Perineal Tears in Childbirth
Author(s): Asma Fahad1, Laila Yahya Al Hubaishi1 and Atif Fazari1,2*
1Latifa Hospital, DHA, Dubai, UAE.
2University of Medical Sciences & Technology, Khartoum, Sudan.
*Correspondence:
Atif Bashir Fazari, Latifa Hospital, DHA, Dubai, UAE. University of Medical Sciences & Technology, Khartoum, Sudan.
Received: 28 September 2020 Accepted: 16 October 2020
Citation: Fahad A, Yahya Al Hubaishi L, Atif Fazari. Perineal Tears in Childbirth. Gynecol Reprod Health. 2020; 4(6): 1-4.
Abstract
Perineum often follow vaginal delivery and are termed as perineal tears, it’s quite common. Royal College of Obstetrics and Gynecology classified perineal tears into four grades and recommended certain steps in repair with specific sutures material, special post-operative and further follow up plan. Psychological concept of perineal. Tears and it repair, healing and outcome of this morbidity has direct impact of patient’s quality of life.
Keywords
Lower genital tract lacerations of the perineum often follow vaginal delivery and are termed as perineal tears. Over 85% of women having a vaginal birth suffer some perineal trauma. Spontaneous tears requiring suturing are estimated to occur in at least a third of women in the UK and USA, with anal sphincter tears in 0.5% to 7% of women [1]. According to the Royal College of Obstetrics and Gynecology, 9 out of 10 first time mothers will have a perineal tear [2].
Perineal tears following vaginal delivery are classified by their depth into four degrees (Table 1).
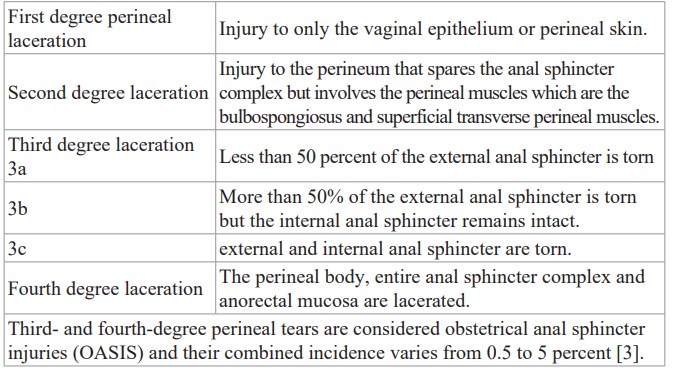
Table 1: Shows Classification of perineal tears.
Risk factors
Risk factors for these more complex lacerations include nulliparity, midline episiotomy, persistent OP position, operative vaginal delivery, Asian race, short perineal length and increasing fetal birth weight [3].
One systematic review showed that perineal tears were associated with (multivariate analysis) forceps (6.021 [IC 95% 1.23-19.45]), nulliparity (OR 9.8 [IC 95% 3.6-26.2]), gestational age over 42 SA (OR 2.5 [IC 95% 1-6.2]), fundal pressure (OR 4.6 [IC 95% 2.3-7.9]), midline episiotomy (OR 5.5 [IC 95% 1.4-18.7]) or fetal weight in interval of 250g (OR 1.3 [IC 95% 1.1-1.6]) [4].
Anal sphincter injuries are associated with greater morbidity culminating in short- and long-term symptoms.
Short term symptoms include increased rates of puerperal pain, infections, wound disruption.
Long term complications include increased rates of fecal incontinence with decreased quality of life and social problems including decreased sexuality. Timely and correct identification results in timely repair as 60-80 % of the women with obstetric anal sphincter injury will be asymptomatic at one year post- delivery [6]. The perineum should always be thoroughly assessed after a vaginal birth to determine the presence of any lacerations. This examination should include a digital rectal examination to evaluate the tone of the anal sphincter [5].
Repair
Like all surgical procedures, the repair of perineal tears should be with proper lighting, positioning with proper hygiene under aseptic conditions, ensuring good anesthesia for the patient which may be topical or by infiltration.
First degree lacerations may be repaired to control bleeding or restore anatomy. Fine gauge absorbable or delayed absorbable sutures may be used. Second degree lacerations, continuous sutures are advocated as it is faster with less pain. Commonly used materials are 2-0 polyglactin Vicryl.
Repair of third- and fourth-degree tears should be conducted by an appropriately trained clinician or by a trainee under supervision. Repair should take place in an operating theatre, under regional or general anaesthesia, with good lighting and with appropriate instruments [6].
Third degree perineal tear may be repaired using end to end technique or the overlapping method. 3-0 PDS or 2-0 polyglactin are the preferred suture material as advised by RCOG [6].
For the anal mucosa, it is advised to use 3-0 polyglactin with and end to end suturing technique, figure of eight suture should be avoided as they can cause ischemia [6].
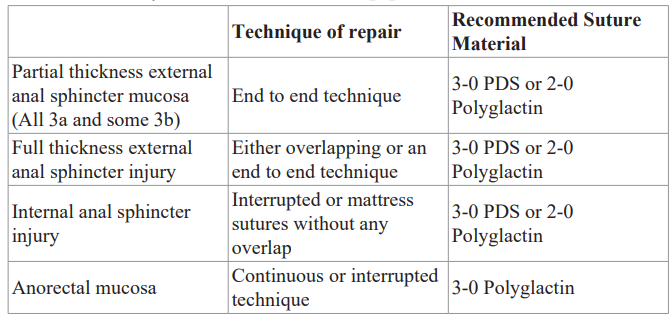
Table 2: Recommended repair technique and suture materials for obstetric anal sphincter injury as recommended by the Royal College of Obstetrics and Gynecology.
Postoperative Management
The use of broad-spectrum antibiotics is recommended following repair of obstetric anal sphincter injury to reduce the risk of postoperative infections and wound dehiscence. The use of postoperative laxatives is recommended to reduce the risk of wound dehiscence. Women should be advised that physiotherapy following repair of obstetric anal sphincter injury could be beneficial [6].
Follow up
For third and fourth degree perineal tears follow up is advised 6-12 weeks postnatal, patient should be referred to a colorectal surgeon if she is experiencing fecal incontinence. About 60-80% of the women with OASIS will be asymptomatic at one year post- delivery [6].
Future deliveries
All women who sustained OASIS in a previous pregnancy should be counselled about the mode of delivery and this should be clearly documented in the notes [6]. The role of prophylactic episiotomy in subsequent pregnancies is not known and therefore an episiotomy should only be performed if clinically indicated [6]. All women who have sustained OASIS in a previous pregnancy and who are symptomatic or have abnormal endoanal ultrasonography and/or manometry should be counselled regarding the option of elective caesarean birth [6].
Future complications
Third- or fourth-degree perineal tears that are not recognized or inadequately repaired may result in both short- and long- term complications. Short term complications such as increased hospital stay, post-operative wound infections/breakdown, more follow up visits and discomfort with reduced quality of life. Long term complications include the graver complications such as fecal incontinence rectovaginal fistulas which have a high morbidity, reducing the patient’s quality of life resulting from reduced social interactions and impaired personal relations.
Proper assessment and examination of the perineum post normal or assisted vaginal delivery with a per rectal examination is advised even if the perineum appears to be intact, as timely recognition and proper repair can help to reduce the morbidity and results in better quality of patient care.
Effect on Quality of life
While perineal tears, its diagnosis and repair has been studied in detail, there seems a paucity of information in its impact on the quality of life including the sexual life of women. According to the World Health Organization “Sexual health is a state of physical, emotional, mental and social well-being related to sexuality; it is not merely the absence of disease, dysfunction or infirmity” [7].
Resumption of sexual activity postpartum is rapid. Approximately half (52%) of women resume sexual activity by 5–6 weeks postpartum. By 3 months postpartum, 90% of women have resumed sexual activity [8,10].
In a study by Rogers et al. on the impact of genital tract trauma on postpartum sexual function, trauma was categorized into minor trauma (no trauma or first-degree perineal or other trauma that was not sutured) or major trauma (second-, third-, or fourth-degree lacerations or any trauma that required suturing). Women who underwent episiotomy or operative delivery were excluded. Fifty- eight percent (326/565) of enrolled women gave sexual function data; of those, 276 (85%) reported sexual activity since delivery. Seventy percent (193) of women sustained minor trauma and 30%(83) sustained major trauma. Sexually active women completed the Intimate Relationship Scale (IRS), a 12-item questionnaire validated as a measure of postpartum sexual function. Both trauma groups were equally likely to be sexually active. Total IRS scores did not differ between trauma groups nor did complaints of dyspareunia. However, for two items, significant differences were demonstrated: women with major trauma reported less desire to be held, touched, and stroked by their partner than women with minor trauma, and women who required perineal suturing reported lower IRS scores than women who did not require suturing [8].
For women who suffer from third- or fourth-degree perineal tear, resumption to normal life may be impaired and delayed. While follow up after 1 year of OASIS has shown around 60-80% of the women to be asymptomatic, we have to think about the remaining 20-40% of women who do not resume normal life.
OASIS will impact the day to day activities and impair their social life, work and of course their sexual life.
Leeman et al. studied the Effect of Perineal Lacerations on Pelvic Floor Function and Anatomy at 6 Months Postpartum, in their study four hundred and forty-eight women had vaginal deliveries. One hundred and fifty-one sustained second-degree or deeper perineal trauma and 297 had an intact perineum or minor trauma. Three hundred and thirty-six (74.8%) presented for 6-month follow-up. Perineal trauma was not associated with urinary or fecal incontinence, decreased sexual activity, perineal pain, or pelvic organ prolapse. Women with trauma had similar rates of sexual activity; however, they had slightly lower sexual function scores (27.3 vs 29.1). Objective measures of pelvic floor strength, rectal tone, urinary incontinence, and perineal anatomy were equivalent. The subgroup of women with deeper (> 2 centimeter) perineal trauma demonstrated increased likelihood of perineal pain (15.5% vs 6.2%) and weaker pelvic floor muscle strength (61.0% vs 44.3%) compared with women with more superficial trauma [11].
Another study by Gommesen et al. showed that impairment of sexual health is common among primiparous women after vaginal delivery. At 12 months postpartum, more than half of the women with a third-degree/fourth-degree tear experienced dyspareunia. Women delivering with no/labia/first-degree tears reported the best outcomes overall. Thus, it is important to minimize the extent of perineal trauma and to counsel about sexuality during and after pregnancy [12].
In a follow-up study by Simone et al, obstetric anal sphincter injuries were associated with AI symptoms up to 4 years after delivery in 40 % of patients and 20 % of the control group. This study showed that women with OASIS have a higher risk of developing AI over the longer term, which is doubled compared with the control group. Furthermore, AI showed a significant impact on QoL after OASIS. Thirty-nine percent of patients had AI and 32 % flatus incontinence. 53% of the women had to alter their lifestyle due to their symptoms and 47% women did not need any alterations in lifestyle due to minimal symptoms. 33% had to wear a pad. According to the results of this study, long-term outcomes following primary repair of OASI are not encouraging. A significant number of women will have incontinence of flatus and liquid stools. OASI will have a negative effect on quality of life in affected women. A significant number of women with OASI decide against further pregnancy and most symptomatic women that have further pregnancy opt to delivery by caesarean section [13].
According to a study by Sultan et al, primary repair is inadequate in most women who sustain third degree tears, most having residual sphincter defects and about half experiencing anal incontinence, which is caused by persistent mechanical sphincter disruption rather than pudendal nerve damage. Attention should be directed towards preventive obstetric practice and surgical techniques of repair [14].
Another study on the long-term symptoms of anal sphincter rupture showed 48% of the women to be affected, mainly with involuntary passage of flatus but also perineal pain, dyspareunia and occasional incontinence of faces [15].
A study on the long-term anal continence and quality of life following postpartum anal sphincter injury women were divided into 3 groups, those who suffered a third-degree tear (Group 1), those who underwent an uncomplicated vaginal delivery (Group 2) or an elective caesarean delivery (Group 3). In the three groups, a total of 28 (53%), 13 (19%) and six (11%) complained of anal incontinence (P < 0.0001) respectively. Comparison of quality of life scores between the groups showed a poorer quality of life in those who suffered a tear (P < 0.0001). In addition, in spite of primary repair, 13 (59%) patients in group 1 showed a persistent sphincter defect compared to one (4%) occult defect in Group 2 and none in Group 3. This study showed that long-term results of primary repair are not encouraging. It therefore emphasizes the importance of primary prevention and preventing further sphincter damage in those who have already suffered an injury (during subsequent deliveries) [16].
Another study evaluating women’s experience after a third degree obstetric anal sphincter tear concluded that a third-degree tear causes a significant emotional and psychological impact on women's physical and emotional well-being. We recommend that all staff receive adequate training to deal with the issues that may be raised. The provision of a dedicated, multidisciplinary team involved at an early stage to coordinate the repair and follow-up is recommended to allow a sensitive, consistent, evidence-based approach, particularly in terms of decision-making for subsequent births. The experiences and needs of partners require further study [17].
Conclusion
Perineal tears during childbirth impact women for years to come. Appropriate intrapartum care and identification and appropriate repair is of extreme importance in this regard. Psychological support and evaluation of the effect of the tears on quality of life is an often neglected but extremely important part of an obstetrician’s practice.
Further research is required to explore the effect on quality of life of women suffering from perineal tears.
References
- Kettle C, Tohill S. Perineal BMJ Clin Evid. 2008.
- https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-perineal-tears-poster-colour.pdf
- https://www.mheducation.ca/williams-obstetrics-25th-edition-study-guide-9781259642906-can
- Villot A, Deffieux X, Demoulin G, et al. Prise en charge des périnées complets (déchirure périnéale stade 3 et 4) : revue de la littérature [Management of third and fourth degree perineal tears: A systematic review]. J Gynecol Obstet Biol Reprod (Paris). 2015; 44: 802-811.
- Aigmueller T, Umek W, Elenskaia K, et al. Guidelines for the management of third and fourth degree perineal tears after vaginal birth from the Austrian Urogynecology Working Group. Int Urogynecol J. 2013; 24: 553-558.
- Fernando RJ, Sultan AH, Freeman RM, et The management of third- and fourth-degree perineal tears. Guideline No. 29. London: Royal College of Obstetricians and Gynaecologists. 2015.
- https://who.int/reproductivehealth/publications/sexual_health/defining_sh/en/
- Rogers RG, Borders N, Leeman LM, et Does spontaneous genital tract trauma impact postpartum sexual function? J Midwifery Womens Health. 2009; 54: 98-103.
- Brubaker L, Handa VL, Bradley CS, et al. Sexual function 6 months after first Obstet Gynecol. 2008; 111: 1040-1044.
- Leeman L, Rogers R, Borders N, et The Effect of Perineal Lacerations on Pelvic Floor Function and Anatomy at 6 Months Postpartum in a Prospective Cohort of Nulliparous Women. Birth. 2016; 43: 293-302.
- Gommesen D, Nøhr E, Qvist N, et Obstetric perineal tears, sexual function and dyspareunia among primiparous women 12 months postpartum: a prospective cohort study. BMJ Open. 2019; 9: e032368.
- Cornelisse S, Arendsen L, van Kuijk, et al. Obstetric anal sphincter injury: a followy on longer term outcome. Int Urogynecol J. 2016; 27: 1591-1596.
- Sultan AH, Kamm MA, Hudson CN, et al. Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ. 1994; 308: 887-891.
- Haadem K, Ohrlander S, Lingman G. Long-term ailments due to anal sphincter rupture caused by delivery--a hidden problem. Eur J Obstet Gynecol Reprod Biol. 1988; 27: 27-
- Samarasekera DN, Bekhit MT, Wright Y, et al. Long-term anal continence and quality of life following postpartum anal sphincter injury. Colorectal Dis. 2008; 10: 793-799.
- Williams A, Lavender T, Richmond DH, et al. Women's experiences after a third-degree obstetric anal sphincter tear: a qualitative study. Birth. 2005; 32: 129-136.