Laparoscopic Diagnosed Fallopian Tube Rupture during Expectant with Negative Urine Pregnancy Test
Author'(s):Sachino Kira*, Naho Tokunaga, Koki Yagi, Naoki Abe, Mariko Matsuno, Sotaro Hayashi, Miho Oda,Hajime Takeuchi, Lifa Lee, Yoko To, Satoshi Nishiyama, Maki Goto and Hiroshi Tsujioka
Department of Obstetrics and Gynecology, Aso Iizuka Hospital,83-3 Yoshio-machi, Iizuka, Fukuoka, Japan.
*Correspondence:
Sachino Kira, 83-3 Yoshio-machi, Iizuka, Fukuoka, Japan 820-8505, Tel: +81-948-22-3800, Fax: +81-948-29-8457.
Received: 15 Jul 2023; Accepted: 20 Aug 2023; Published: 27 Aug 2023
Citation: Kira S, Tokunaga N, Yagi K, et al. Laparoscopic Diagnosed Fallopian Tube Rupture during Expectant with Negative Urine Pregnancy Test. Addict Res. 2023; 7(1): 1-3.
Abstract
In cases of ectopic pregnancy during expectant management, follow-up is usually performed until the urine pregnancy test is negative. We encountered a case of rupture from a tubal pregnancy during expectant management, despite a negative pregnancy test. We recommend monitoring serum human chorionic gonadotropin level until it falls below the sensitivity.
Keywords
Introduction
Ectopic pregnancy raptures are the leading cause of maternal mortality within the first trimester of pregnancy. The current standard for diagnostics includes transvaginal ultrasound imaging and human chorionic gonadotropin (hCG) level monitoring [1]. Due to high-quality ultrasound diagnosis in recent years, early diagnosis may prevent rapture, allowing patients to choose nonsurgical options [2]. Generally, the patients with initially low level and decreasing of hCG can be considered for expectant management [1]. It should be monitored until serum hCG<20mIU/ mL or the pregnancy test is negative [3]. However, we encountered a case of rupture from a tubal pregnancy during expectant management, despite a negative pregnancy test. We recommend monitoring serum human chorionic gonadotropin level until it falls below the sensitivity, together with regular follow-up including transvaginal ultrasound, until the ectopic tissues have completely disappeared.
Case Report
A 33-year-old, gravida3, para1 (cesarean section) female presented to the emergency department with a 3-day history of severe abdominal pain. The patient had a medical history of cesarean section, artificial abortion, and hysteroscopic endometrial polypectomy
Five weeks after her last menstrual period, the patient did a pregnancy test, which was positive, and she subsequently visited a gynecology clinic. During the gynecological consult, a gestational sac could not be found in the uterus, transvaginal ultrasonography revealed a thin endometrium with no evidence of an adnexal mass, and the serum hCG level was 1625 mIU/mL. Since the hCG level had decreased by the next day, an ectopic pregnancy was suspected. As the patient had no pain or vaginal bleeding, she was observed for expectant management as outpatient. As expected, serum hCG levels continued to decline for four weeks. Three days before presentation to the emergency department, sudden onset of lower abdominal pain started during sexual activity and persisted at intervals thereafter. The pain had been progressively worsening; therefore, she called an ambulance.
On clinical examination, she was pale, with a pulse rate of 68 beats per min and a blood pressure of 100/68 mmHg. Her lower abdomen was soft, tender, and showed diffuse rebound tenderness. Urinary pregnancy test results were negative and her hemoglobin level was 11.8 mg/dL. Computed tomography (CT) of the abdomen and pelvis with intravenous contrast showed active bleeding with linear contrast extravasation from the mass in the right uterine region. Ovarian bleeding was suspected, once the patient was admitted to our department for follow-up. A few hours later, the blood pressure had dropped to 79/52mmHg, and hemoglobin level to 7.9mg/dl, thus the patient was taken to the theater for an urgent laparotomy.
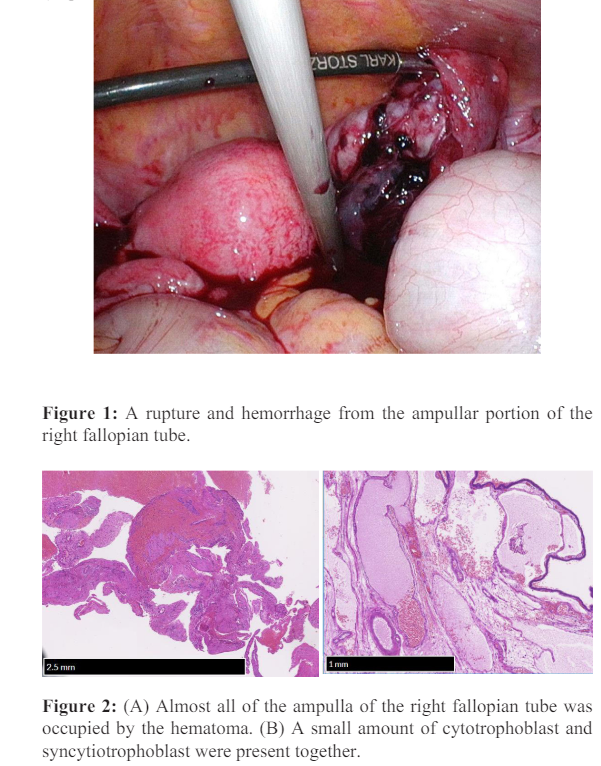
An acute laparotomy revealed approximately 600 mL of blood in the upper abdominal and peritoneal cavities. There was a rupture and minimal active bleeding from the ampulla of the right fallopian tube (Figure 1). The uterus was almost normal in size. The fimbria of the left tube was apparently patent and intact. Bilateral ovaries were normal in size. There were fine adhesions in ascending colon to peritoneum. Right salpingectomy was performed, the bleeding stopped, and the patient's condition became hemodynamically stable. The serum hCG level was measured during surgery and found to be 28 mIU/mL. Her hemoglobin level decreased to 5.4 mg/dL, and thus, transfusions were administered to compensate for the hemorrhage from the rupture. The patient's immediate postoperative condition was satisfactory. Villus tissue was not clear macroscopically in extracted right fallopian tube, and right tubal pregnancy was confirmed by histopathological examination (Figure 2A and B).
Discussion
We encountered a case of a ruptured ectopic pregnancy with a negative urine pregnancy test result. During expectant management, fallopian tube rupture may occur even if the urine pregnancy test result is negative [3].
The urine pregnancy test is useful because it takes only a few minutes to obtain the results. This is particularly useful in cases of hemodynamically unstable women of reproductive age with gross abdominal bleeding [5,6]. However, the urine pregnancy test is not always reliable because it cannot detect below 25 mIU/ mL of hCG. Up to 1% of ectopic pregnancies are associated with hCG values of 20 mIU/mL or less, a threshold which is below the detection limit of most urine hCG assays. In addition, urine hCG tests may yield false negative results in dilute urine samples. Certain drugs, such as diuretics and promethazine, may also cause false-negative urine results; therefore, these tests should be used with caution [7]. Clinically stable women, with no abdominal pain or evidence of significant hemoperitoneum on ultrasound, with an ectopic pregnancy measuring <30 mm in mean diameter, no evidence of embryonic cardiac activity, and low initial serum hCG (<1500 mIU/mL) could be candidates for expectant management. In clinical practice, this protocol significantly reduces the need for surgical or medical treatment of ectopic pregnancies. It recommends outpatient follow-up until serum hCG levels become lower than 20 mIU/mL or a negative urine pregnancy test result [3]. However, in cases of tubal miscarriage, trophoblasts undergo degenerative changes that increase vascularity and tissue edema. Neutrophils and macrophages are recruited to aborted tissues, causing inflammation and tissue fragility [8]. The hematoma may grow even after the trophoblast tissues have almost disappeared during the miscarriage. The fallopian tubes have no elastic myometrium; thus, in such cases, tubal rupture may occur once the tubal ectopic mass grows beyond a certain limit [9]. It is important to follow up until ectopic tissues and/or hematomas completely disappear.
Conclusions
If the urine pregnancy test result is negative, it is important to consider the possibility of ectopic pregnancy in cases of acute abdominal pain with genital bleeding in women of reproductive age. During expectant management, fallopian tube rupture may occur even if the urine pregnancy test result is negative. We recommend monitoring the serum hCG level until it falls below sensitivity, together with regular follow-up including transvaginal ultrasound, until the ectopic tissues and/or hematoma have completely disappeared.
Acknowledgment
We would like to thank Editage (www.editage.com) for English language editing.
References
- Mullany K, Minneci M, Monjazeb R, et al. Overview of ectopic pregnancy diagnosis management and Womens Health Lond. 2023;
- Kirk E, Papageorghiou AT, Condous G, et al. The diagnostic effectiveness of an initial transvaginal scan in detecting ectopic pregnancy. Hum Reprod. 2007; 22:
- Mavrelos D, Nicks H, Jamil A, et al. Efficacy and safety of a clinical protocol for expectant management of selected women diagnosed with a tubal ectopic pregnancy. Ultrasound Obstet Gynecol. 2013; 42:
- Hughes M, Lupo A, Browning A. Ruptured ectopic pregnancy with a negative urine pregnancy test. Proc Bayl Univ Med Cent. 2017; 30:
- Tonick S, Conageski C. Ectopic pregnancy. Obstet Gynecol Clin North Am. 2022; 49:
- Belics Z, Gerecz B, Csakany MG. Early diagnosis of ectopic pregnancy. Orv Hetil. 2014; 155:
- Montagnana M, Trenti T, Aloe R, et al. Human chorionic gonadotropin in pregnancy diagnostics. Clin Chim 2011; 412:
- Christiansen OB, Nielsen HS, Kolte AM. Inflammation and miscarriage. Semin Fetal Neonatal Med. 2006; 11:
- Shabbir U, Anwar J, Asghar MS, et al. A ruptured seventeen weeks ectopic pregnancy A case report. J Pak Med 2021; 71: 763-765.