Lower Uterine Section Transverse Incision Defect and Ectopic in the Cesarean Section Scar: A Case Presentation and Review of The Literature
Author(s): Vasilios T. Goudas, MD FACOG*
NYU Langone Reproductive Specialists of New York, USA.
*Correspondence:
Vasilios T. Goudas, NYU Langone Reproductive Specialists of New York, 200 Old Country Road Suite 350, Mineola New York 11501, USA.
Received: 02 November 2020 Accepted: 18 November 2020
Citation: Goudas VT. Lower Uterine Section Transverse Incision Defect and Ectopic in the Cesarean Section Scar: A Case Presentation and Review of The Literature. Gynecol Reprod Health. 2020; 4(6): 1-4.
Abstract
The aim of this paper is to present the first patient where a lower uterine segment transverse incision defect that led to a cesarean section scar ectopic pregnancy was repaired at the same time with Hysterotomy for removal of her persistent ectopic pregnancy. We also reviewed the literature.
Background: Cesarean Sections leave on occasion the lower uterine segment thinner with resulting consequences that range from bleeding, fluid in the cavity, pain, cramping and infertility. In addition, ectopic implantation at the cesarean section site is relatively common.
Case: A patient treated for infertility primarily resulting from lower uterine segment transverse incision deficit (LUSTID) is presented. After she conceived with IUI it was noted that she had an ectopic pregnancy. Methotrexate was given and the hCG declined but the gestational sac remained in the lower uterine segment with the mean diameter increasing. The patient underwent a laparotomy and hysterotomy, with hysteroscopic guidance. The pregnancy was removed and the incision was rejuvenated and re-approximated. The literature was searched for similar cases but none were found.
Discussion: LUSTID should be recognized as a cause of infertility and strongly considered in secondary infertility patients. This is the first case we identified in the literature with primary intent hysterotomy for a cesarean section scar ectopic removal and repair. We also propose criteria for surgical intervention.
Keywords
Introduction
Low uterine segment transverse Cesarean Section is the most frequently performed surgery in obstetrics with a reported frequency of 31.9% of deliveries in the USA reported by the CDC [1]. While Cesarean Section is an indispensable tool in Obstetrics, like all surgical procedures it carries risks. As a procedure performed in young and for the most part healthy women, the incidence of severe morbidity and mortality is relatively low, approximating 2.9% [2] nevertheless we are recently identifying additional risks, such as that of Post-Cesarean Syndrome [3-7].
That has been defined broadly as symptoms resulting from the presence of a defect in the lower uterine segment (Lower Uterine Segment Transverse Incision Defect, LUSTIDs). Such symptoms can be pain, bleeding [7] and dysmenorrhea [6]. In addition, the likelihood of a larger defect increases with retro flexion and repeat cesarean deliveries [6]. Such cases are also identified at the time of delivery and the thickness of the remaining lower uterine segment wall is a determinant of the likelihood of complications during labor. In a more recent identified expression of LUSTIDS is infertility, as documented by failure to conceive in the absence of any other cause of infertility [3,8]. We present a case series of patients with LUSTIDS, starting with a Cesarean Section Ectopic managed with primary intent repair at the time of Hysterotomy
Case
34 y.o. WF P2002 normo-ovulatory patient with a history of 2 prior Cesarean Sections conceived spontaneously, presented in our practice with secondary infertility. The patient reported having no difficulties in her two prior conceptions and had been trying to conceive in the past year. An initial evaluation with a hysterosalpingogram reported a normal cavity with bilateral tubal patency; seminal parameters were likewise normal. The only relevant finding in her evaluation was a 4 mm defect in the lower uterine segment. The patient denied any symptoms relating to the defect, such as bleeding at irregular times or pain. She underwent ovulation induction with clomiphene citrate and intrauterine insemination and conceived with the first cycle. At her first pregnancy sonogram, a pregnancy sac was identified at the level of the Cesarean Section Scar. She was given Methotrexate and the serum hCG levels declined slowly as did the serum progesterone. The gestational sac however remained in place and continued to slowly increase in size from an original 5.5 mm to 15 mm in largest diameter 40 days after the Methotrexate injection (Figure 1).
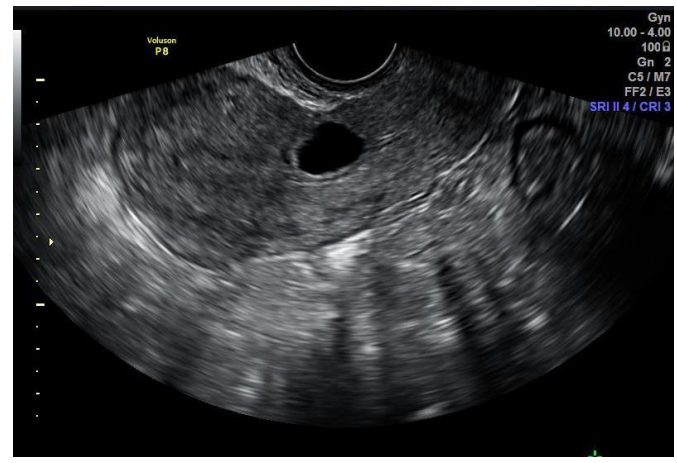
Figure 1: A. Cesarean Section Ectopic pregnancy sac. There is only a 2mm wall over the sac.
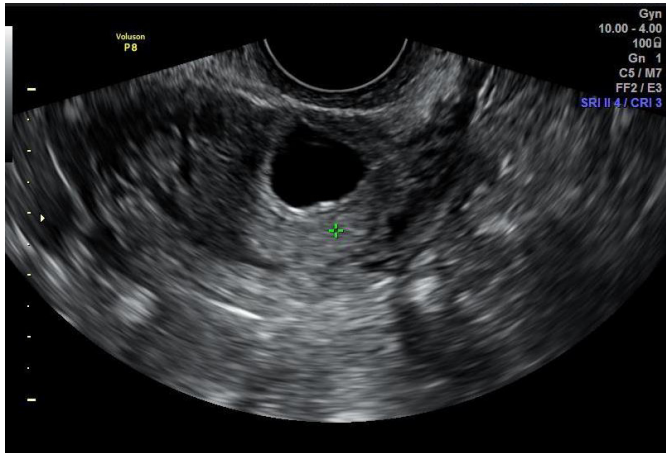
B.Transverse view of the ectopic pregnancy. Minimal distance from the anterior wall.
When the patient started to have significant vaginal bleeding that persisted for 1 week with the sac still in place, a decision was made to take the patient to the OR for hysterotomy and removal of the ectopic as well as repair of the deficit at the same time. After the gestational sac was identified hysteroscopically (Figure 2A), the patient underwent a laparotomy through her prior lower transverse abdominal incision. With the help of transillumination the defective thinned out anterior aspect of the. The bladder then the lower uterine segment was entered abdominally, the pregnancy was removed and the edges were rejuvenated. The defect was then re-approximated with interrupted “figure of 8” delayed-absorbable 0-0 polyglycolic sutures. When the sutures were tied hysteroscopy confirmed the elimination of the deficit (Figure2B). Following a 2-month recovery period and an additional two months of trying to conceive at home, a saline infusion sonogram was performed that identified that the deficit had been repaired. She then underwent ovulation induction and IUI and conceived with the first cycle. Two gestational sacs were identified, both with fetal cardiac activity and she is currently in her second trimester with both pregnancies progressing well.
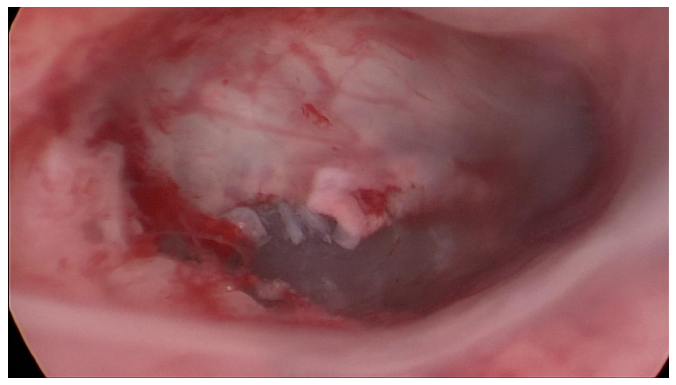
Figure 2: A. The gestational sac is visible in the lower uterine segment.

B. After the figure of eight stiches are closed, the cervical canal has receded to a narrower diameter.
Discussion
Caesarean section through lower uterine segment transverse incision is the most frequently performed surgery in obstetrics with a reported frequency of 31.9% of deliveries in the USA reported by the CDC [1]. While Cesarean Section is an indispensable tool in Obstetrics, like all procedures it carries risks. As a procedure performed in young and for the most part healthy women, the incidence of severe morbidity and mortality is relatively low, approximating 2.9 % [2]. A recently identified negative late outcome is the so-called Post-Cesarean Syndrome [3-7].
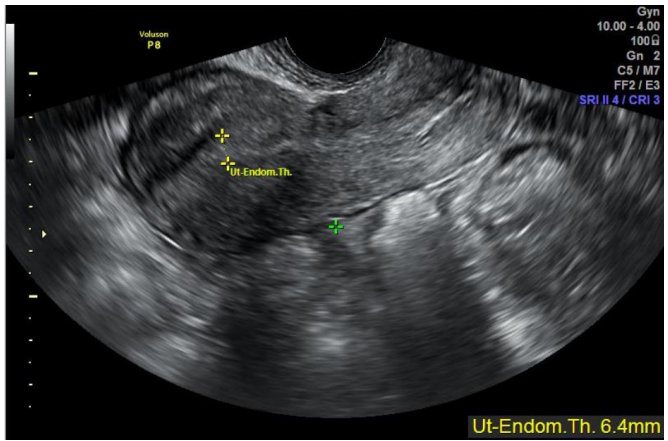
Figure 3: Following the repair the defect has been eliminated.
That is defined broadly as bleeding after the period is finished or pain and dysmenorrhea resulting from the presence of a defect in the lower uterine segment [9]. The presence of a defect has been reported in 293 women out of a cohort of 4250 women with history of cesarean section for a crude ratio of 6.9% of the population [6]. However according to varying definitions, the prevalence of a cesarean section defect has been even reported to be between 19 and 84%. The symptomatic defects are likely to be much lower though. When symptoms are assigned to the defect, they fall in two categories. One is pain, during or after period, and the other is post-menstrual bleeding, as a result of retained blood [7].
The notion that a Cesarean Section may have a negative effect in future fertility is supported by a large population study from the Denmark [10]. A prior Cesarean section, whether elective or requested is associated with a lower chance for future delivery. Whether this finding reflects maternal choice or biological consequence is debatable, however if time to conception is used as a marker of fecund ability, as it has been used as such [11], there are various reports showing that both adhesion formation and time to delivery increases with each subsequent Cesarean Section [12].
A likely explanation of the mechanism that leads to infertility is that the space in the lower uterine segment formed by the defect allows for the collection of blood thus leading to intermenstrual bleeding and affects the microenvironment, thus preventing implantation [8].
In patients with existing defects, when undergoing controlled ovarian hyper stimulation such as for IVF, the incidence of intracavitary fluid has been reported as high as 40% [13]. This observation suggests that besides the microenvironment there may be a “mechanical” or hydraulic effect where the cavitary fluid may help expel the conceptus from the cavity.
A relationship of a Cesarean section scar to miscarriages is not supported though by the observation that past cesarean sections do not appear to increase the likelihood of miscarriage as indicated by a large population-based cohort study based on the same Danish population cohort [14]. An effect of the Cesarean Section in the fallopian tubes is also not apparently clinically significant in another population-based case-control study [15].
When the scar of the cesarean section is above the lower uterine segment at the cervix, something that reportedly happens in approximately 20.9% [16], then there is connective tissue covering myometrium making it more likely that there can be myometrial invasion during a cervical ectopic pregnancy. This can explain why despite the decline of hCG in our patient there was no expulsion, possible because of deeper/myometrial implantation of the placenta.
In summary, we are presenting the first case where a hysterotomy guided by hysteroscopy was performed to first remove and then by primary intent re-approximate the lower segment using interrupted “figure of 8” delayed-absorbable sutures.
Caesarean scar defects, Uterine scar insufficiency, isthmocele or scar dehiscence following a caesarean section involve myometrial discontinuity at the site of a scar from previous caesarean section. These anatomical defects associated with prolonged menstrual bleeding, chronic pelvic pain, dysmenorrhea, dyspareunia and secondary infertility as well as possible Cesarean Section Scar ectopic pregnancy. Repair of the uterine scar defect in the non- pregnant state can be affected with laparoscopy or laparotomy, while when infertility is the issue, management may be more complex.
We propose that in a patient with secondary infertility following cesarean section or sections, it is meaningful to enquire specifically about symptoms that may be manifestation of Cesarean Section defects. Proper imaging with transvaginal sonography and including saline infusion sonohysterography may help measure the thickness of the residual myometrium. In the absence of another cause of infertility repair of the defect in the non-pregnant state can be discussed. Finally, as was exhibited in our case, in a Cesarean Section Scar ectopic pregnancy, the defect can be repaired at the same time with a hysterotomy for removal of the ectopic pregnancy and re-approximation after rejuvenation of the edges.
References
- Joyce A Martin MPH, Brady E Hamilton, Michelle JK, et al. Births: Final Data for 2018. National Vital Statistics 2019; 68: 1-47.
- Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012; 120: 1029-1036.
- Gubbini G, Centini G, Nascetti D, et Surgical hysteroscopic treatment of cesarean-induced isthmocele in restoring fertility: prospective study. J Minim Invasive Gynecol. 2011; 18: 234- 237.
- Florio P, Gubbini G, Marra E, et al. A retrospective case- control study comparing hysteroscopic resection versus hormonal modulation in treating menstrual disorders due to isthmocele. Gynecol Endocrinol. 2011; 27: 434-438.
- Gubbini G, Casadio P, Marra Resectoscopic correction of the "isthmocele" in women with postmenstrual abnormal uterine bleeding and secondary infertility. J Minim Invasive Gynecol. 2008; 15: 172-175.
- Wang CB, Chiu WW, Lee CY, et al. Cesarean scar defect: correlation between Cesarean section number, defect size, clinical symptoms and uterine position. Ultrasound Obstet Gynecol. 2009; 34: 85-89.
- Fabres C, Arriagada P, Fernandez C, et Surgical treatment and follow-up of women with intermenstrual bleeding due to cesarean section scar defect. J Minim Invasive Gynecol. 2005; 12: 25-28.
- Florio P, Filippeschi M, Moncini I, et al. Hysteroscopic treatment of the cesarean-induced isthmocele in restoring infertility. Curr Opin Obstet Gynecol. 2012; 24: 180-186.
- Tower AM, Frishman GN. Cesarean scar defects: an underrecognized cause of abnormal uterine bleeding and other gynecologic J Minim Invasive Gynecol. 2013; 20: 562-572.
- O'Neill SM, Khashan AS, Henriksen TB, et al. Does a Caesarean section increase the time to a second live birth? A register-based cohort Hum Reprod. 2014; 29: 2560- 2568.
- Maheshwari A, Bhattacharya S, Johnson NP. Predicting fertility. Hum Fertil (Camb). 2008; 11: 109-117.
- Tulandi T, Agdi M, Zarei A, et al. Adhesion development and morbidity after repeat cesarean delivery. Am J Obstet Gynecol. 2009; 201: 56 e1-e6.
- Lawrenz B, Melado L, Garrido N, et al. Isthmocele and ovarian stimulation for IVF: considerations for a reproductive medicine specialist. Hum Reprod. 2019; 35: 89-99.
- O'Neill SM, Agerbo E, Kenny LC, et al. Cesarean section and rate of subsequent stillbirth, miscarriage, and ectopic pregnancy: a Danish register-based cohort study. PLoS Med. 2014; 11: e1001670.
- Wolf ME, Daling JR, Voigt LF. Prior cesarean delivery in women with secondary tubal infertility. Am J Public Health. 1990; 80: 1382-1383.
- Markovitch O, Tepper R, Hershkovitz R. Sonographic assessment of post-cesarean section uterine scar in pregnant women. J Matern Fetal Neonatal Med. 2013; 26: 173-175.