Non-Puperal Uterine Inversion: About Three Case
Author(s): Mouhamadou WADE, Babacar BIAYE*, Abdoulaye DIAKHATE, Simon Biran NDOUR, Mor CISSE, Khalifa Ababacar GUEYE, Abdou Aziz DIOUF, Mamour GUEYE, Jean Charles MOREAU
Aristide Le Dantec Hospital, Gynecologist, Dakar, Senegal.
*Correspondence:
BIAYE Babacar, Aristide Le Dantec Hospital, Gynecologist, Dakar, Senegal.
Received: 13 August 2020 Accepted: 01 September 2020
Citation: Wade M, Biaye B, Diakhate A, et al. Non-Puperal Uterine Inversion: About Three Case. 2020; 4(4): 1-3.
Abstract
Inversion of the uterus usually occur during delivery. Non puerperal inversion is rare, it’s usually associated with an underlying benign or malignant uterine mass. Clinical diagnosis of uterine inversion can be easy in complete forme ; However, incomplete uterine inversion is difficult to identify, MR imaging can be usefull. The treatment of the inversion is Chirurgical, that depend to the stage of inversion and associated pathology.
Keywords
Introduction
Non-puerperal uterine inversion is an extremely rare clinical situation. 85% of uterine inversions are puerperal, complicating delivery bleeding. Non-puerperal uterine inversion most often follows a prolapsed endo-cavitary myoma, which may require two approaches (vaginal and abdominal).
We report 3 cases of non-puerperal uterine inversion.
Observations
Case 1
The patient was 27 years old unmarried nulligeste with no particular pathological history, presenting menometrorrhagia on a fundic mass of about 3 cm.
Clinical examination at the entrance showed a soft, depressed abdomen without palpable mass, no cry from the umbilicus. Hernial orifices were free. However, the speculum examination and vaginal touch were not done because the patient was a virgin. The rest of the clinical examination was unremarkable.
The biological assessment showed severe anemia with a hemoglobin level of 5.8g/dl.Pelvic ultrasonography by the trans abdominal route revealed a slightly echogenic vascularized endocavitary image of 35.3x30.2 mm, and the adnexa were normal (Figure 1).
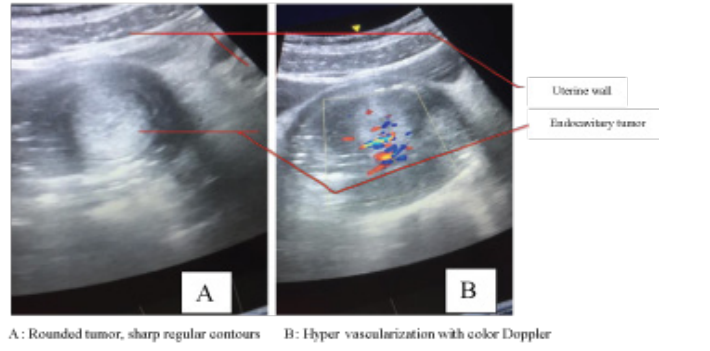
Figure 1: Trans abdominal pelvic ultrasound
The clinical picture was complicated by third degree uterine inversion after 3 weeks with a fleshy vascularized budding mass of 12 cm long by 5 cm long axis hanging from the inverted uterine fundus (Figure 2A).
Surgical management had required two steps:
- First stage: We performed a vaginal approach with the removal of the mass with an electric scalpel at the level of the mucous membrane. The mass weighed 450g.
- Second step: we performed an abdominal approach with a pfannenstiel incision.
On exploration, the uterine cavity was empty and filled by the adnexa which were aspirated into the vagina through a cervical constriction ring (Figure 2B).
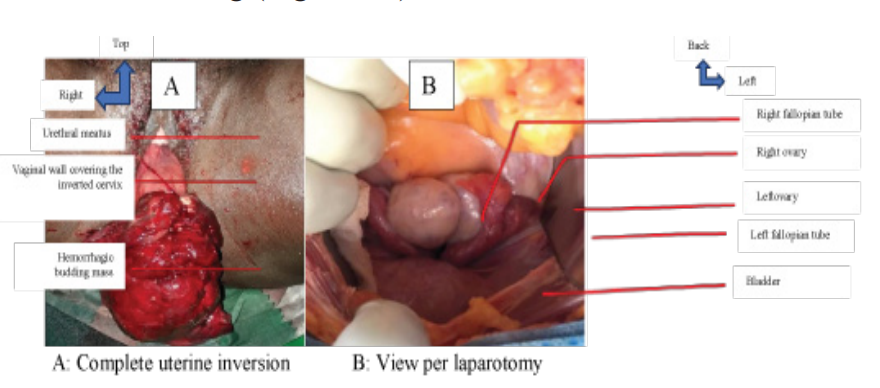
Figure 2: Macroscopic aspect
The procedure consisted of manual vaginal compression of the uterus followed by vesico-uterine dissection and a 5 cm corporal cervico-hysterotomy followed by uterine reintegration into the pelvis and Vicryl 1 suture.
The postoperative follow-up was simple. The anatomo- pathological examination of the surgical specimen was in favor of an endometrial benign glandular polyp.
Case 2
This is a 40-year-old IVP VG who was evacuated for a hemorrhagic myoma delivered through the cervix. On admission, the patient presented with cardiovascular collapse, a 5 cm rounded, firm, pedicled, hemorrhagic mass appended to the uterine fundus suggestive of uterine myoma (Figure 3A).
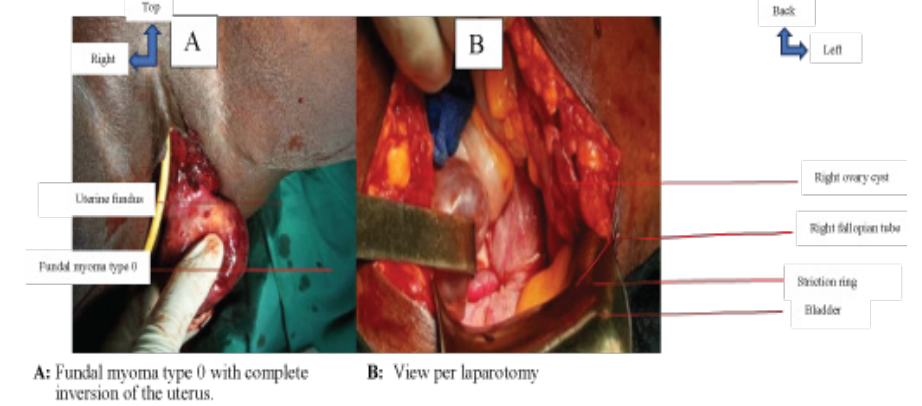
Figure 3: Macroscopic aspect
Biological tests had shown severe anemia with a hemoglobin level of 6 g/dl. Pelvic ultrasound could not identify the uterus in the pelvic region. MRI could not be done in this patient due to lack of financial means. In total we diagnosed a third degree non- puerperal uterine inversion.We performed medical resuscitation and then removal of the mass vaginally followed by an upper inter- adnexal hysterectomy after reintegration of the uterus by the same procedure described above (Figure 3B).
Case 3
This was a G7P7 of 47 years old, with no particular pathological history, who had consulted for abdominal and pelvic pain and metrorrhagia.
Clinical examination revealed a third-degree uterine inversion with a mass appended to the uterine fundus (figure 4A).
- Histology of the biopsy specimen: fleshy bud
- Pelvic ultrasound: uterus not visualized; rounded anechoic image with sharp storytellers, sitting behind the cystic bladder about 5 cm long; bladder normal-looking; ovaries not visualized
The diagnosis of a type 4 uterine inversion associated with an ovarian cyst was made.
Management included a hysterectomy with bilateral adnexectomy in two stages:
- First stage: abdominal approach (Figure 4B):
- Midline sub umbilical incision
- Investigation: uterus not visualized; adnexa sucked towards the vagina with the presence of a serous left ovarian cyst.
- Gesture: ligation and bilateral section of lumbo-ovarian pedicles and round ligaments
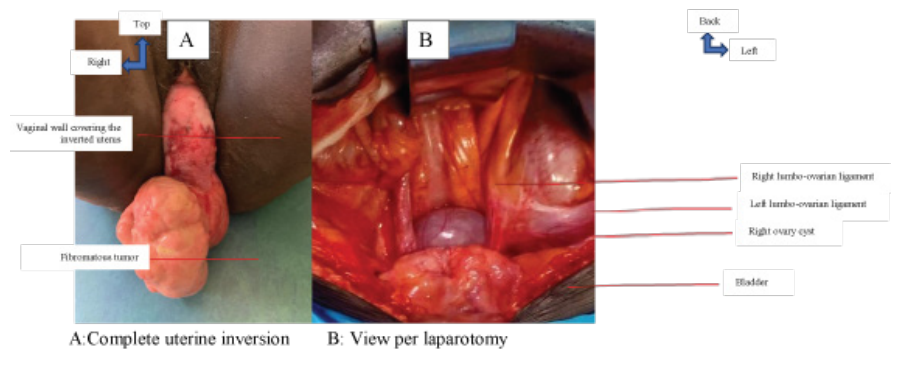
Figure 4: Macroscopic aspect
- Second stage: lower approach; sectioning of the uterus at the level of the isthmus allowing a subtotal hysterectomy to be performed, then removal of the vagina and the remaining cervix allowing an anatomical reconstruction to be made.
- Third stage: abdominal route to complete total hysterectomy Surgical suites were simple Histological examination of the surgical specimen came back in favor of a uterine myoma.
Discussion
Non-puerperal uterine inversion is a rare situation. It occurs most often in patients who are postmenopausal or over 45 years of age. Between 1976 and 2014, only fifty-six cases have been reported in the literature, mainly in women who are postmenopausal or over 45 years of age [1]. In our series, the 2 patients were over 45 years of age (47 and 40 years) and the other was 28 years old.
Several factors are involved in the pathophysiology of nonpubertal uterine inversion: the presence of a uterine tumor located preferentially on the uterine fundus; on a thin uterine wall; with a small tumor pedicle; rapid tumor growth; and cervical dilatation by distension of the uterine cavity [1].
Non-puerperal uterine inversion may be idiopathic or associated with predisposing factors such as benign uterine tumors in 70-80% of cases such as leiomyomas as in our last 2 cases, endometrial polyps (case 1), or a malignant tumor in the remainder, especially in young women (leiomyosarcoma, rhabdomyosarcoma, carcinoma of the endometrium and cervix)[2]. The only young patient in our series was 28 years old and had a benign uterine tumor (Benign Endometrial Polyp)
There are two types of uterine inversion: puerperal and non- puerperal or gynecological. Depending on the severity, there are four degrees [3]: first degree: the uterine fundus is depressed in a "vial bottom" or cup; second degree: the inverted uterus crosses the external orifice of the cervix; third degree: the uterine body becomes intravaginal and can completely externalize; fourth degree or total inversion: the vaginal walls participate in the inversion. Several treatments have been described in the literature: conservative treatment when reduction of uterine inversion is possible, mainly in case of uterine inversion of the 1st or 2nd degree; third degree: the uterine body becomes intravaginal and may completely externalize; fourth degree or total inversion: the vaginal walls participate in the inversion.
Uterine inversion is suspected when a tumor is palpated in the vagina and the uterine fundus is not accessible to pelvic palpation.
If the diagnosis is easy in the complete forms (3rd and 4th degree) by visualization of a reddish externalized mass reminiscent of the endometrium on the speculum, with a vaginal touch associated with abdominal palpation of the absence of uterine fundus, incomplete forms are radiologically diagnostic [4].
Imaging can be of significant value in types 1 and 2.Transvaginal ultrasound shows only the mass. Transabdominal ultrasound usually shows a mass at the cervico-vaginal level, and uterine morphology is difficult to define because of the mass. However, two signs are described: the indentation of the fundal area and the depressed longitudinal groove extending from the fundus to the center of the inverted part [5,6].
MRI is an examination of choice in diagnosis because it allows examination of the characteristic image of uterine inversion. Lewin et al. reported that, in T2-weighted MRI scans, a U-shaped uterine cavity and a thickened and inverted uterine fundus on a sagittal image and a bull's-eye configuration on an axial image are signs indicating uterine inversion [7].
Management is surgical and depends on age, parity, degree of inversion and, above all, etiology.In young women with a suspected benign tumor, conservative treatment will be continued until histopathology confirms the benign nature of the mass; this attitude was adopted for this case. Biopsy of the mass is always necessary regardless of the age prior to surgery.
Studies have shown that there is no obstetrical impact after this surgical correction of the inversion [8]. In all other cases, treatment will usually consist of a hysterectomy (cases 2 and 3). The hysterectomy is performed vaginally, exposing the operator to technical difficulties due to changes in the usual anatomical landmarks, particularly with regard to the excretory urinary tract (ureters and bladder). The abdominal route gives greater accessibility but requires reduction of the inversion with restitution of the uterus into the pelvic cavity.
In our three patients, the management was radical in two of the three and conservative with a vaginal and abdominal approach.
Conclusion
Non-puerperal uterine inversion is rare. Diagnosis is easy in the complete forms, this during imaging is of real benefit in stages 1 and 2. The treatment is surgical and will be conservative or radical depending on the subsequent desire for pregnancy and the malignant or benign nature of the cause.
References
- Lupovitch A, England ER, Chen R. Non-puer- peral uterine inversion in association with uterine sarcoma: case report in a 26-year-old and review of the Gynecol Oncol. 2005; 97: 938-941.
- de Vries M, Perquin DAM. Non-puerperal uterine inversion due to submucous myoma in a young woman: a case J Med Case Reports déc. 2010; 4: 21.
- http://www.syngof.fr/~syngof/fmc/inversion.html.2000
- Miras T, Collet F, Seffert Acute puerperal uterine inversion: two cases. J Gynecol Obstet Biol Reprod (Paris). 2002; 31: 668-671.
- Chou HH, Chen CJ, Chu KK. Ultrasonogra- phy diagnosis in subacute uterine inversion- a case report. Changgeng Yi Xue Za Zhi. 1995; 73-76.
- Hsieh TT, Lee JD. Sonographic findings in acute puerperal uterine inversion. J Clin Ultrasound. 1991; 19: 306-309.
- Lewin JS, Bryan PJ. MR imaging of uterine inversion. J Comput Assist Tomogr. 1989; 13: 357-359.
- Sinha G, Sinhan A. Fertility and reproduction following inversion of 17 the uterus. Juin. 1993; 96: 149-150.