Nutritional Status Assesment of The Type 2 Elderly Diabetic Patient
Author'(s): Hasna Ballaziri, Nassim Essabah Haraj, Siham El Aziz, and Asma Chadli*
Endocrinology-Diabetology and Metabolic Diseases Department, University Hospital Ibn Rochd, Morocco.
Laboratory of Neuroscience and Mental Health, Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco.
*Correspondence:
Asma Chadli, Endocrinology and Diabetology Department. Ibn Rochd University Hospital of Casablanca, Casablanca, Morocco, Tel: +212 6 61092820; E-mail: drachadli@gmail.com.
Received: 30 June 2019 Accepted: 25 July 2019
Citation: Hasna Ballaziri, Nassim Essabah Haraj, Siham El Aziz, et al. Nutritional Status Assessment of The Type 2 Elderly Diabetic Patient. Diabetes Complications. 2019; 3(3): 1-5.
Abstract
Aims: To assess the nutritional status of elderly type 2 diabetes (T2D) patients, to describe the undernutrition prevalence level and understand the driving factors.
Methods: Our study included 300 elderly T2D patients who were hospitalized in our unity, between 2016-2017. The assessment tool used was the Mini Nutritional Assessment (MNA).
Results: Patients’ average age was 71.7 years with a sex ratio of 0.68. Glycemic control was satisfactory within 39.7% of patients, two-thirds of them were treated by insulin therapy and more than half of them were following specific diets. Oral disorders were present within 63% of patients. Half were polymedicated and 15.33% weren’t autonomous. The MNA found that 14.33% of our patients were malnourished, 47.67% were at risk of malnutrition, whereas 38% had a satisfactory nutritional status. A positive correlation was found between poor nutritional status and advanced age, male sex, BMI, a restrictive diet, microangiopathy, loss of autonomy, oral and swallowing disorders. We did not find any correlation with the socio-economic level, diabetes duration, macroangiopathy, and polymedication.
Conclusion: Elderly diabetic patients’malnutrition increase morbidity and mortality, so it is important to evaluate their nutritional status in order to detect and treat an early malnutrition state for a better overall management.
Keywords
Introduction
Protein-energy malnutrition is a common pathology in the elderly [1]. This is a real public health problem, with particularly harmful consequences in this population [2]. Malnutrition in the elderly diabetic subject, despite being frequent, is often underestimated because systematic nutritional assessment is not a routine practice yet. The nutritional management is therefore often omitted, insufficient or even inadequate. Several tools have been proposed for assessing nutritional status in the elderly [3,4]. This raised the problem of choosing a valid test that is easy to perform (without requiring a paraclinical check-up) while maintaining reliable results. As a result, Mini Nutritional Assessment (MNA), which is recommended by the European Society of Parenteral and Enteral Nutrition (ESPEN) for the assessment of nutritional status for old patients in all health care centers (5), appears ideal for the elderly diabetic patient.
In search of these factors, we conducted a descriptive observational study using the MNA as a tool, with 300 diabetic patients whose age is 65 years and over, hospitalized or followed up in consultation at the Endocrinology, Nutrition and Metabolic Diseases Department of the IBN ROCHD University Hospital of Casablanca. The main objective of our study is to assess the nutritional status of the elderly diabetic type 2 patients, as well as describe the prevalence of undernutrition and to determine the factors influencing this problem.
Patients and Methods
This was a study involving 300 patients with type 2 diabetes (T2D) aged 65 years and older. The participants were recruited from the consultation or were hospitalized in the Endocrinology, Nutrition and Metabolic Diseases Department of the IBN ROCHD University Hospital in Casablanca, over a year period, from November 2016 to November 2017.
Inclusion criteria
- T2D patient, aged 65 years and older.
- Hospitalized patient or consultant within our unit
- Patient hospitalized in any department of our University Hospital that has requested an interdepartmental endocrinological opinion.
Exclusion criteria
- Patient less 65 years of age.
- Patient with another type of diabeties.
We carried out the data collection using a pre-established form with two sections: a first section with questions related to the patient’s clinical characteristics (anthropo-demographic data, diabetes- related data, cardiovascular risk factors, and other comorbidities) and a second section with the MNA questionnaire. The parameters and measurements related to the study were taken on site during a brief clinical examination (weight, brachial circumference, calf circumference, blood pressure, capillary blood glucose).
At the end of this analysis, 3 groups were selected: Group 1 of subjects with normal nutritional status (MNA score between 24 and 30), Group 2 of subjects at risk of malnutrition (MNA score was between 17 and 23.5), Group 3 of malnourished subjects (MNA score was below 17).
We performed the statistical analysis using Microsoft Excel software. We used the Epi.info 6.0 software for the data collected subsequently. Finally, we used a Chi 2 test to obtain "p". A value of p < 0.05 was considered statistically significant.
Results
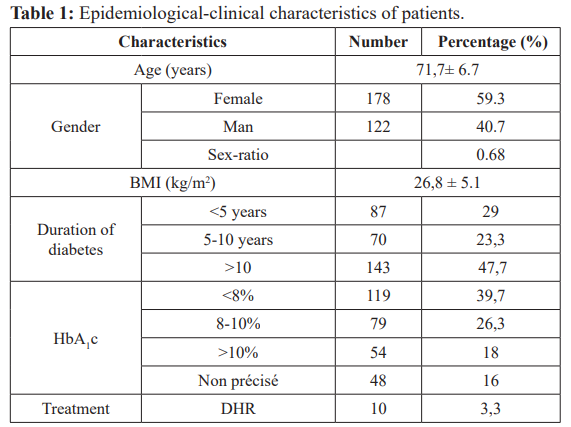
Table 1 summarizes the epidemiological and clinical characteristics of the patients studied.
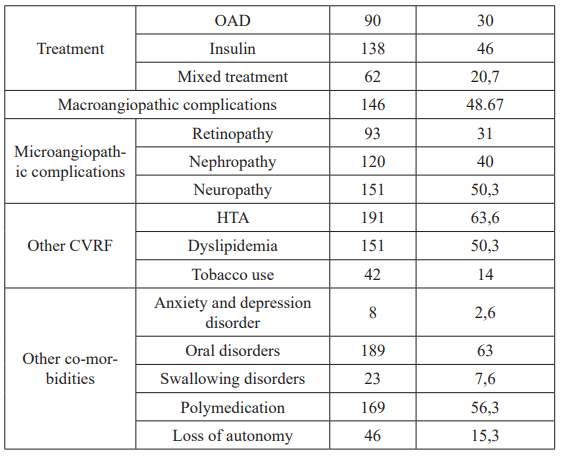
Our patients were divided into 3 groups according to the number of points obtained following the MNA questionnaire (Figure 1).
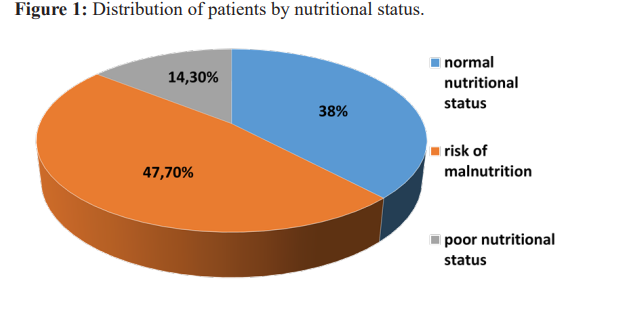
Table 2 shows the comparison of the epidemiological and clinical characteristics of the three patient groups and the correlation between the normal nutritional status group and the undernourished patient group.
The risk of malnutrition was associated with the age extremes of the study population (> 80 years: p= 0.002 and <70 years: p=0.003), male sex (p=0.04), leanness (p=0.00001) and obesity (p=0.0005). Regarding the complications of diabetes, the presence of diabetic nephropathy (p=0.001), digestive autonomic neuropathy (p=0.03) and urinary neuropathy (p=0.02) were associated with malnutrition among our patients.
Also, the association of diabetes with other cardiovascular risk factors such as dyslipidemia (p=0.009) and smoking (p=0.003), the frequency of oral disorders (p=0.0005) or swallowing disorders (p=0.0001) constituted risk factors for malnutrition. We also found a significant positive association (p = 0.0000000001) between the loss of autonomy and the nutritional status of our patients.
Table 2: Comparison of the characteristics of the three patient groups and correlation between group 1 and group 3.
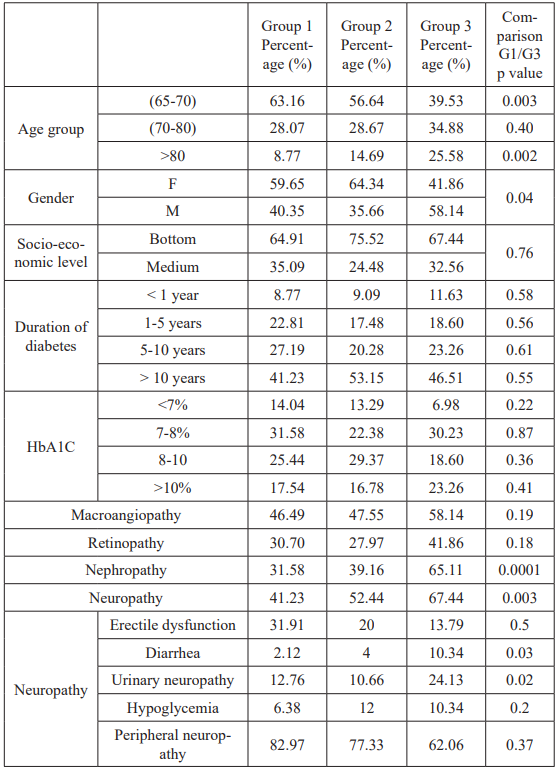
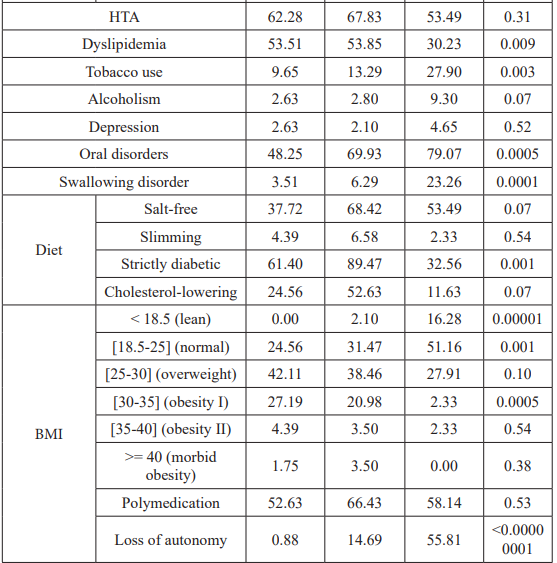
Table 2: Comparison of the characteristics of the three patient groups and correlation between group 1 and group 3.
Discussion
T2D is the most common form of diabetes mellitus in the world; its prevalence increases with the ageing of the population. According to the latest report of the IDF (International Diabetes Federation), the number of people aged 65-99 with diabetes in 2017 was 122.8 million, representing a prevalence of 18.8%. Forecasts according to this trend estimate that this number will reach 253.4 million by 2045 [6].
The nutritional needs of this fragile population are generally equivalent to those of adults and increase in intercurrent stress situation. Dietary intakes must cover total energy expenditure [7]: 30 kcal/kg/day, or 2200 kcal/d for a 70 kg man and 1800 kcal/d for a 60 kg woman. A daily energy intake less than 1500 kcal exposes to the risk of malnutrition with the following consequences: tissue loss, including muscle loss (muscular atrophy) resulting in alteration of the organism's ability to respond to certain aggressions (infections) and autonomy’s decrease. This malnutrion of the senior subject was responsible for an aggravation for the state of fragility already established by the physiological process of ageing. Its consequences have repercussions on the whole organism. This morbidity aggravates the prognosis of underlying diseases and thus increases the risk of death [8].
The clinical criteria for undernutrition are based on a set of anthropometric tools that are not used for diagnosis but rather for screening. They help to assess the nutritional status of a subject from comparing the values found at reference values and/or comparison of measurements in the same individual over time [9]. We distinguish: weight, BMI, skin folds and circumference measurement. The biological markers of undernutrition find their interest in screening for undernutrition at an infra-clinical stage and the follow-up of a process of correcting it. They are also used in the construction of scores and index of malnutrition. We distinguish four serum proteins (albumin, transthyretin or prealbumin, transferrin and retinol carrier protein) [10], 24- hour creatinuria, urea and lymphocyte assay. Given the lack of sensitivity and specificity of the various clinical and biological markers mentioned above, several indexes or scales for screening for undernutrition have therefore been developed, raising the question of the validity, sensitivity and specificity relative to each other depending on the clinical context of the patient [11].
The MNA was developed to detect undernutrition specifically in elderly subjects [12]. It consists of a questionnaire of 18 items based on the interrogation and measurement of anthropometric parameters. It has been validated by several scholarly societies as a tool for the diagnosis of malnutrition. Most of the studies that assessed the nutritional status of the elderly diabetic patients used the MNA as an assessment tool [3,4,13,14].
In the literature, the prevalence of malnutrition in elderly diabetic patients in hospital varies from 5.3 to 22.8% (Table 3). A case- control study comparing the nutritional status of older diabetic and non-diabetic patients has showed a significantly lower score of the MNA in diabetic patients compared to the control group

Table 3: Prevalence of malnutrition in elderly diabetic patients according to various studies.
[15]. Several authors had evoked diabetes as a risk factor for malnutrition [13,16-18]. Concerning the duration of diabetes, Sanz Paris and his colleagues [3,4], found a positive association between poor nutritional status and duration of diabetes ≥ 10 year. Contrary to the results of the Chinese study conducted by Liu GX and his colleagues [13], as well as that one conducted by Doostan and his colleagues [14], who did not find a statistically significant association between the duration of diabetes and the nutritional status of patients. Several authors have also demonstrated that restrictive diets within older subjects in general represent an important factor leading to malnutrition [18,19]. Morley [20], places particular emphasis on hyposodium and hypocholesterolemic diets.
Concerning the chronic complications of diabetes and the risk of malnutrition, the study carried out by Sanz-Paris and al. found a positive association between malnutrition and the presence of diabetic complications, both macro and microangiopathics (OR = 1,973; 95% CI: 1,519-2,563). These results are consistent with those of the study conducted by Gong-Xiang and al. which found a correlation between malnutrition and complications, particularly microvascular complications of diabetes (OR = 2.89; 95% CI: 1.50-5.57). On the other hand, the study conducted by Doostan and al. in 190 elderly diabetic patients did not confirm this association. Some studies have associated poor nutritional status with advanced age, both in diabetic [6,13] and non-diabetic patients [18,21]. In addition, data from the literature correlate the sex gender as an isolated factor in the risk of malnutrition in the elderly are rare [28- 30]; some studies have shown a higher prevalence of malnutrition or involuntary weight loss for males [21-25]. Other risk factors have been implicated, including the presence of oral disorders [26- 29], malnutrition and depression [20,30,31-33] or malnutrition and anxiety [34,35]. Our results are consistent with the literature on the loss of autonomy or dependence on the daily life activities as the determinant factors associated to the nutritional status, for both the malnutrition status (p<0.00000001) and malnutrition risk (p=0.00009). This loss / lack of autonomy is most often one of the factors most significantly associated with malnutrition in the elderly [21,36-38].
Conclusion
Nutritional status assessment in elderly patients especially diabetic ones stays an often-neglected exercise in common practice. However, it remains clear, that this evaluation has to be taken into consideration, due to the high prevalence of undernutrition and the risk of malnutrition in this population. Several authors and societies validated the MNA, as a practical screening test, fulfilling the criteria of validity and ease of use for assessment of nutritional status in the elderly diabetic patients. Our study, through the research of the various factors involved in malnutrition among the elderly diabetic patients, gives substance to the establishment of a systematic global and individualized approach to the nutritional management of each diabetic elderly patient.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- Patry C, Raynaud-Simon Prise en charge de la dénutrition chez les personnes âgées: quoi de neuf depuis les recommandations de l’HAS en 2007 ?. Neurologie - Psychiatrie - Gériatrie. 2011; 11: 95-100.
- Organisation mondiale de la Santé. Rapport mondial sur le diabète, Genève.
- Sanz Paris A, Gomez-Candela C, Martin-Palmero A, et al. Application of the new ESPEN definition of malnutrition in geriatric diabetic patients during hospitalization: A multicentric Clinical Nutrition. 2016; 35: 1564-1567.
- Sanz Paris A, Garcia JM, Gomez-Candela C, et Malnutrition prevalence in hospitalized elderly diabetic patients. Nutr Hosp. 2013; 28: 592-599.
- Kondrup J, Allison SP, Elia M, et al. ESPEN guidelines for nutrition screening 2002. Clinical Nutrition. 2003; 22: 415-
- Fédération Internationale du Diabète. Atlas du diabète de la FID, Huitième édition 2017.
- Collège National des Enseignants de Gériatrie. Nutrition et malnutrition du sujet âgé. Collège National des Enseignants de Gériatrie. Vieillissement. Masson, Paris. 2007; 99-116.
- Haute Autorité de Santé. Stratégie de prise en charge en cas de dénutrition protéino- énergétique chez la personne âgée (Argumentaire).
- Corish CA, Kennedy Protein-energy undernutrition in hospital in-patients. Br J Nutr. 2000; 83: 575-591.
- Lamisse F. Évaluation de l’état nutritionnel péri-opératoire. Cah Nutr Diét. 1995; 30: 278-282.
- Kondrup J, Rasmussen HH, Hamberg O, et Ad Hoc ESPEN working group. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clinical Nutrition. 2003; 22: 321-336.
- Guigoz Y, Vellas Test d’évaluation de l’état nutritionnel de la personne âgée : le Mini Nutritional Assessment (MNA). Méd Hyg. 1995; 53: 1965-1969.
- Liu GX, Chen Y, Yang YX, et al. Pilot study of the mini nutritional assessment on predicting outcomes in older adults with type 2 diabetes. Geriatr Gerontol Int. 2017; 17: 2485-
- Doostan F, Sa zadeh H, Kazemzadeh H, et al. Nutritional Status and Its Associated Factors in Elderly with Diabetes, 2015 (Persian). Iranian Journal of 2016; 11: 384-391.
- Turnbull P, Sinclair Evaluation of nutritional status and its relationship with functional status in older citizens with diabetes mellitus using the Mini Nutritional Assessment (MNA) tool. A preliminary investigation. J Nutr Health Aging. 2002; 6: 185-189.
- Hickson M. Malnutrition and ageing. Postgrad Med J. 2006; 82: 2-8.
- Nazemi L, Skoog I, Karlsson I, et , Malnutrition, Prevalence and Relation to Some Risk Factors among Elderly Residents of Nursing Homes in Tehran, Iran. Iran J Public Health. 2015; 44: 218-227.
- Newman AB, Yanez D, Harris T, et al. Weight change in old age and its association with J Am Geriatr Soc. 2001; 49: 1309-1318.
- Zeanandin G, Molato O, Le Duff F, et Impact of restrictive diets on the risk of undernutrition in a free-living elderly population. Clinical Nutrition. 2012; 31: 69-73.
- Morley JE. Anorexia of aging: physiologic and pathologic. Am J Clin Nutr. 1997; 66: 760-773.
- Woo J, Ho SC, Sham A. Longitudinal changes in body mass index and body composition over 3 years and relationship to health outcomes in Hong Kong Chinese age 70 and older. J Am Geriatr 2001; 49: 737-746.
- Fávaro-Moreira NC, Krausch-Hofmann S, Matthys C, et al. Risk Factors for Malnutrition in Older Adults: A Systematic Review of the Literature Based on Longitudinal Data. Adv 2016; 7: 507-522.
- Rist G, Miles G, Karimi The presence of malnutrition in community-living older adults receiving home nursing services. Nutrition & Dietetics. 2012; 69: 46-50.
- Schilp J, Kruizenga HM, Wijnhoven HA, et High prevalence of undernutrition in Dutch community-dwelling older individuals. Nutrition. 2012; 28: 1151-1156.
- Kaiser MJ, Bauer JM, Ramsch C, et Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010; 58: 1734-1738.
- Lamy M, Mojon P, Kalykakis G, et Oral status and nutrition in the institutionalized elderly. J Dent. 1999; 27: 443-448.
- Paillaud E, Merlier I, Dupeyron C, et al. Oral candidiasis and nutritional deficiencies in elderly hospitalised patients. Br J 2004; 92: 861-867.
- Daly RM, Elsner RJ, Allen PF, et al. Associations between self-reported dental status and diet. J Oral Rehabil. 2003; 30: 964-970.
- Budtz-Jorgensen E, Chung JP, Rapin CH. Nutrition and oral Best Pract Res Clin Gastroenterol. 2001; 15: 885-896.
- Saka B, Kaya O, Ozturk GB, et Malnutrition in the elderly and its relationship with other geriatric syndromes. Clin Nutr. 2010; 29: 745-748.
- Tamura BK, Bell CL, Masaki KH, et al. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: A systematic review of the literature. J Am Med Dir 2013; 14: 649-655.
- Smoliner C, Norman K, Wagner K-H, et al. Malnutrition and depression in the institutionalised elderly. Br J Nutr. 2009; 102: 1663-1667.
- Yoshimura K, Yamada M, Kajiwara Y, et al. Relationship between depression and risk of malnutrition among community- dwelling young-old and old-old elderly people. Aging Ment 2013; 17: 456-460.
- Patel MD, Martin FC. Why don’t elderly hospital inpatients eat adequately? J Nutr Health 2008; 12: 227-231.
- Ribeiro RSV, da Rosa MI, Bozzetti MC. Malnutrition and associated variables in an elderly population of Criciúma, Rev Assoc Med Bras. 2011; 57: 56-61.
- Donini LM, Scardella P, Piombo L, et al. Malnutrition in elderly: Social and economic determinants. J Nutr Health 2013; 17: 9-15.
- Mitri R, Boulos C, Adib SM. Determinants of the nutritional status of older adults in urban Lebanon. Geriatr Gerontol Int. 2017; 17: 424-432.
- Fanello S, Foucault S, Delbos V, et al. Évaluation de l’état nutritionnel de la personne âgée hospitalisée. Santé publique. 2000; 12: 83-90.