Outcome of Umbilical Cord Prolapse in A Tertiary Health Centre in Northwestern Nigeria
Author’(s): Burodo Ahmed Tanko1, Nnadi Daniel C1, Umar Amina Gambo1, Ibrahim Rukayya1, Ladan Ashiru A2, Garba Jamila Abubakar1, and Rabiu Anas Funtua1
1Usmanu Danfodiyo University Teaching Hospital Sokoto.
2Federal Medical Center Birnin Kebbi.
*Correspondence:
Garba Jamila Abubakar, Department of Obstetrics and Gynaecology, Usmanu Danfodiyo University Teaching Hospital Sokoto, 09031239328, E-mail: jgarba80@gmail.com.
Received: 13 August 2020 Accepted: 01 September 2020
Citation: Burodo A T, Nnadi D C, Umar A G, et al. Outcome of Umbilical Cord Prolapse in A Tertiary Health Centre in Northwestern Nigeria. Gynecol Reprod Health. 2020; 4(4): 1-4.
Abstract
Background: Umbilical cord prolapse (UCP) is the presence of a loop of umbilical cord below the presenting part with ruptured membranes which is an obstetric emergency associated with increased fetal morbidity and mortality and also maternal morbidity.
Objectives: The aim was to determine the incidence; risk factors and complications of umbilical cord prolapse.
Materials and Method: This was a cross sectional case study carried out to review all cases of umbilical cord prolapse managed at Usmanu Danfodiyo University Teaching Hospital Sokoto from 1stJanuary, 2006 to 31st December, 2015. Statistical analysis was done using SPSS version 22.
Results: There were 48 cases of UCP and 29,743 deliveries. The incidence of UCP was 0.16% of the deliveries. Among the cases, 83.3% had emergency caesarean section. This accounted for 1% of the total 3,982 caesarean section during the study period. Prematurity was the most common identified risk factor and accounted for 20.8% of cases while six patients had transverse lie which account for 12.5%. Twin gestation and breech presentation occurred in 4.2% and 8.3% of cases respectively. There was no risk factor was identified in 37.5%. In 62.5% of cases, the UCP occurred at term. In 45.8% of cases, the babies were between s1.5-2.5kg and 41.7% weighed 2.5kg or more. There were 70.8% live births and 29.2% stillbirths.
Conclusion: The incidence of UCP was 0.16%. Prematurity was the most common identified risk factor and there was prompt and appropriate management of the cases of umblical cord prolapse.
Keywords
Introduction
Umbilical cord prolapse (UCP) is defined as the presence of a loop of umbilical cord below the presenting part with ruptured membranes [1]. Prolapse of the umbilical cord is an obstetric emergency associated with increased fetal morbidity and mortality and also maternal morbidity [1]. It is overt if the cord is seen within the cervix or in the vagina, whereas occult cord prolapse is when it is compressed between the uterine wall and the fetal part [2,3]. This compromises foetal circulation and depending on the duration and intensity of compression, may lead to foetal hypoxia, brain damage and death [1].
The incidence of umbilical cord prolapse as quoted in several studies varies between 0.1% and 0.6%4-6. The prevalence of umbilical cord prolapse as well as the perinatal mortality rate associated with umbilical cord prolapse has been noted to be declining in the last seven decades due to increase in use of elective caesarean section in non-cephalic presentations, and the more rapid and frequent recourse to caesarean section once cord prolapse is diagnosed [6].
Cord prolapse is associated with all factors maintaining the presenting part above the pelvis. Predisposing factors include the following conditions: Unengaged presenting part, malpresentations, prematurity, multiple pregnancy and polyhydramnios [1]. Prematurity is also a major risk factor for UCP because the fetuses are often small and in a nonvertex presentation [7-9]. UCP is associated with adverse neonatal outcomes, such as low Apgar scores and low cord pH values [10-12]. There is also a significant increased risk of mortality in babies born following UCP.
The optimal management is prompt delivery to avoid foetal death from cord compression [7]. Measures to alleviate compression on the prolapsed cord must be carried out until emergency delivery of the baby can be affected [8]. Various resuscitative measures such as, giving oxygen to the mother, manual elevation of the presenting part above the pelvic brim, inflating the bladder with 500-600mls of normal saline with the aim of inhibiting uterine contractions and elevating the presenting part have been applied following diagnosis, while preparing for emergency delivery in a life foetus [12-14]. These actions singly or in combination will raise the presenting part off the cord and reduce the uterine activities. Provided the cervix is not completely dilated, prompt delivery through caesarean section offers the best chance for a favourable foetal outcome [9]. In cases where patients however present with a completely dilated cervix, the obstetrician has a choice between instrumental vaginal delivery and caesarean section. Several studies have quoted more favourable foetal outcome with c/s in the second stage of labour [6]. If the foetus is dead, cord prolapse may be ignored and vaginal delivery should be aimed at except if there is mechanical problem such as inadequate maternal pelvis, malposition or malpresentation [7]. The perinatal mortality and morbidity due to cord prolapse has significantly improved over past century as a result of advances in labour management, improved surgical techniques and neonatal intensive care [5]. However, studies have revealed that perinatal outcome can further be improved by a multi-professional obstetric emergency training session [10].
Aim and Objectives
This study is aimed to determine the prevalence, risk factors and complications of umbilical cord prolapsed.
Materials and Method
This was a retrospective cross-sectional study carried out to review all cases of umbilical cord prolapse managed at Usmanu Danfodiyo University Teaching Hospital Sokoto between January 2006 to December 2015. The sources of the data were the labour ward birth records, theatre operation register and patient case files. Information obtained from the records were age, parity, gestational age, booking status, risk factors, cervical dilatation at presentation and the mode of delivery. Data were also collected on the number of foetuses (singleton or multiple), foetal presentation, Apgar score at the first and fifth minutes, birth weight and feotal outcome. In cases of twin pregnancy, only the parameter on the foetus with a prolapsed cord was included in the study. Of the 64 cases of umbilical cord prolapse recorded over the study period, 48 case files wereavaibleforreviewandformthebasisforanlysis. All patients that presented with live foetuses had either manual elevation of thepresenting part, maternal headdown positioning or instillation of 500 mls of normal saline into thematernal bladder Statistical analysis was done using SPSS version 23. A P value of <0.05 was considered significant at 95% confidence interval (CI).
Results
During the study period, there were 65 cases of umblical cord prolapse (UCP), however only 48 files were available for review among 29,743 deliveries. The incidence rate of UCP was 0.16% or 1 in 619 deliveries. Of the 48 cases, 40 (83.3%) had emergency c/s. This accounted for 1% of the total 3,982 caesarean section during the study period. Figure 1 shows the mode of delivery of the cases.

Figure 1: Mode of the delivery of the cases
Table 1 shows the age, parity and booking status of patients with umbilical cord prolapse. The ages of the patients ranged from 15 to 40 years. Patients in the age range of 25- 29 years had the highest incidence of cord prolapse (41.7%). The women between P1-4 constituted 83.3%. Twenty patients (41.7%) were unbooked.
Figure 2 shows the risk factors identified in the patients with cord prolapse. Prematurity accounted for 20.8% of cases while six patients had transverse lie which account for 12.5%. Twin gestation and breech presentation occurred in 4.2% and 8.3% of cases respectively. In 37.5% of cases, no risk factor was identified.
Table 2 shows the gestational age of the fetuses at the time of cord prolapse. The gestational age range between 28- 42 weeks. In 62.5% of cases, the UCP occurred at term. Eighty seven percent of patients presented with cervical dilatation of <8cm.in 45.8% of cases, the babies were between the range of 1.5-2.5kg and 41.7% weighed 2.5kg or more. Of the 48 cases of UCP, 34 (70.8%) were alive while 14 (29.2) were dead. The perinatal mortality is therefore 21.5%.
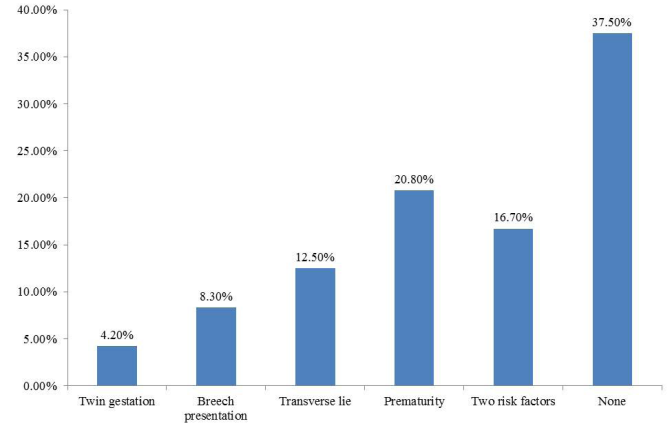
Figure 2: Risk factors identified in the patients with cord prolapse

Table 1: Age distribution, parity and booking status of the parturients.
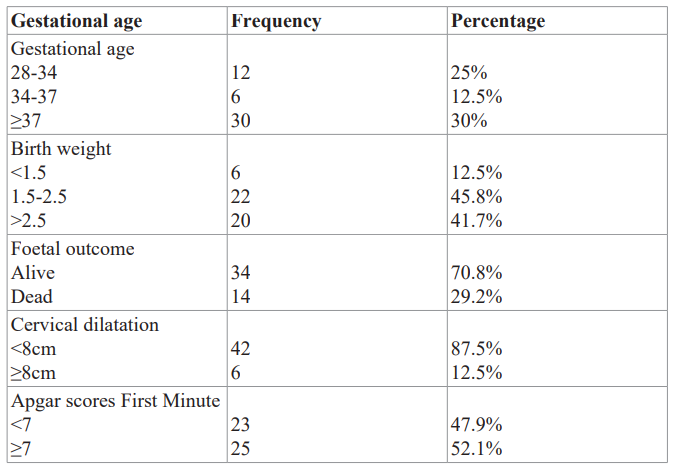
Table 2: Gestational age of the fetuses at the time of cord prolapse
Discussion
UCP is an obstetric emergency and is associated with significant neonatal morbidity and mortality if prompt and adequate management is not instituted. Patients with UCP can expect good neonatal outcome if intervention is prompt.
The incidence of cord prolapse varies worldwide, with quoted rate of between 1 in 200 and 1 in 700 [4-6]. In this study, the incidence of 1 in 619 deliveries (0.16%) was found. This is similar to the study in Kaduna [12], Nigeria with an incidence 0.19% or 1 in 526 deliveries, but lower than the study in Jos [15], Nigeria with an incidence of 1 in 358 deliveries or 0.28% and Calabar [4] with an incidence of 0.31%. Other studies done in southern part of Nigeria showed higher incidences [5,9]. This may be due to differences in both health-seeking behaviour and use of antenatal services among women in northern and southern part of the country.
Multiparous women were responsible for 77% of all the cases of cord prolapse in this study which is similar to the study done in Kano, Kaduna and Calabar [4,6,12], Nigeria. This was however less than the 94.3% reported in Jos [15], Nigeria. The higher incidence found in multipara in this study may be due to the lax anterior abdominal wall that encouraged the occurrence of malpresentation, unstable lie or an unengaged head in labour.
Twenty-eight (58.3%) of the patients in this study were booked. This is contrary to findings in other studies where association between UCP and unbooked status were documented. Most patients with the UCP occurred outside the hospital. The high prevalence among booked cases may be due to a delay in reaching the hospital after the membranes have ruptured.
There is therefore the need to educate women during health talk at the antenatal clinic (ANC) on early presentation to the hospital in labour especially after the membranes have ruptured. Educating the women on proper positioning should cord prolapse occur outside the hospital setting such as the lateral positioning with pelvic elevation or the knee-chest positioning is also important. The later though may not be feasible especially during transportation to the hospital.
The perinatal mortality rate in this study is 21.5%.This confirms cord prolapse as an obstetric emergency that courses higher perinatal mortality. However, the perinatal mortality has been found to be declining due to increase in use of elective caesarean section in non-cephalic presentations, and the more rapid and frequent recourse to caesarean section once cord prolapse is diagnosed [6]. Perinatal outcome is improved in women were the UCP occurs within the hospital. In this study, 34 fetuses (70.8%) were alive. All dead fetuses were intrauterine death at presentation.
UCP is common in conditions were the presenting part is not well applied to the cervix. The most common risk factor identified in this study was prematurity (20.8%). This is followed by transverse lie (12.5%). This is similar to several studies [5,6,9].
Emergency caesarean section was the commonest mode of delivery among patients with cord prolapse in this study accounting for 83.3%. All the patients who presented with cord prolapse and live foetus had emergency caesarean section. The finding is similar to some studies in Nigeria [6,9]. None of this patient presented in second stage of labour with live foetus to warrant instrumental vaginal delivery.
Conclusion
This study has shown that the incidence of umbilical cord prolapsed is 0.16% and prematurity is the commonest risk factor associated with umbilical cord prolapse. Perinatal mortality is low due to early interventions which lead to a live birth.
References
- Kwawukume EY. Cord Prolapse. In: Kwawukume EY, Emuveyem EE (eds). Comprehensive Obstetrics in the Tropics. 1st ed. Dansoman: Ashante and Hittscher Printing Press Ltd. 2002; 208-210.
- Kish K. Malpresentation and Cord Prolapse. In: Decherney AH, Nathan L, Laufer N, Roman AS (ed). Current Obstetric and Gynecologic Diagnosis and Treatment. 11th ed. New York: Lange Medical Books. 2013; 317-333.
- Dilbaz B, Ozturkoglu E, Dilbaz S, et al. Risk factors and perinatal outcomes associated with umbilical cord prolapse. Arch Gynaecol Obstet. 2006; 274: 104-107.
- Emechebe CI, Njoku CO, Anachuna K, et Determinants and Obstetric Outcome of Umbilical Cord Prolapse at University of Calabar Teaching Hospital, Calabar, Nigeria. JDMS. 2015; 14: 98-103.
- Kalu CA, Umeora O. Risk factors and perinatal outcome of umbilical cord prolapse in Ebonyi State University Teaching Hospital, Abakaliki, Niger J Clin Pract. 2011; 14: 413-417.
- Umar UA, Gaya Outcome of umbilical cord prolapse at Aminu Kano Teaching Hospital, Kano, North-Western Nigeria. Niger J Basic Clin Sci. 2015; 12: 20.
- Critchlow CW, Leet TL, Benedetti TJ, et al. Risk factors and infant outcomes associated with umbilical cord prolapse: A population-based case-control study among births in Washington Am J Obstet Gynecol. 1994; 170: 613-618.
- Monique CL. Umbillical cord prolapse CME review article. Obstetrical and Gynecological Survey. 2006; 61: 269-277.
- Eleje GU, Ofojebe CJ, Udegbunam OI, et al. Determinants of Umbilical Cord Prolapse in a Low-Resource Setting. J Womens Health. 2004; 3: 1.
- https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg50/
- Sangwan V, Nanda S, Sangwan M, et Cord complications: associated risk factors and perinatal outcome. OJOG. 2011; 1: 174-177.
- Onwuhafua PI, Zayyan M, Ozed-Williams I, et al. Fetal outcome following umbilical cord prolapse in Ahmadu Bello University Teaching Hospital, Kaduna (ABUTHK), northern Nigeria. Niger J Med. 2007; 16: 334-337.
- Boyle JJ, Katz VL. Umbilical cord prolapses in current obstetric practice. J Reprod Med. 2005; 50: 303-306.
- Bord I, Gemu O, Anleby EY, et al. The value of bladder filling in addition to manual elevation of presenting foetal part in cases of cord prolapse. Archives of Gynecology and Obstetrics. 2010; 15.
- Josiah TM, Innocent AO. Fetal outcome in umbilical cord prolapse in Jos, Nigeria. Trop J Obstet Gynaecol. 2006; 23: