Lessons Learned Treating Retinoblastoma in Panama Children's Hospital
Author'(s): Napoleon Chen1, María Sabina Ah Chu1*, Roberto Yee2 and Daniel Sanchez2
1Pediatric Oncologist, Panamá Children`s Hospital, StatisticsFaculty of National Panama University, Panama.
2Pediatric Ophthalmologist, Panamá Children`s Hospital,Statistics Faculty of National Panama University, Panama.
*Correspondence:
María Sabina Ah Chu Sánchez, Pediatric Oncologist Panamá Children’s Hospital, Panama, E-mail: compahumani@hotmail.com.
Received: 03 January 2018; Accepted: 24 January 2018
Citation: Napoleon Chen, María Sabina Ah Chu, Roberto Yee, et al. Lessons Learned Treating Retinoblastoma in Panama Children’sHospital. Cancer Sci Res. 2018; 1(1); 1-3.
Keywords
Introdution
Retinoblastoma is the most ocular tumor during infancy. Its diagnosis requires the suspicion of a family member or the personnel who attend the child, especially the pediatrician. This is an entity that requires a multidisciplinary approach and its long tern survivance is increasing.
The authors review 20 years of experiences in Panama Children’s Hospital that is a third level pediatric hospital, located at Panama City, the capital city of Panama, with the mission of provide the best management of childhood pathology based on scientific evidence.
Material & Methods
This is an observational, retrospective, descriptive and transversal study that includes:
Patients with diagnosis of retinoblastoma confirmed by histology between January 1, 1996 and December 31, 2016, who at the moment of data collection (January 2017) finished treatment and are at the follow-up consultation for at least one year.
We excluded
- Those patients lost from the follow-up consultation for more than one year.
- Patients with incomplete data of
- Patients who are on treatment at the moment of data
We collected the data in Excel (version 2010) and calculated the rank, frequency, media, ratio, mean, mode or percentage according to the parameters of interest:
- Age in months at diagnosis.
- Gender (male/female).
- Principal symptom at
- Unilaterally or
- Compromise extension including: extensively compromise of the face and cranial structures (buftalmos), transcoroideal, exclusively retinal compromise, orbit compromise, retina and optic nerve compromise, cerebral spinal fluid compromise, ganglionic compromise, bone compromise.
- Age in months at the time of enucleation.
- If the patient receive chemotherapy (yes/no)
- If the patient receive radiation therapy (yes/no).
- If the patient receive close observation as only assessment (yes/no).
- The use of laser and/or cryotherapy with conservative intention (yes/no).
- Age in years at the moment of last consultation.
- Status at the last follow-up consultation (alive/death).
- Level of education (toddler, preschooler, elementary school, high-school, education with especial adaption, college, professional).
Results
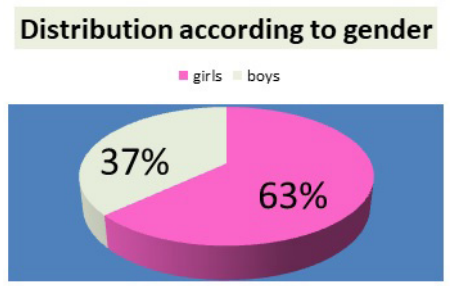
We collected the data of 38 retinoblastoma patients. This is the distribution according to gender.
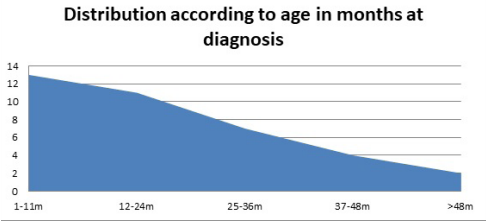
According to our data the range of the age at diagnosis is between 3 – 70 months. The mean age at diagnosis in months is 21.3 months. The mode is 13 months. This is the distribution according to age in months at diagnosis.
The most common symptom was leucocoria (white pupil) that its 86.8% of total.
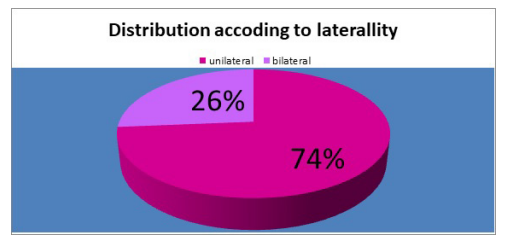
This is the distribution according to laterality.
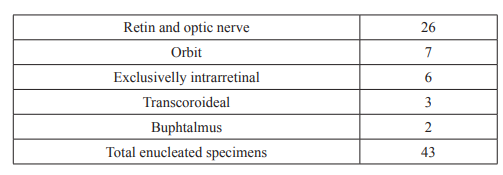
We reviewed 43 enucleated eyes. Table 1 shows the extension of compromise.
This is the distribution according to primary approach: Enucleation vs. Conservative.

All the conservative approach cases what receive laser and cryotherapy.
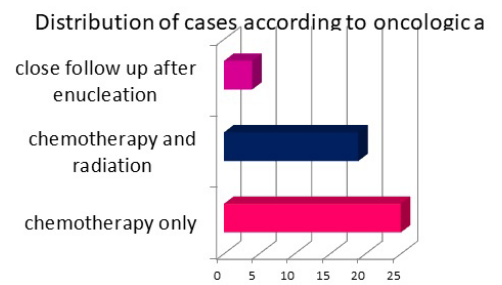
According to our results 52% of our patients, receive chemotherapy after enucleation, 39.6% receive chemotherapy and radiation therapy and 8.3% did not receive chemo or radiotherapy.
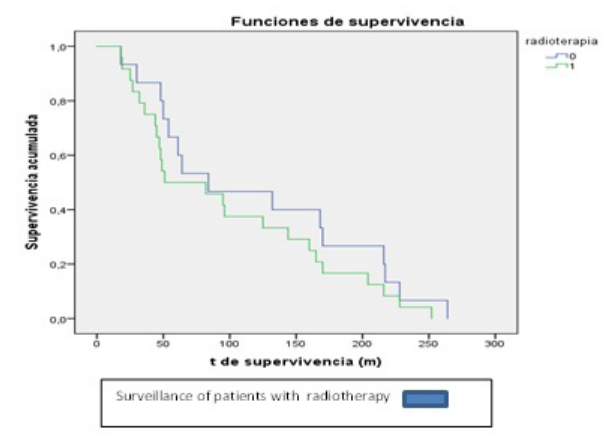
This is the surveillance graphic of the patients that receive radiotherapy:
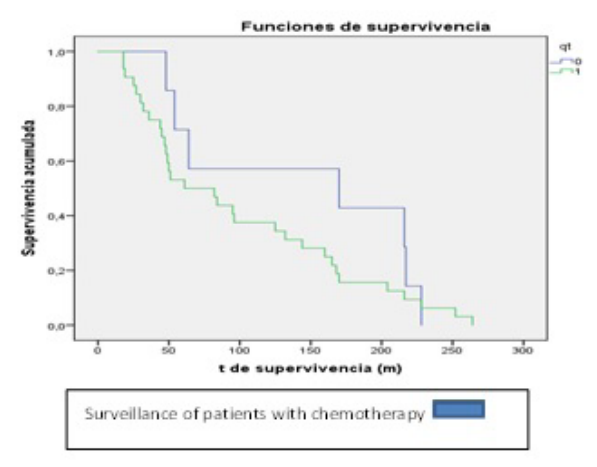
This is the surveillance graphic of the patients that receive chemotherapy:
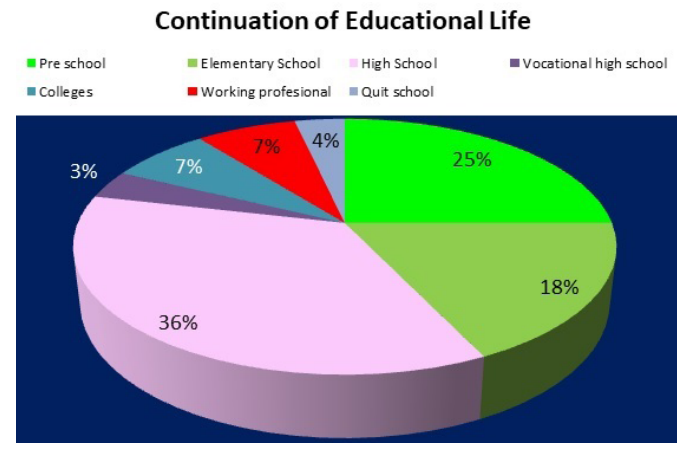
This is the distribution according to level of education:
Conclusion
In Panama, thanks to combined efforts like:
- The Ministry of Health Program of Growth and Developing during Early Childhood
- The campaign of “Early signs of cancer in children” promoted by the FANLYC Association for Kids with Leukemia and Tumors
- The project of continual medical and nurse education involving Panamá Children’s Hospital and Texas Children’s Hospital of Houston.
Nowadays the diagnosis of retinoblastoma is made early. There are cases of extensive compromise of the face and cranial structures, coming from the indigenous aboriginal regions of our country. Our efforts should be directed to those communities. Today thanks to more conscience of the heath personnel and the general public is possible to offer effective treatment that produce increasing surveillances and good quality of life. The message of this, long term survivors are: CONTINUE WORKING OF EARLY DETECTION AND CLOSE FOLLOW-UP.
References
- Hurwitz R, Shields C, Shields J, et al. Retinoblastoma en Pizzo P, Poplack D, Principles and Practice of Pediatric Oncology, 5ª Edición, Filadelfia, Lippincott, Williams and 2006; 865-886.
- Leahey A: Retinoblastoma en Lanzkowsky P, Lipton J, Fish J, Manual of Pediatric Hematology & Oncology, 6ª Edición, Filadelfia, ©Academic 2011; 788.
- Lagrutta F, Coronado L. Normas de Manejo de Problemas Pediátricos, 4ª Edición, segunda reedición, Panamá, Imbase A. 2014; 213.
- Aviña J, Hernández Síndrome de Wolf-Hirschhorn: Microdeleción distal del brazo corto del cromosoma 4, Revista Chilena de Pediatría, 2008; 79: 50-53.
- Ah Chu MS. Tumores Sólidos en Pediatría, Primera Edición, Panamá, Praga’s 2017; 80.
- Mondal R, Dasgupta J, Ghosh J. Miscellaneous Neoplastic Disorders in Children (Hepatoblastoma/ Retinoblastoma/ Germ Cell Tumors) en Mondal R, Essential Pediatric Oncology, Primera edición, Nueva Delhi, Jaypee Brothers Medical Publishers (P) 2016; 153-157.