Loss of Consciousness (LoC) from Potential Double Origin
Author'(s): Camara Youssouf1*, Bâ Hamidou Oumar2, Sangaré Ibrahima2, Diarra Alou3, Doumbia Coumba Thiam1, Coulibaly Souleymane3, Diall Ilo Bella3, Menta Ichaka2 and Diallo Boubakar3
1 CHU Kati, Kati, Mali
2 CHU Gabriel Touré, Bamako, Mali
3 CHU Point G, Bamako, Mali
*Correspondence:
Camara Youssouf, Cardiology Department, University Hospital Kati, Mali, E-mail: cestoto29@yahoo.fr
Received: 25 September 2018; Accepted: 06 October 2018
Citation: Camara Youssouf, Bâ Hamidou Oumar, Sangaré Ibrahima, et al. Loss of Consciousness (LoC) from Potential Double Origin. Cardiol Vasc Res. 2018; 2(4): 1-3.
Keywords
Introduction
Transient loss of consciousness (LoC) is loss of consciousness with complete recovery. It is commonly described by the patient as a blackout [1]. LoC can result from several disorders mainly cardiovascular but nervous system dysfunction account for about 10% [2].
We report a case of LoC by an 65 years old woman with complete AV block and long QT by which the 24 hours ECG revealed more severe disorders namely "Torsades de pointe" (TdP).
Case presentation
A 65 year-old woman came, referred for episodic prolonged LoC. This patient was symptomatic 2 months ago with: dizziness, faintness with two episodes of LoC of several minutes, according to her family. They reported neither abnormal movement, nor tongue bite, nor sphincter disorder.
After a first hospitalization on 2017 October 14 for diabetes imbalance, the patient presented one day after a new episode of LoC. This one started after palpitation with heart rate of 150/min with gradual return to consciousness after 2 minutes. There was nor clinical sign nor neurological focal sign.
This patient had diabetes for more than 10 years, hypertension and treated with insulin and captopril+hydrochlorothiazide. At admission she was asthenic with moderate alteration of physical condition. There was no fever. The clinical examination revealed a regular rhythm with heart rate of 36/min, normal pulse finding and pressure of 160/80 mmHg. Pulmonary as well as other organ examination didn’t reveal any abnormality.
Laboratory tests showed normal renal function (serum creatinine 11mg / l), no ionic disturbance (Kalium 4 mmol / l, Sodium 139mmol / l), elevated blood glucose of 1.68g / l and normochromic microcytic anemia (Hb = 11.3g / dl VGM = 68%, TCMH = 22.9 μg).
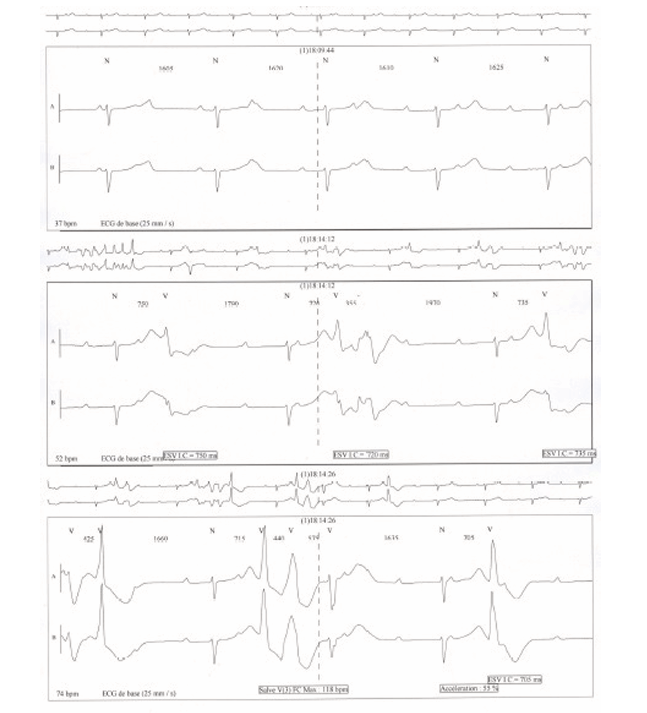
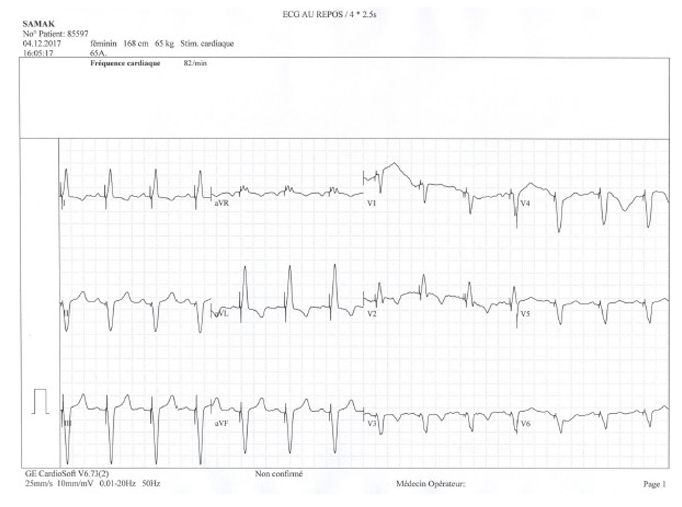
Electrocardiogram (ECG) showed a complete AV-block with a junctional escape at 47 beats / min associated with ventricular extrasystoles, sometimes in bigeminus, and a long QT at 488-529 m (Figure 1).
Echocardiography found normal left VG (EF 70%, dp/dt 113 mmHg), no valvular abnormality but dilated right ventricle with systolic pulmonary arterial pressure of 74 mmHg. There was no pericardial abnormality.
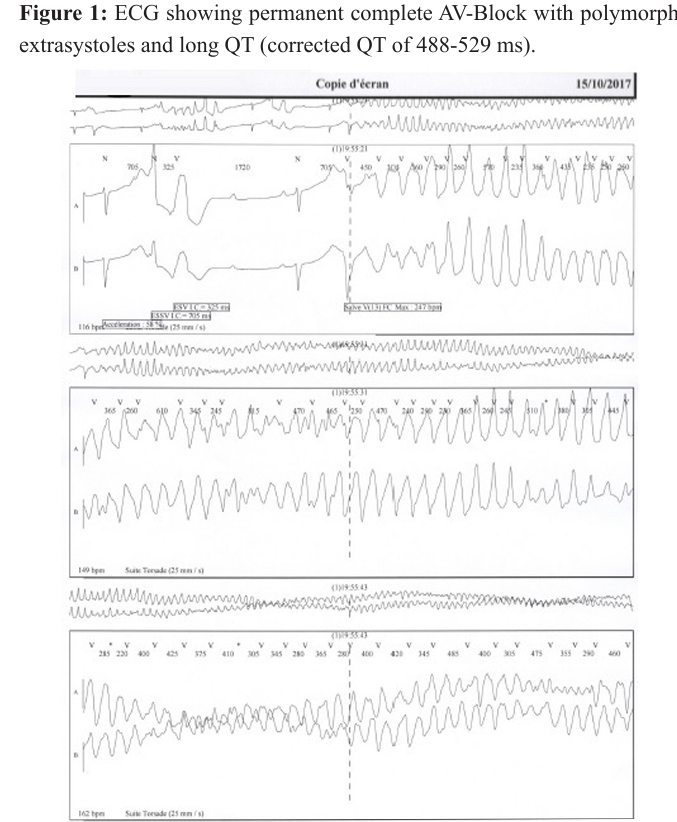
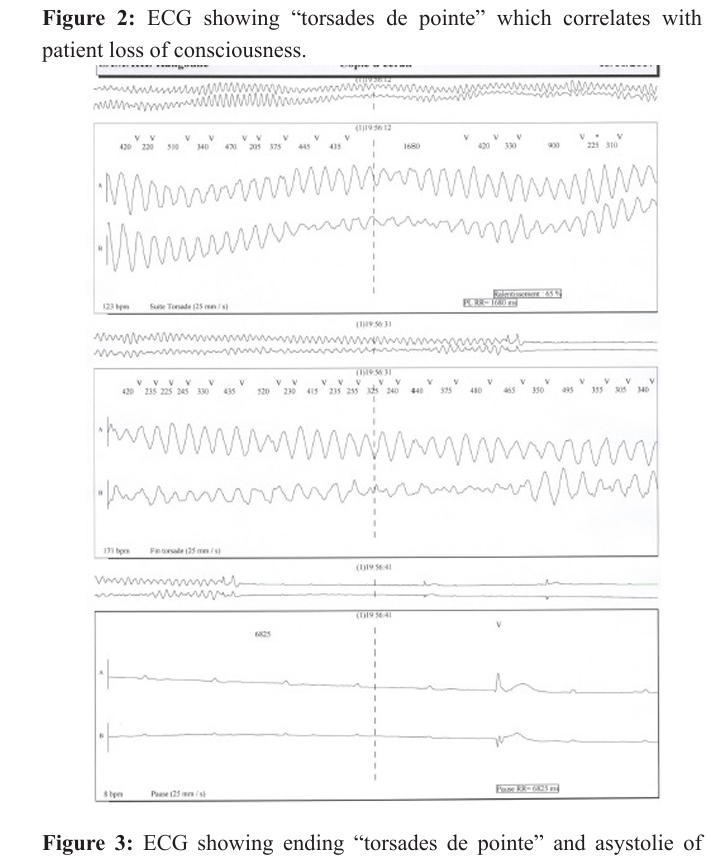
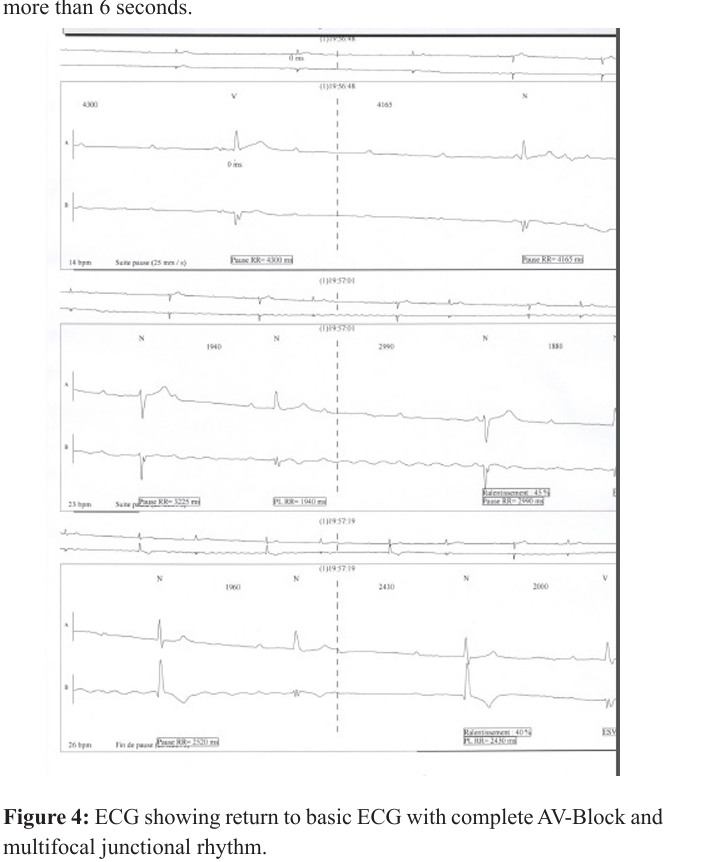
A 24H ECG found: complete AV-Block, junctional rhythm of 36/ min, several “torsades de pointe” up to 1.11 min a QT elongation to 488-529 ms, arrests up to 6 secondes and ventricular extrasystoles. These findings were concomitant with LoC.
The patient became on 2017 october 16 a DDD-Pace-maker set at 70/min. From this time up to now, she remains free of symptoms and felt wery well.
Discussion
From the numerous causes of LoC, cardiovascular system disorders and nervous system dysfunction are the commonest findings [3] and requiring genetic testing [4]. The latter is not available in our context.
Central Nervous system disorders had been ruled out through patient history, absence of seizures. We also ruled out hypoglycemic syncope as possible cause as noted by Lagi and Cencetti [5]. The patient had no hypoglycemia when presented LoC.
As the patient had neither electrolyte disturbance nor potential arrhythmic medication an acquired long QT syndrome seems less probable. It is known that third degree AV block with a wide QRS escape rhythm often presents with fatigue, dyspnea, presyncope or frank unheralded syncope. Rarely ventricular fibrillation and TdP tachycardia can result from marked tachycardia and prolonged pauses [6].
Sex differences exist in arrythmia. Long QT syndrome (acquired and congenital ) are more frequent in women opposed to AVblock [7]. It is so that infra his escape rhythm are more likely to be associated with prolonged asystole, leading to syncope and sudden death [7]. We had in this case a more junctional multifocal escape rhythm in the setting of severe bradycardia and complete AV-block.
Due to lack of labor equipment we were unable to make a molecular screening. Based on Schwartz criteria [8] our patient had a high probability (clinical history, QTc and TdP). Permanent complete AV-Block with junctional escape rhythms are less likely to provoke LoC in this patient so that we retained episodic TdP on long QT was responsible in this case for patient LoC.
There was an indication for pacemaker (PM) implantation as well for severe bradycardia as for TdP. This was achieved by the implantation of a DDD-PM making the patient symptom free. We have not been able to perform genetic testing in order to confirm congenital long QT syndrome.
References
- Rogers G, O’Flynn N. NICE guideline: transient loss of consciousness (blackouts) in adults and young people. British Journal of General Practice. 2011; 40-42.
- Fernandes PM, Davenport RJ. Transient loss of consciousness first ever seizure? Tips for the Acute Receiving Unit Scottish Universities Medical Journal. 2013; 2: 5-12.
- Simon RP. Syncope and transient loss of consciousnessDifferential diagnosis and treatment (Medical Information). West J Med. 1975; 123: 164-170.
- Milburn-McNulty P, Larner AJ. Episodic loss of consciousness: how genetic testing points to diagnosis. Progress in Neurology and Psychiatry. 2018; 22: 18-19.
- Lagi Alfonso, Cencetti Simone. Transient loss of consciousness, syncope and hypoglycaemia Cardiovascular Endocrinology & Metabolism. 2012; 1: 20-23.
- John RM. Atrioventricular Block. In Zipes DP, Jalife J, Stevenson WG. Cardica Electrophysiology: from cell to bedside-Seventh Edition. ISBN 978-0-323-44733-1. 1006.
- Ozcan C, Curtis AB. Sex differences in arrhythmias. In Zipes DP, Jalife J, Stevenson WG. Cardica Electrophysiology: from cell to bedside-Seventh Edition. ISBN 978-0-323-44733-1. 1013
- Schwartz PJ, Crotti L. Long and short QT syndromes. In Zipes DP, Jalife J, Stevenson WG. Cardica Electrophysiology: from cell to bedside-Seventh Edition. ISBN 978-0-323-44733-1. 897.