Physical Activity After Delivery: A Feasibility Study
Author'(s): Antonio Gonzalez Fiol, MD1, Geoffrey Ho, MBBS2, Dongchen Li, MD3, Richard Amdur, PhD4, Chapman Wei, MD2, Homa K. Ahmadzia, MD5, Marianne David, MD2, Christopher Jackson, MD2 and Jeffrey S Berger, MD, MBA2
1Department of Anesthesiology, Yale School of Medicine, New Haven,CT, USA.
2Department of Anesthesiology and Critical Care Medicine, George Washington University School of Medicine and Health Sciences,Washington, DC, USA.
3Department of Anesthesiology, Rutgers, New Jersey Medical School,Newark, NJ, USA.
4Department of Surgery, George Washington University School of Medicine and Health Sciences, Washington, DC, USA.
5Department of Obestetrics and Gynecology, George Washington University School of Medicine and Health Sciences, Washington, DC, USA.
*Correspondence:
Antonio Gonzalez Fiol, MD, Department of Anesthesiology,Yale School of Medicine, New Haven CT, USA.
Received: 12 September 2020; Accepted: 08 October 2020
Citation: Antonio GF, Geoffrey Ho, Dongchen Li, et al. Physical Activity After Delivery: A Feasibility Study. Anesth Pain Res. 2020;4(3): 1-6.
Abstract
Background: Early mobility is one of the main goals of the enhanced recovery after cesarean delivery, yet it is rarely objectively measured. Benefits related to this goal include mechanical prevention of deep venous thrombosis and early discharge.
Methods: We conducted a multi-center prospective study in which an activity tracker was utilized to measure the steps taken by patients after delivery. The primary outcome was steps taken after vaginal or cesarean delivery. Secondary outcomes was factors affecting ambulation (e.g pain/satisfaction with pain management and mode of delivery).
Results: Data from 50 postpartum patients were analyzed. Vaginal delivery patients took more cumulative steps at all times when compared to cesarean delivery patients. At 24 and 48 h vaginal and cesarean delivery patients took 5911 ± 2162 versus 3421± 2314 (P = 0.0006) and 9813 ± 3916 versus 6306 ± 5835 (P = 0.03), respectively. In the random effects mixed model, mode of delivery and time main effect were also significant (p<0.0001). In addition, each point increase in body mass index was noted to decrease the number of steps by 35 (95% CI -68 to -3).
Conclusion: Ambulation in the first 48 h after delivery is mainly affected by the mode of delivery and body mass index.
Keywords
Introduction
Enhanced Recovery after Surgery focuses on decreasing modifiable factors associated with prolonged hospital stay. These factors are:pain control, ileus, and immobilization [1]. Despite the recognition that early ambulation may enhance recovery and offers mechanical prophylaxis against deep venous thrombosis (DVT), this variable is rarely objectively measured immediately post-partum [2,3]. The use of activity trackers may help identify patients not meeting early functional recovery targets [3].
The use of activity trackers have been studied before to monitor the physical activity of cardiac patients given that this is a population for which physical activity is a major rehabilitation component [4,5]. In addition, the aforementioned devices have also been used to objectively measure the physical activity of parturients self-identified as inactive [6,7]. Most parturients (50-60%) do not participate in regular physical activity during pregnancy [6,8]. Sedentary behaviors are more noticeable during the third trimester [6]. When sedentary behaviors and the hypercoagulable state of pregnancy are factored in, encouraging and measuring postpartum mobility to prevent DVT seems prudent [6,8,9].
In this pilot study we aimed to objectively quantify ambulation for 48 hoursafter cesarean and vaginal delivery in our patient population. We hypothesize that the vaginal delivery patient population will demonstrate earlier ambulation when compared to their counterparts during this period. In addition, we also assessed demographic variables, patient satisfaction with pain management strategies as well as visual analogue scores for pain and compared findings to ambulation patterns.
Methods
After Institutional Review Board approval from both Rutgers, New Jersey Medical School and George Washington University School of Medicine and Health Sciences, we conducted this pilot, prospective study aimed at measuring the physical activity of American Society of Anesthesiologists (ASA) Classification I and II women aged 18 years and older, after a normal spontaneous vaginal (NSVD) or cesarean delivery (CD) under neuraxial anesthesia. The study was registered at clinicaltrials. gov (NCT02967016). Patients were approached and consented by a member of the study team during the preoperative interview process for the elective CD group, and immediately after delivery (without immediate major complications, i.e hemorrhage, retained placenta) for the NSVD group. After obtaining informed consent, patients were divided into two groups depending on the mode of delivery. We excluded patients who had neonates admitted to intensive care, as we felt that this would artificially inflate their ambulation. All patients were recruited (delivered) during regular working hours of 7am - 5 pm from April 1, 2017 to July 30, 2019. Of note, recruitment was slow given that one of the main recruiters left Rutgers Medical School of NJ.
Patients were provided with an Actigraph GT3X+ activity tracker (ActiGraph LLC, Pensacola, FL) to be worn on the nondependent wrist 3 hours after delivery. Number of steps taken was the primary outcome variable. Patients were then evaluated at 6, 12, 24, 36 and 48 hours after delivery. During these evaluation points, pain (visual analogue scores; ranging from 0 to 100), factors affecting mobility, and level of satisfaction with their analgesia (range 0-100) were assessed. After 48 hours the Actigraph GT3X+ was interrogated and objective data, such as mean daily steps, was obtained.
All patients in the CD group received a spinal with bupivacaine 0.75% (1.6 ml), Fentanyl 15 mcg and intrathecal morphine (ITM) 0.1 mg. In addition, ketorolac 30 mg was administered during fascia closure. Postoperative orders included acetaminophen and a non-steroidal anti-inflammatory agent every 6 h scheduled. The NSVD patients had controlled epidural analgesia delivered via a continuous infusion of bupivacaine 0.125% with 2 mcg/ mLfentanyl solution at 8 mL/h and patient-activated boluses of 5 mL with a lockout interval of 10 minutes. After delivery both groups were offered additional oral opioid for breakthrough pain, as well as antiemetics as requested.
Statistical Methods and Analysis
Distributions of continuous variables were examined for non- normality or outliers using frequency histograms and QQ plots, and transformed if necessary. Outliers defined by a gap in the histogram at least 2 standard deviation (SD) units wide, were capped at a value 0.1 SD units above the next largest value. After recruiting 50 patients a post-hoc power analysis was performed. We examined power to detect a group by time interaction in a random effects mixed model, across 5 time points using 2 treatment groups (CD, NSVD), based on an effect size in which CD had mean steps of 1000, 1600, 3400, 4000, and 6300 at each time point, respectively,and NSVD had 700, 1500, 2500, 3800, and 3500 more steps at each of these time points. We generated 1000 simulated data sets with this effect size with n=25 per group, with each subjects’ steps being selected randomly and independently from a distribution with the above mean and SD. The proportion of simulations with significant group by time interaction represented the power to detect this effect size using this sample size. Using total N of 50, power was 0.82 to detect this effect.
Descriptive statistics were reported by delivery mode and for the full sample, using mean and SD. The association between delivery mode and patient variables was examined using chi- square or Fishers Exact Test for categorical variables, or a 2-tailed independent-groups t-test or Kruskal-Wallis test for continuous variables. In order to account for within-subject auto-correlation of patient variables across time, a random-effects mixed model was used to evaluate whether there was a time effect (change in steps taken over time from delivery, averaged across types of delivery), a group effect (whether NSVD vs. CD patients had different total steps, averaged across time), and the group by time interaction (whether the pattern over time differed by group). This was adjusted for age and BMI, since these might be associated with both type of delivery and with steps taken post-delivery, and thus, could act as confounds. This type of analysis was also used for satisfaction with pain control, level of resting pain, and level of pain when moving. SAS v9.4 (SAS Institute, Cary, NC) was used for data analysis with p <0.05 considered significant.
Results
There were 25 CD patients and 25 VD patients in the study, with mean age 30.0 ± 6.1 years and mean BMI 31.7 ± 6.1 kg/m2. CD and VD patients did not differ significantly by parity, gestation number or BMI. Age was slightly older in CD patients (Table 1). All recruited patients completed the study.
Ambulation
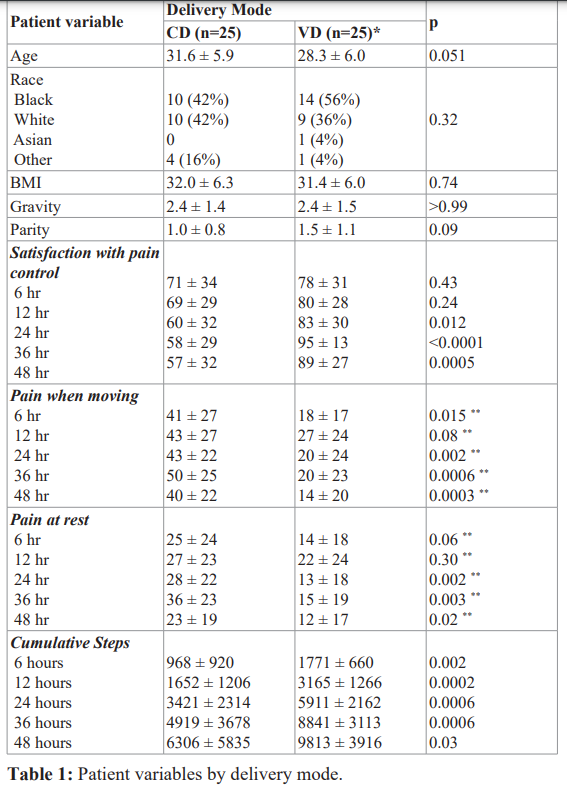
Cumulative steps were significantly higher for VD than CD patients at each time interval (Table 1; Figure 1). The mean cumulative steps (standard deviation, SD) at 24 hours were noted to be 5911 (2162) and 3421 (2314) for the VD and CD patients, respectively. At 48 hours the mean cumulative steps (SD) were 9813 (3916) and 6306 (5835) for the VD and CD patients, respectively.
CD- Cesarean delivery; VD- Vaginal delivery; BMI- Body mass index. * Step Data was only available for n=20 patients** Kruskal-Wallis test was used due to skewed distributions.
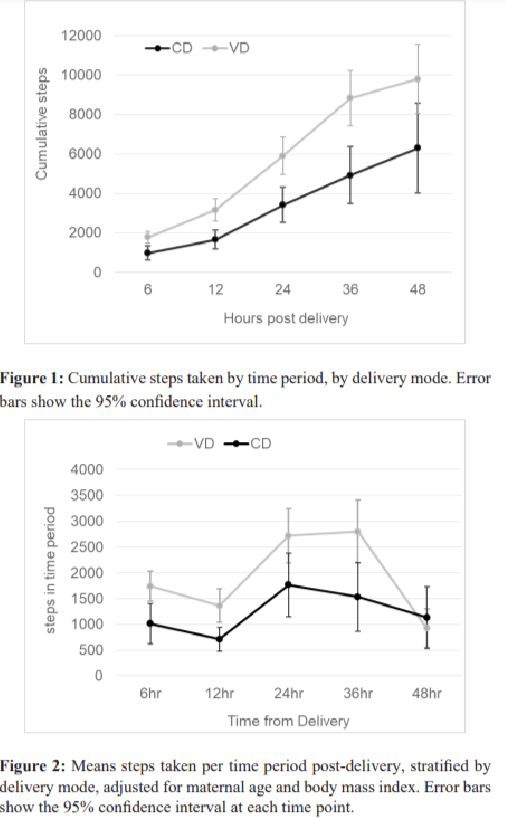
In the random effects mixed model predicting steps taken as a function of time post-delivery and mode of delivery, adjusted for age and BMI, the main effect of mode of delivery was significant. CD patients took 728 fewer steps than VD patients during the first 6 hours (95% CI -1230 to -226; p=0.005). The time main effect was also significant (p<0.0001). Compared to the reference time period (0-6 hours post-delivery) the VD cohort took 378 fewer steps during 6-12 hours, 975 and 1057 more steps were taken at 12-24 and 24-36 hours, respectively. In this same cohort a total of 818 fewer steps were taken at 36-48 hours (all p<0.001 compared to 0-6 hours; Figure 2). Also, the delivery mode by time interaction was significant (p<0.0001), with a larger increase in steps from 24 to 36 hours in VD (2799) than CD (1534) patients (Figure 2). As noted in the adjusted model (Figure 2), CD patients demonstrated a trend toward decrease steps after 24 hours, whereas the decrease in steps for the VD group occurred after 36 h. In the adjusted model, the percentage difference in steps taken at 24 and 36 hours between VD and CD was noted to be 42% and 58%, respectively.
Type of analgesia (p=0.19), race (p=0.34), and age (p=0.34) were not significantly associated with steps taken. There was a significant association with BMI, however, (p=0.04). The parameter estimate for BMI (-0.35 with SE 16.5) indicates that for each additional BMI point, the mean number of steps taken dropped by 35 (95% CI -68 to -3), after adjusting for age, race, delivery mode and time.
Pain Control
Pain at rest was significantly higher for CD than VD patients, starting at 24 hours post-delivery. Pain at rest had a significant time effect, with a significant increase from 6 to 12 hours post-delivery (from 19 [13-25] to 24 [17-30]) and then a decline at 48 hours (to 17 [12-22]). On average, CD patients had higher resting pain than VD patients (27 [20-34] vs 15 [9-21], p=0.014). CD patients also reported significantly more pain while moving at most time points, with mean pain score more than twice as high than VD patients pain (mean 41 [34-49] vs mean 20 [13-27], p<0.0001) (Table 1).
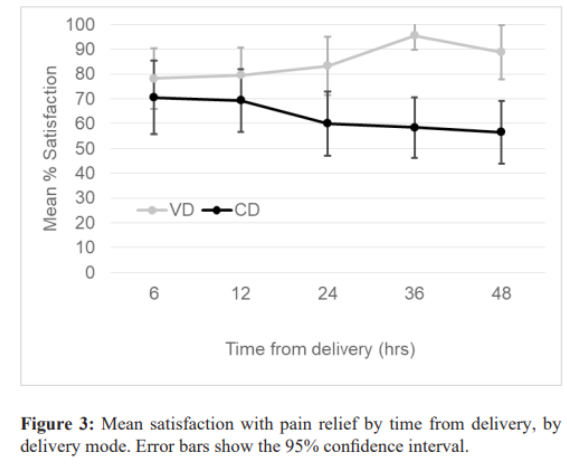
Satisfaction with Pain Relief
Across the study population, satisfaction with pain control was significantly higher for NSVD patients at 24 hours (p=0.012), 36 hours (p<0.0001), and 48 hours (p=0.0005), but did not differ significantly at 6 hours (p=0.43), or 12 hours (p=0.24) (Table 1; Figure 3). CD patients had mean satisfaction with pain control of 57 (95% CI 45-69) across time, while NSVD patients had mean satisfaction of 83 (73-93), after adjusting for age and BMI (p=0.0006).
Discussion
Our study suggests that VD patients take more steps across all time points, compared to patients who deliver via CD. Before 24 hours, the pattern of mobility is largely similar, with most steps taken at 24 and 36 hours in both groups. The most notable deviation occurs during the 24-36 hour period. The VD patients continued to increase their step count, until the 36-48 hour period where there is a steep fall in the number of steps taken. This timeline likely reflects the breastfeeding courses and other sedentary activities associated with their discharge paperwork. Similarly CD patients increased their number of steps until the 24-36 h epoch. Up to 24 h, our results are in agreement with those reported by Ma et al.3 The latter study noted a 44 % difference in steps between the VD and CD groups, whereas our study revealed a 42% difference. Our study provides additional imformation beyond the 24 h epoch.
The difference in steps between the two groups mentioned above increases to 58% at 36 h, favoring again the VD group. This decrease in the number of steps in the CD group coincides with a decrease in maternal satisfaction and increased pain scores in the hours leading to the 24-36 h epoch. This timeframe is in accordance with the decaying analgesic effects of intrathecal morphine (11- 29 h) [10,11]. Our study points toward a negative trend between pain and steps taken. This is in accordance with the findings from Sharpe et al. [12] that demonstrated that pain is associated with fewer steps taken during the day. In addition, they demonstrated that each additional CD is associated with a decreased number of steps taken.
When evaluating physical activity (steps) afer delivery, it is important to acknowledge the results from the study by Huberty et al. [6]. His team of researchers followed a cohort of parturients self described as inactive from 8-16 weeks gestational age until the third trimester. Their study showed a trend towards an increase in physical activity during the second trimester and the least amount of activity during the third trimester. Hence, parturients self identified as inactive may be undergoing recovery immediately after their most inactive period [6]. These results highlight the importance of promoting the safety and benefits of physical activity during pregnancy, particularly for those patients with sedentary behaviors [6,7].
Our study contributes to the mounting evidence associated with the feasibility of the use of activity trackers [3,12,13]. The use of Actigraph has been validated before by comparing the device to pedometers and other activity trackers [8,14]. The feasibility in our study is substantiated in the fact that none of the patients enrolled withdrew from the study or removed their accelerometers during the 36-48 h of study. Although the total numbers of steps before adjusting for age, mode of delivery and BMI were not similar to those reported by Ma et al. [3] the trends and the difference of steps between the groups were very similar. This can be at least partially explained by the use of different activity tracker devices.
Further statistical analysis suggests that BMI was significantly associated with reduced mobility post-delivery, regardless of mode of delivery. This finding is in accordance with those described by Ma et al. [3]. Analysis of risk factors associated with parturients characteristics that may hinder their ability to recover after delivery is of utmost importance in this era of enhanced recovery after cesarean delivery [3,12,15-18]. This is especially significant as increased BMI is independently associated with risk of venous thromboembolism, a complication carrying high morbidity and mortality, [9] and preventable by taking mechanical (i.e physical activity) and or pharmacologic measures [2].
Some of the limitations of our study include the possible translation of upper extremity movements to steps. This is a limitation to the use of most activity trackers [3]. Despite the limitations known to activity trackers, since all patients wore the same the device in our study, any potential effect of over or under estimation should be similar for all patients. Another limitation in our study is that not all the postpartum rooms have the same layout, hence even for the most essential movements, such as going to the bathroom, patients could have incurred in a different number of steps. Our study may not have been powered to detect the impact of secondary variables,such as age, affecting postpartum ambulation, as identified by Ma et al. [3].
As commercial pedometers and activity trackers become more accurate and widely accessible, there is an increasing awareness that this technology can be used to encourage better health outcomes [19-21]. Despite this mounting evidence of benefits, there is a lack of guidelines regarding the amount of steps needed in the peripartum and puerperium period. Some studies have recommended 8500-12000 steps during the peripartum period [7]. These numbers are based on the Physical activity Guidelines from the Secretary of Health and Human services.* Despite some recommendations for resumption of activities postpartum, there is a lack of guidance surrounding the resumption of physical activity in the early postpartum period, and most guidelines leave both the timing and nature of this activity ill-defined, making it difficult to define standardized goals [22,23]. There is also some evidence that even low-intensity exercise in the early postpartum period can reduce chronic disease risks [24,25].
In conclusion, the use of activity trackers is a feasible measure to monitor postpartum patients and create recovery physical activity curves. Our data points towards the need to improve analgesia past the 24 h mark to parturients undergoing CD. Future study should include determining optimal activity levels for patients based on demographics, including delivery type and BMI, and evaluating educational interventions aimed at achieving ambulation goals.
References
1.Timothy E Miller, Julie K Thacker, William D White, et al. Reduced Length of Hospital Stay in Colorectal Surgery after Implementation of an Enhanced Recovery Protocol.Anesthesia Analgesia. 2014; 118: 1052 1061.
2.D’Alton, Mary E, Elliott K, et al. National Partnership for Maternal Safety. AnesthesiaAnalgesia. 2014; 123: 942-949.
3.Julia Ma, Rachel Martin, Bokman Chan, et al. Using Activity Trackers to Quantify Postpartum Ambulation. Anesthesiology. 2018; 128: 598-608.
4.Alharbi M, Bauman A, Neubeck L, et al. Validation of Fitbit-Flex as a measure of free-living physical activity in a community-based phase III cardiac rehabilitation population. Eur J Prev Cardiol. 2015; 23: 1476-1485.
5.Keith M Diaz, David J Krupka, Melinda J Chang, et al. An accurate and reliable device for wireless physical activity tracking. Int J Cardiol. 2015; 185: 138-140.
6.Huberty JL, Buman MP, Leiferman JA, et al. Trajectories of objectively-measured physical activity and sedentary time over the course of pregnancy in women self-identified as inactive. Prev Medicine Reports. 2016; 3: 353-360.
7.Choi J, Lee J hyeon, Vittinghoff E, et al. Health Physical Activity Intervention: A Randomized Pilot Study in Physically Inactive Pregnant Women. Matern Child Healt J. 2016; 20: 1091-1101.
8.Harrison CL, Thompson RG, Teede HJ, et al. Measuring physical activity during pregnancy. Int J Behav Nutr Phy. 2011; 8: 19.
9.Gonzalez-Fiol A, Eisenberger A. Anesthesia implications of coagulation and anticoagulation during pregnancy. Semin Perinatol. 2014; 38: 370-377.
10.JS Berger, A Gonzalez, A Hopkins, et al. Dose–response of intrathecal morphine when administered with intravenous ketorolac for post-cesarean analgesia: a two-center, prospective, randomized, blinded trial. Int J Obstet Anesth. 2016; 28: 3-11.
11.Sultan P, Halpern SH, Pushpanathan E, et al. The Effect of Intrathecal Morphine Dose on Outcomes After Elective Cesarean Delivery. Anesthesia Analgesia. 2016; 123: 154-164.
12.Sharpe Emily E, Booth Jessica L, Houle Timothy T, et al. Recovery of physical activity after cesarean delivery and its relationship with pain. Pain. 2019; 160: 2350-2357.
13.Faraj Massouh, Rachel Martin, Bokman Chan, et al. Is Activity Tracker–Measured Ambulation an Accurate and Reliable Determinant of Postoperative Quality of Recovery? A Prospective Cohort Validation Study. Anesthesia Analgesia. 2019; 129: 1144-1152.
14.Cadmus-Bertram LA, Marcus BH, Patterson RE, et al. Randomized Trial of a Fitbit-Based Physical Activity Intervention for Women. Am J Prev Med. 2015; 49: 414-418.
15.Unyime Ituk, Ashraf S Habib. [Enhanced recovery after caesarean delivery. Not just a postoperative rehabilitation]. F1000Res. 2018; 7: 513.
16.V Jacques, F Vial, M Lerintiu, et al. [Enhanced recovery following uncomplicated elective caesarean section in France: a survey of national practice]. Ann Françaises D’anesthésie Et De Réanimation. 2013; 32: 142-148.
17.Maike Liebermann, Michael Awad, Megan Dejong, et al. Ambulation of Hospitalized Gynecologic Surgical Patients. Obstetrics Gynecol. 2013; 121: 533-537.
18.Aluri S, Wrench IJ. Enhanced recovery from obstetric surgery: a UK survey of practice. Int J Obstet Anesth. 2014; 23: 157- 160.
19.Dena M Bravata, Crystal Smith-Spangler, Vandana Sundaram, et al. Using Pedometers to Increase Physical Activity and Improve Health: A Systematic Review. Jama. 2007; 298: 2296.
20.Alexander Hodkinson, Evangelos Kontopantelis, Charles Adeniji, et al. Accelerometer- and Pedometer-Based Physical Activity Interventions Among Adults With Cardiometabolic Conditions. Jama Netw Open. 2019; 2: 191-289.
21.I-Min Lee, Eric J Shiroma, Masamitsu Kamada, et al. Association of Step Volume and Intensity With All-Cause Mortality in Older Women. Jama Intern Med. 2019; 179: 1105-1112.
22.Evenson KR, Mottola MF, Owe KM, et al. Summary of International Guidelines for Physical Activity After Pregnancy. Obstet Gynecol Surv. 2014; 69: 407-414.
23.Minig L, Trimble EL, Sarsotti C, et al. Building the Evidence Base for Postoperative and Postpartum Advice. Obstetrics Gynecol. 2009; 114: 892-900.
24.Davenport MH, Giroux I, Sopper MM, et al. Postpartum Exercise Regardless of Intensity Improves Chronic Disease Risk Factors. Medicine Sci Sports Exerc. 2011; 43: 951-958.
25.Michelle F Mottola, Isabelle Giroux, Robert Gratton, et al. Nutrition and Exercise Prevent Excess Weight Gain in Overweight Pregnant Women. Medicine Sci Sports Exerc. 2010; 42: 265-272.