Eriksson H, et Net clinical benefit of dabigatran vs. warfarin in venous thromboembolism: analyses from RE-COVER, RE-COVER II and Re-MEDY. J Thromb Thrombolysis. 2017; 43: 484-489.
- Kaymaz EINSTEIN CHOICE: Comparison of rivaroxaban treatment and prophylactic doses with aspirin in the extended treatment of patients with venous thromboembolism. Turk Kardiyol Dernegi Arsivi Turk Kardiyol Derneginin Yayin Organidir. 2017; 45: 1-7.
- Sylvester KW, Connors JM. Betrixaban in the prevention of venous thromboembolism in medically ill patients. Future 2018.
- https://www.ameli.fr/l-assurance-maladie/statistiques-et-publications/donnees-statistiques/medicament/medic-am/ medic-am-mensuel-2018.php
- https://www.legifrance.gouv.fr/loda/id/JORFTEXT000031912641
- Semakula JR, Mouton JP, Jorgensen A, et A cross-sectional evaluation of five warfarin anticoagulation services in Uganda and South Africa. PLoS One. 2020; 15: 1-9.
- Freeman JV, Zhu RP, Owens DK, et al. Cost-effectiveness of dabigatran compared with warfarin for stroke prevention in atrial Ann Intern Med. 2011; 154: 1-11.
- Pouvourville Cost effectiveness of direct oral anticoagulants: a literature overview in European. Archves of Cardiovascular Diseases Supplements. 2016; 8: 180-191.
- Coulibaly I, Diatema S, Hauhouot-Attoungbre ML. Qualité de l’anticoagulation orale par antivitamine K évaluée par le calcul du TTR chez des patients traités en ambulatoire pour fibrillation auriculaire non valvulaire (FANV) à l’Institut de Cardiologie d’Abidjan (ICA). Cardiologie Tropicale. 2018;
- Nganou-Gnindjio CN, Tchapmi D, Sadeu Wafeu G, et Evaluation de la qualité de l’anticoagulation par les antivitamines K en milieu cardiologique camerounais : étude longitudinale prospective. Cardiologie Tropicale. 2021; 163.
- Maura G, Billionnet C, Alla F, et Comparaison of Treatment Persistence with Dabigatran or Rivaroxaban versus Vitamin K Antagonist Oral Anticoagulants in Atrial Fibrillation Patients: A Competing Risk Analysis in the French National Health Care Databases. Pharmacother J Hum Pharmacol Drug Ther. 2018; 38: 6-18.
- Zhou Y, Yao Z, Zhu L, et al. Safety of Dabigatran as an Anticoagulant: A Systematic Review and Meta-Analysis. Front 2021; 12: 6260-6263.
- Touma L, Filion KB, Atallah R, et al. A meta-analysis of randomized controlled trials of the risk of bleeding with apixaban versus vitamin K antagonists. Am J Cardiol. 2015; 115: 533-541.