Laterality of Colorectal Cancer (CRC) in Oman
Author'(s): Bassim Jaffar Al Bahrani, Itrat Mehdi*, Essam Abdul Monem, AbdulAziz Majid Al Farsi, Najla Al Lawati and Ayman Mohammed Nada
Department of Medical Oncology, National Oncology Centre,the Royal Hospital, Muscat, Sultanate of Oman.
*Correspondence:
Itrat Mehdi, Senior Consultant, Department of Medical Oncology, National Oncology Centre, the Royal Hospital, Muscat, Sultanate of Oman, Tel: +968 92756105, Fax: + 968 24627003.
Received: 27 November 2020; Accepted: 02 January 2021
Citation: Al Bahrani B, Mehdi I, Monem EA, et al. Laterality of Colorectal Cancer (CRC) in Oman. Cancer Sci Res. 2021; 4(1): 1-7.
Abstract
Introduction: Colorectal cancer (CRC) is the first most predominant malignancy in men, a bit less 3rd commonest in women. The prevalence rate is higher in developed than in developing economies, though the pattern is gradually changing. In Oman, CRC prevalence rate has shown a significant escalating pattern in the recent past. From 1996 to 2012, CRC incidence in Oman has increased by 282% in females and 386% in males. There is emerging data that
right and left sided lesions are different in terms of aetiology, pathogenesis, biologic behaviour, genetic makeup, response to treatment and outcome. This study has looked at this issue in the Omani population of CRC.
Methods: Eligible CRC patients treated at the Royal Hospital were identified from electronic medical record (Al-SHIFA 3) and Oman cancer registry data base (Ministry of Health) from 1998-2013. The BMI (body mass index), age, gender, stage, tumour location, K-Ras status, and Diabetes mellitus (DM) were explored. The RAS mutation status test (mutant type MT or wild type WT) was carried out in Lab21. Log regression was conducted to estimate the association between food intake, BMI, presence of metabolic syndrome, and level of physical activity with both cancers. Data was analysed using the SPSS.
Results: Total number of patients treated at Royal Hospital were 492, 193 females (44%) and 214 males (56%). About 71.9% of patients were less than 60 years of age. The obese and overweight patients were 201 (57.3%). The rectum was found to be the predominant site of the tumor. The left sided tumors were significantly higher, 4 out of every 5 tumors (80.3% Vs 16.4%). The patients with right sided CRC were slightly younger, had a higher BMI, and more likely to be diabetic. The tumors of the left colon are more K-ras wild while those of the right colon are more K-ras mutant.
Conclusions and Discussion: The right sided tumors as per our study are younger; with significant obesity, diabetes, and K-Ras mutant, and this correlates with high meat and protein consumption in the Omani population. The sidedness or laterality of CRC needs further study in Oman. There is emerging data that right and left-sided lesions are different in terms of etiology, pathogenesis, biologic behaviour, genetic makeup, response to treatment and outcome.
Keywords
Introduction
Colorectal cancer (CRC) is a foremost global health concern and remains one of the major causes of cancer-related morbidity and mortality in both the developed and developing countries [1-4]. CRC is the first most predominant malignancy in men, a bit less in women ranking 3rd [5]. The prevalence rate is higher in developed than in developing economies, though the pattern is gradually changing. The trend and frequency for CRC from the advanced nations have been accounted for in most studies, and there is a scarcity of such information from the Arab world [6]. Very few studies have been conducted in Oman till date [20,25].
In Oman, CRC prevalence rate has shown a significant escalating pattern in recent past [6]. CRC is the second most predominant cancer among men and fourth most ubiquitous among women in Oman, with a significantly rising management cost [20]. The current data show that Oman has a higher incidence of CRC in the Gulf region even though they have a common culture and life style. The age-adjusted annual incidence of cancer ranges from 70-110 per 100 000 populations [6]. According to the Globocan report, the estimated number of new cancers cases in Oman in 2020 will be 2451 cases and 2030 it will increase to 3792 new cancer cases [5]. In 2012, the country recorded 116 new CRC cases for both men and women. The yearly age-standardized incidence rate was 10.2 and 8.5 per 100000 for men and women. From 1996 to 2012, CRC incidence in Oman has increased by 386% in males and 282% in females [6,7].
The risk factors for CRC are adaptable, and incorporate consumption of red meat, food rich in saturated fats and obesity [3]. As an after effect of the lifestyle variability, there is a considerable difference in frequency and mortality from CRC all over the globe [5]. The Omani population has definite dietary and environmental variation, are often overweight, and incidence of diabetes mellitus is significantly higher [7-9]. The role of RAS/ RAF mutation is well established in carcinogenesis of CRC. RAS mutations are identified in up to 36% of colorectal cancers. RAS testing is now the standard of care being recommended by all international guidelines. These mutations define treatment response to anti-EGFR agents, and prognosis by predicting tumour recurrence [7,9].
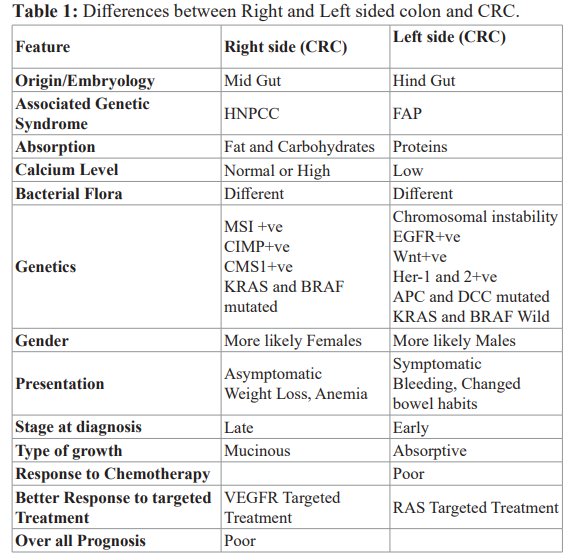
There are increasingly appreciated differences between right and left-sided colon [10]. Right and left colon has distinct embryologic development and physiologic functions. CRC, on the left or right side, are different in terms of etiology (diet related), clinical feature, molecular biology and genetic features [11]. The embryological development of the large bowel is different. The right sided colon is derived from midgut while the left sided colon is derived from hindgut. The midgut eventually develops into distal duodenum, jejunum, ileum, caecum, appendix, ascending colon, and proximal two thirds of the transverse colon. The hindgut develops into the distal third of the transverse colon, the sigmoid colon, rectum, and upper two thirds of the anal canal [12]. There is higher concentration/absorption of protein on left side colon while that of fat and carbohydrate on right side [13]. The calcium levels are low in the left colon. The bacterial flora is different between left and right side [14]. The left sides tumours are more male while right-sided are more females. Right-sided CRC are more likely mucinous while left-sided are more absorptive [15-16]. Left-sided tumours are often associated with FAP (familial Adenomatous polyposis), while that of the right side with HNPCC (hereditary non-polyposis colorectal cancer). Left-sided CRC shows chromosomal instability, EGFR and Wnt Positive, and Her-1/Her- 2 amplification. Left-sided CRC also shows mutations in APC, K-ras, DCC, and p53. The right-sided CRC are more MSI +ve, CIMP+ve, CMS1 +ve, CMS3 +ve, and BRAF mutated with active MAPK signalling pathway (Table 1). The mutagenic metabolites of CYP450 are seen more on the right side [11,15,17].
The gene which decides the localization or laterality of an organ (left or right) is called LEFTy [18]. We are now aware of increasing differences in the molecular pathology of carcinomas depending on their laterality within the large bowel. These differences will become more relevant as systemic treatments improve. Microsatellite instability is significantly more common in right- sided bowel cancers, 20% of right-sided and 1% of left-sided bowel cancers. K-ras mutations may also be more common in proximal tumors. Sporadic right-sided colorectal cancers showing microsatellite instability may have lower levels of other factors such as vascular endothelial growth factor, and mutant p53. In contrast, left-sided bowel or rectal cancers are more likely to show features including aneuploidy, loss of heterozygosity, overexpression of vascular endothelial growth factor, and mutations in genes from the Vogelstein model including p53 [15,21,23].
Differences in clinical presentation and surgical management of right and left-sided large bowel cancer are well known [16]. For example, right-sided tumours typically present at a more advanced stage with symptoms of weight loss and anaemia, whereas left- sided tumors often present with rectal bleeding, change in bowel habit, and tenesmus. The reported treatment responses and survival between left and right-sided tumours is different as well. Right- sided tumors have poor prognosis [11,17]. In Japan, the right- sided CC is more prevalent, diagnosed at a late stage, and have flat growths while left-sided are more polypoidal [10]. Mortality rate of 5 years is usually not much different, except right sided CRC in stage II/III has higher mortality [16]. Tumors showing microsatellite instability have an improved prognosis. The good prognosis of these predominantly right-sided cancers may be offset by the fact that they tend to present at a later stage. Microsatellite instability predicts a benefit from adjuvant chemotherapy, particularly in right-sided tumors.
In contrast, the features seen predominantly in left-sided cancers such as mutant p53, and overexpression of vascular endothelial growth factor are associated with an adverse prognosis and poor response to fluorouracil based chemotherapy. New targeted treatments, such as VEGF antibodies, may be appropriate for these tumours. Newer agents such as irinotecan and Oxaliplatin may also show differing responses dependent on the site of disease or molecular pathology. In the future, both the primary site and genetic features of an individual cancer may determine the systemic treatment [12].
Patients and Methods
An ethical approval from the Royal Hospital scientific and ethical committee was taken, and the study was conducted after this approval. Eligible Colorectal patients treated at the Royal Hospital were identified from Royal Hospital electronic medical record (Al-SHIFA 3) and Oman cancer registry data base (Ministry of Health) from 1998-2013. National Oncology centre (NOC) is the only comprehensive Oncology centre in Oman; more than 70% of all newly diagnosed patients are treated at NOC. We included even those patients who developed a recurrence or death shortly after their original diagnosis of colorectal cancer.
The BMI (body mass index) was used as measures of obesity. Patients must have had their baseline height and weight prospectively recorded at their initial consultation visit before any treatment offered (systemic chemotherapy or radiation therapy). BMI was calculated as the patient’s weight (in kilograms) divided by the patient’s height squared (in square meters). Patients were subsequently assigned to four BMI categories: Underweight <18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (>30 kg/m2). In addition to the BMI, the following variates were analysed: Age, Gender, Stage, tumour location, K-Ras status, and Diabetes mellitus (DM).
The RAS mutation status tests were carried out in Lab21, the United Kingdom as per arrangements with the pathology department. Patients with mutations will be considered as mutant type (MT), and with no detectable mutations will be regarded as wild type (WT).
Multiple regression analysis carried out to examine which risk factors predicted colorectal cancer. Logistic regression was conducted to estimate the association between food intake, BMI, presence of metabolic syndrome, and level of physical activity with both cancers. Data was analysed using the SPSS Statistics Version 20.
Results
The total number of patients treated at the Royal Hospital from 2000 to 2013 was 492. There were 193 females (44%) and 214 males (56%). BMI was available for 351 patients, 158 were female and 193 were male. There were 92.2% Omani nationals. About 71.9% of patients were less than 60 years of age.
The number of underweight patients was 19 (5.4%) and normal as 131 (37.3%). The number of overweight patients was 118 (33.6%) and obese was 83 (23.7%).
The total number of underweight plus normal weight was 150 (42.7%), and with obesity plus overweight were 201 (57.3%). Stage I, II, III and IV in underweight plus normal weight were 5.3%, 15.3%, 34.7% and 38.7%. Stage I, II, III and IV in overweight plus obese were 8%, 18.9%, 39.3% and 25.8% respectively.
Table 2 and 3 shows the morphologic site of a tumor. The rectum was found to be the most predominant site of a tumor. Left-sided tumors are significantly higher at almost 4 out of every 5 tumors.

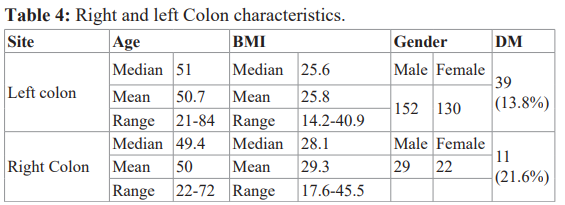
Table 4 and 5 shows the correlation of age, BMI, gender, obesity, diabetes mellitus, and K-ras status concerning right and left -sided tumors. The patients with right sided colorectal tumors were slightly younger, had a higher BMI, and more likely to be diabetic. The right-sided tumours are more obese. The tumors of the left colon are more K-ras wild while that of the right colon is more K-ras mutant.

Discussion
Oman is the 2nd largest country by area in the GCC region, having a population of about 4.5 million as reported in 2016. Oman has a relatively young population with only 6% population being over the age of 60 years. The life expectancy in Oman is increasing over a while, being reported as 73 years in 2010. Cancer is the 3rd leading cause of death in Oman. The median age diagnosis of cancer in Oman is reported as 55 years, 60 years for male and 49.5 years in females. The cases of colorectal cancers reported from our study are 14.5% over the age of 65 years while 78.1% are between 30 and 65 years of age. The CRC cases under 49 years of age are 44.8% [6,25]. The reported age at diagnosis is younger in CRC in Oman than reported from the Kingdom of Saudi Arabia (KSA), Egypt, Iran, Malaysia and Pakistan but older than that reported from United Arab Emirates [19-20]. The young age at diagnosis in CRC is also seen and reported among other cancers in Oman, consistent with the observation from other Arab countries and most of the developing world [19,21-22]. This young presentation has clinical, prognostic, social, psychological, and economic implications which need to be analysed further [23].
The frequency and ASR of common cancers in Oman have shown a change from 1996 to 2012. The frequency of CRC, breast, thyroid and prostate has increased by 314%, 177%, 128% and 64% respectively (60). CRC incidence and mortality rates vary up to 10-times globally, with definite ascents and descents across populations and country’s development levels, directing towards broadening inequalities and a mounting burden in countries in transition. Generally, CRC incidence and mortality rates are still escalating rapidly in many low-middle income countries; while stabilizing or decreasing trends in highly developed countries where rates remain among the highest in the world [21-22]. It appears that CRC incidence is dramatically increasing in many developing countries [23] like in the former Eastern European Communist Bloc, Hong Kong, Taiwan, urban China, Singapore, Iran, Saudi Arabia, Jordan, Yemen and Egypt [24].
Early detection, improved treatment, and lifestyle changes such as diet and exercise modification have contributed to these changes [25]. The greatest increases in the incidence of CRC are in Asia related to the increasing prevalence of obesity. The decrease in CRC incidence in the United States partially reflects the increase in detection and removal of precancerous lesions; while the increase in several Asian and Eastern European countries may reflect changes in risk factors for colorectal cancer that are associated with westernization such as elevated obesity and smoking. The data from GCC suggest that CRC incidence continues to increase [20]. Numerous environmental risk factors, principally changes in diet and life style, are proposed to trigger the rise of CRC in these populations [21,23-24].
The stage information wherever available in our study showed stage I, II, III and IV as 7.4%, 18.7%, 40.2% and 33.7% respectively. The localized disease (stage I and II) was 26.1%, while advanced and metastatic disease (stage III and IV) was 73.9%. The advanced stage at presentation (stage III 42.6% and stage IV 32.7%) is similar to data published from Egypt, KSA and Jordan but different from the data published from Western Europe and North America [2,5,16,21]. The early stage at presentation from the Western World reflects their successful screening programs [7]. The ratio of mortality to incidence rates in different regions varies from 30.2%, 45%, 69% and 78% in America, Europe, South East Asia and Africa respectively [28]. The data from GCC suggest that advanced colorectal cancer was present in 60%, while localized tumors were present only in 20% [20].
Numerous environmental risk factors, principally changes in diet and lifestyle, are proposed to trigger the rise of CRC [21,23]. Diet and lifestyle impact on nuclear receptors, on the intestinal microflora and critical molecular pathways incriminated in intestinal carcinogenesis. This epidemiological transition globally offers a unique opportunity to better understand CRC carcinogenesis by exploring the disease phenotypes and their environmental and molecular associations in these different geographic and economically distinct populations [2,4]. The information from these studies may have important implications for the global screening, prevention, and diagnostic and management strategy of CRC [20,21,23,25].
Our study indicates BMI variation in Oman, the highest median BMI as 27.8 and the lowest median BMI 21.8. Obesity has turned epidemic globally in the last few decades and CRC-obesity relationship is reinforced by the importance of nutrition in CRC. CRC has been associated with red and processed meat intake, high- carbohydrate intake, and high-sugar content beverages. Obesity sets in mutagenesis, metabolic dysregulation, and exaggerated inflammatory responses facilitating pathogenesis of CRC [26-27]. Diet in CRC may increase the risk of recurrence and mortality after initial diagnosis. Obese patients appear to have worse overall survival with CRC. In a recent study, BMI is identified as an independent predictor for overall survival dealing with overweight and obese patients with mCRC treated with Bevacizumab [8].
About 17.4% of CRC patients had DM all CRC cases, in this analysis. In another analysis, DM in CRC patients in Oman is reported as high as 24.7% [7]. The age-adjusted prevalence of T2DM in Oman varied from 10.4% to 21.1% (24). CRC risk is higher (1.3 fold) in patients having type 2 DM [12,27], either proximal or distal, in both males and females. Diabetic patients over 50 years of age should be counselled regarding their elevated risk for CRC, and screening colonoscopy can be recommended. There is strong evidence to indicate that DM is a causal agent for CRC development and it provides new impetus for re-evaluating CRC screening worldwide [8,28].
The morphologic distribution of CRC reported from Europe and UK is: Right colon 23% males and 32% females, Left colon 26% males and 25% females, and rectum 32% males and 23% females [29]. One analysis from the US showed 70% left-sided CRC with a better survival [17]. In another study from the USA, the distribution of right colon, left colon and rectum were 42%, 23% and 28% respectively [27]. An Indian study found 21% CRC in right and 7% in left colon [30]. In another study from Oman, it was reported as right colon (21%), left colon (17.9%), and rectum (29.6%) [7]. From our study data, most CRC tumors are left-sided (80% Vs 14.6 %,). The rectum is the commonest site representing 36.1% (126 cases), followed by sigmoid 26.2%, while caecum and transverse colon were lowest at 6.3% each (22 cases.). The right- sided tumors as per our study are younger; with significant obesity (74.5% Vs 54.3% are obese). The right-sided tumors are more diabetic (21.6% Vs 13.8%). The left-sided tumors are more K-Ras wild (71.1% Vs 28.9%). The right sided tumours were more K-Ras mutant (41.6% Vs 15.8%). The data is consistent with high meat and Protein consumption in the Omani population.
The rectal carcinoma is different in terms of presentation, diagnostic evaluation, surgical management, neoadjuvant chemo- radiotherapy and/or adjuvant chemotherapy or radiotherapy. The outcome and relapse pattern are different as well. There is increasing appreciation of significant differences between right and left-sided colon cancers as well in terms of presentation, biological and clinical behaviour, molecular genetics, and management outcome. mCRC arising in the right or left colon are clinically different. In KRAS wild mCRC, patients with left primary tumor have a superior OS and PFS versus patients with right-sided primary tumors [10,11,13,15]. OS and PFS were prolonged with Cetuximab in left and with Bevacizumab in right-sided ones but were poorer with Cetuximab in right sided tumors. Forthcoming molecular analysis of primary tumors like BRAF, MSI, and methylation may provide a biological explanation. Stratification in mCRC studies by right vs. left sidedness is therefore indicated. These data support BV in 1st line treatment for mCRC pts with right-sided primary tumor regardless of KRAS status [31].
There are increasingly appreciated differences between right and left sided colon [11,13,18,30]. Right and left colons have distinct embryologic development and physiologic functions. CRC, on the left or right side, are different in terms of etiology (diet related), clinical feature, molecular biology and genetic features. A right-sided colon is derived from midgut while left-sided colon is derived from hindgut. There is a higher concentration/ absorption of protein on the left side colon while that of fat and carbohydrate on the right side. The calcium levels are low in the left colon. The bacterial flora is different between the left and right side. Right-sided CRC is seen in an older age group [13,15]. The left sides tumors are more male while right-sided are more females. Emergency surgery is seen more frequently in left sided CRC [15]. Right-sided CRC are more likely mucinous while left- sided are more absorptive. Left-sided tumours are often associated with FAP, while that of right side with HNPCC. Left CRC shows chromosomal instability, EGFR and Wnt Positive, and show Her- 1 and Her-2 amplification. Right-sided CRC is diagnosed at a larger size, while surgically with left-sided CRC is under staged due to the low number of lymph node retrieved [15]. Left-sided CRC show mutations in APC, K-ras, DCC, and p53. The right- sided CRC are more MSI +ve, CIMP +ve, CMS1 +ve, CMS3 +ve, and BRAF mutated (>30% vs. <5%) with active MAPK signalling pathway [32]. The mutagenic metabolites of CYP450 are more seen on the right side. The gene, which decides the localization or laterality of an organ (left or right), is called LEFTy [18].
The reported treatment responses and survival between left and right-sided tumors is different as well [33]. In the PRIME study, FOLFOX was compared with FOLFOX+Pannatumumab in 1st line mCRC. In PRIME trial OS and PFS data in RAS WT was better with Pannatumumab. OS was 30.3 vs 11.1 months and PFS was 12.9 vs 7.5 months in left and right side CRC respectively [36]. In another PEAK study, FOLFOX+Bevacizumab was compared with FOLFOX+Pannatumumab. In PEAK trial OS data in RAS WT was better with bevacizumab in left CRC (32 vs right side 21 months) while with Pannatumumab OS was 43.4 vs 17.5 months in left and right side CRC respectively [36]. Similarly, progression free survival (PFS), response rate (RR), and duration of response (DoR) were significantly better in left-sided CRC. In left-sided tumors chemotherapy plus pannatumumab was better than chemotherapy plus bevacizumab, while in right-sided tumors it was another way around. In FIRE-3 trial, FOLFRI+ cetuximab was compared with FOLFRI+ bevacizumab. In FIRE-3 OS data in RAS WT was not consistent and different, while bevacizumab OS was left CRC 28 vs right side 23 months while with Cetuximab OS was 38.3 vs 18.3 months in left and right side CRC respectively [35]. Comparing left and right-sided CRC, PFS (10.7 vs. 7.6 months), and ORR (68.8% vs. 52.6%) were better in left-sided tumors in FOLFRI + Cetuximab. The reported ORR (61.7% vs. 50%) was better in left- sided tumors in FOLFRI + bevacizumab. Bevacizumab showed better responses in right-sided CRC, while Cetuximab showed better results in left side tumors. In CRYSTAL trial, FOLFRI was compared with FOLFRI+ cetuximab. In CRYSTAL trial OS and PFS data in RAS WT was better with Cetuximab. OS was 28.7 vs 18.5 months and PFS was 12.0 vs 8.1 months in left and right side CRC respectively [37]. Comparing left and right-sided CRC, the reported ORR (72.5% vs. 42.4%) was better in left-sided tumors in FOLFRI + Cetuximab. Bevacizumab showed better responses in right-sided CRC, while Cetuximab showed better results in left side tumors. In CALGB 80405 Overall Survival OS data in RAS WT was different; bevacizumab was more effective in right-sided CRC (29.2 vs 13.6 months) while Cetuximab was more effective in left-sided CRC (39.3 vs 32.6 months). {34}. It is generally believed that right-sided CRC is more resistant to chemotherapy [17,33] and more responsive to bevacizumab. The left-sided CRC is more responsive to cetuximab and pannatumumab, and that is why they are now recommended exclusively in left-sided CRC in 2017 NCCN guidelines.
Our study of CRC patients showed 69% as RAS-WT and 31% as RAS-MT. RAS-WT were more in normal weight compared to overweight 72.9% vs. 66.1%. RAS-MT was 27.1% and 33.9% in normal weight and overweight CRC patients. The mean age for RAS-WT CRC was 46.7 years and those of RAS-MT were 67 years, indicating that WT RAS patients were relatively younger. Early (stage I+II) were more in WT-RAS 16.3% vs. 12.1%. Conversely, late stage CRC (stage III + IV) was more in MT-RAS 81.9% vs. 78.3%. RAS-WT CRC was more in normal weight and diabetic patients, while RAS-MT CRC was more in overweight diabetic patients.
Another small study from Oman showed 24.6% WT and 26.7% as MT, with rectal CA showing less mutant type. The study was small with only half the cases tested for RAS [20].
High BMI among mCRC patients treated with bevacizumab is associated with shorter TTP [37].
In a small retrospective analysis of 109 cases from Oman, recurrence was documented in 35.8% patients. Median RFS was 22 months. With the univariate log rank analysis, age, BMI, absence of ischemic heart disease, tumor location, surgery, adjuvant chemotherapy, chemotherapy regimen, dose delays and adverse events post-chemotherapy were associated. Gender, family history, grade, disease stage, and K-Ras status were not associated with RFS.
Median OS for all patients was 43 months (range 0-146), with 5-year OS of 42%. Observed 5-year OS for stage I, II and III was 100%, 60% and 60% respectively, while all patients with stage IV disease at diagnosis died. The median survival for patients with stage IV disease was 17 months. On univariate analysis, age, BMI, diabetes, hypertension, metformin use, stage at diagnosis, site of metastasis, surgical intervention, chemotherapy, radiotherapy, chemotherapy regimen, number of the stage at diagnosis, access to medical care, availability of care and screening program [20]. OS in CRC from Oman is comparable to many EU countries and is better than neighbouring countries [38]. In Oman, most patients are less than 50 years, and only 8.6% have a positive family history. The screening guidelines and strategy, therefore, need to be modified accordingly.
Conclusions
CRC is the second most prevalent cancer in the Sultanate of Oman, and is on a rise. The cancer incidences are attributed to weight gain, changing eating habits and lifestyle, socioeconomic factors and low consumption of dietary fibre. Obesity is one of the main risk factors that are linked to the development and progression of CRC, associated with over 30 percent of the male CRC. Obesity must be considered as an early warning for a potential pre-neoplastic lesion. Oman is a country with a very high incidence of DM and High BMI. There is a need to study it and enforce preventive and management strategies. Better control may have a positive influence on the overall CRC scenario. Colorectal cancer is more common with younger age and obesity, consistent with more consumption of fast food in a younger age group. CRC occurring at a relatively young age has distinct issues and implications. It needs to be studied further in terms of genetic, environmental, and other causal factors influencing age at presentation.
The right-sided tumors as per our study are younger, with significant obesity, diabetic, and K-Ras mutant, and this with high meat and protein consumption in the Omani population. The sidedness or laterality of CRC needs further study in Oman. There is emerging data that right and left-sided lesions are different in terms of etiologic, pathogenesis, biologic behaviour, genetic makeup, response to treatment and outcome. The stage at presentation of CRC is often late in Oman. There are factors of health education, access to timely diagnostic workup, the status of primary health care, development and implementation of local screen program. These need to be worked out to improve early diagnosis. The molecular profile needs further evaluation to dissect out the local CRC. This may well have diagnostic, pathologic, management and treatment response implications.
Acknowledgements
Cancer Registry Section – Directorate of Non-communicable diseases, Ministry of Health, Sultanate of Oman.
The study was conducted at department of medical oncology – National oncology centre, the Royal hospital Muscat, Sultanate of Oman.
References
- Nooyi, Shalini, Jawad Al-Lawati. Cancer Incidence in Oman 1998-2006. Asian Pacific J Cancer Prev. 2011; 12: 1735-1738.
- Siegel RL, Jemal A, Thun MJ, et al. Trends in the incidence of colorectal cancer in relation to county-level poverty among blacks and J Natl Med Assoc. 2008; 100: 1441-1444.
- Siegel RL, Jemal A, Ward Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2009; 18: 1695-1698.
- SIain CRC trends reflect human development. Nature Reviews Gastroenterology & Hepatology. 2016; 13: 122.
- Ferlay, Jacques, Freddie Estimates of worldwide burden of cancer in 2008 GLOBOCAN 2008. International Journal for Cancer. 2010; 127: 2893-2917.
- https://internal.moh.gov.om/documents/272928/0/Cancer+Incident+2012+Final.pdf/bf8b0ac3-ad0f-4a1e-8f92-340b2b78c34e
- Shiyam Kumar, Ikram A Burney, Khawaja Farhan Zahid, et Colorectal Cancer Patient Characteristics Treatment and Survival in Oman a Single Center Study. Asian Pac J Cancer Prev. 2015; 16: 4853-4858.
- http://www.moh.gov.bh/pdf/publications/GCCCancerInci- pdf.
- http://www.worldgastroenterology.org/publications/e-wgn/e- wgn-expert-point-of-view-articles-collection/the-future-of- colorectal-cancer-prevention-in-developing-countries.
- Al-Lawati JA, Panduranga P, Al-Shaikh HA, et Epidemiology of Diabetes Mellitus in Oman Results from two decades of research. Sultan Qaboos Univ Med J. 2015; 15: e226-e333.
- Paul Peeters, Marloes T. Bazelier, Hubert GM, et al. The Risk of Colorectal Cancer in Patients with Type 2 Diabetes Associations with Treatment Stage and Obesity. Diabetes Care. 2015; 38: 495-502.
- Toru Nawa, Jun Kato, Hirofumi Kawamoto, et Differences between right- and left-sided colon cancer in patient characteristics, cancer morphology and histology. Journal of Gastroenterology and Hepatology. 2007; 23: 418-423.
- Benedix F, Kube R, Meyer F, et al. Comparison of 17,641 patients with right- and left-sided colon cancer differences in epidemiology, perioperative course histology and survival. Dis Colon Rectum. 2010; 53: 57-64.
- Susanna C. Larsson, Nicola Orsini, Alicja Wolk. Diabetes Mellitus and Risk of Colorectal Cancer. A Meta-Analysis. J Natl Cancer Inst. 2005; 97: 1679-1687.
- Pappas AV, Lagoudianakis EE, Dallianoudis IG, et Differences in colorectal cancer patterns between right and left sided colorectal cancer lesions. J BUON. 2010; 15: 509-513.
- Christine Dejea, Elizabeth C. Wick, Elizabeth M. Hechenbleikner, et al. Microbiota organization is a distinct feature of proximal colorectal cancers. PNAS. 2014; 111: 18321-18326.
- Michal Mik, Maciej Berut, Lukasz Dziki, et Right- and left- sided colon cancer clinical and pathological differences of the disease entity in one organ. Arch Med Sci. 2017; 13: 157-162.
- Jennifer M. Weiss, Patrick R. Pfau, Erin S. O'Connor, et al. Mortality by Stage for Right- Versus Left-Sided Colon Cancer Analysis of Surveillance Epidemiology and End Results–Medicare Journal of Clinical Oncology. 2011; 29: 4401-4409.
- Loupakis F, Yang D, Yau L, et Primary tumour location as a prognostic factor in metastatic colorectal cancer. J Natl Cancer Inst. 2015; 107: dju427.
- Hiroshi Hamada, Chikara Meno, Daisuke Watanabe, et al. Establishment of vertebrate left–right Nature Reviews Genetics. 2002; 3: 103-113.
- SIain CRC trends reflect human development. Nature Reviews Gastroenterology & Hepatology. 2016; 13: 122.
- Faraz Bishehsari, Mahboobeh Mahdavinia, Michele Vacca, et Epidemiological transition of colorectal cancer in developing countries Environmental factors molecular pathways and opportunities for prevention. World J Gastroenterol. 2014; 20: 6055-6072.
- Itrat Mehdi, Essam Abdul Monem, Bassim Jaffar Al Bahrani, et Age at diagnosis of female breast cancer in Oman Issues and implications. South Asian J Cancer. 2014; 3: 101-106.
- Mehdi Malignant Gastrointestinal tumours. Are they increasing? JPMA. 1997; 47: 1-3.
- Greg Hislop. Trends and risk factors for colorectal cancer. 2000; 42: 131-135.
- Musthafa Chalikandy Peedikayil, Prem Nair, Seena SM, et al. Colorectal cancer distribution in 220 Indian patients undergoing colonoscopy. Indian J of Gastroenterology. 2009; 28: 212-215.
- Rebecca Siegel, Carol DeSantis, Ahmedin Jemal. Colorectal cancer 2014. CA A cancer J for Clinicians. 2014.
- Olga Giouleme, Michael D Diamantidis, Marios G Is diabetes a causal agent for colorectal cancer? Pathophysiological and molecular mechanisms. World J Gastroenterol. 2011; 17: 444-448.
- Susan Richman, Julian Adlard. Left and right sided large bowel cancer Have significant genetic differences in addition to well-known clinical BMJ. 2002; 324: 931-932.
- Alan P. Venook, Donna Niedzwiecki, Federico Innocenti, et Impact of primary (1º) tumour location on overall survival OS and progression-free survival PFS in patients pts with metastatic colorectal cancer mCRC Analysis of CALGB/ SWOG 80405 Alliance. J Clin Oncol. 2016; 34.
- Faruk Aykan N, Ibrahim YildizFatma, SenLeyla KilicSerkan, et al. Effect of increased body mass index BMI on time to tumour progression TTP in unresectable metastatic colorectal cancer mCRC patients treated with bevacizumab-based Medical Oncology. 2013; 30: 679.
- Heinz-Josef Lenz. Right or left metastatic colon cancer Will the side change your ESMO. Copenhagen. 2016.
- Susan Richman, Julian Adlard. Left and right sided large bowel cancer Have significant genetic differences in addition to well-known clinical BMJ. 2002; 20: 931-932.
- Boeckx N, Toler A, Op de Beeck K, et al. Primary tumor sidedness impacts on prognosis and treatment outcome results from three randomized studies of panitumumab plus chemotherapy versus chemotherapy or chemotherapy plus bevacizumab in 1st and 2nd line RAS/BRAF WT Ann Oncol. 2016; 27.
- Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol. 2011; 29: 1465-1471.
- Sabine Tejpar, Sebastian Stintzing, Fortunato Ciardiello, et Prognostic and Predictive Relevance of Primary Tumor Location in Patients with RAS Wild-Type Metastatic Colorectal Cancer - Retrospective Analyses of the CRYSTAL and FIRE-3 Trials. JAMA Oncol. 2017; 3: 194-201.
- Van Cutsem E, Cervantes A, Adam R, et ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016; 27: 1386-1422.
- Javier Martinez, Jesus Garcia-Foncillas. Obesity and colorectal cancer molecular features of adipose Journal of Translational Medicine. 2016; 14: 21.