Post-Cardiac Injury Syndrome In A Polytraumatized Patient With Aortic Intervention, Case Report And Literature Review
Author'(s): Juan Samuel Hernández-Meza1*, Juan Diego Monsalve-Sanchez1, Julian Alfonso Sierra-Peña1 and Gustavo Alexis Lemus-Barrios2
1Student, Faculty of Medicine, Pontifical Xavierian University, Bogotá D.C, Colombia.
2Department of Cardiology, Hospital Universitario San Ignacio, Pontifical Xavierian University, Bogotá D.C, Colombia.
*Correspondence:
Juan Samuel Hernandez-Meza, Student, faculty of Medicine,Pontifical Xavierian University, Hospital Universitario San Ignacio. Phone: (+571) 5946161 Ext 2901
Received: 25 Nov 2022; Accepted: 05 Jan 2023; Published: 10 Jan 2023
Citation: Hernández-Meza JS, Monsalve-Sanchez JD, Sierra-Peña JA, et al. Post-Cardiac Injury Syndrome In A Polytraumatized Patient With Aortic Intervention, Case Report And Literature Review. Cardiol Vasc Res. 2023; 7(1): 1-5.
Abstract
Post-cardiac injury syndrome is a type of inflammatory pericardial syndrome that occurs when there is some degree of direct or indirect injury to the pericardium or myocardium, and can occur in patients with acute myocardial infarction, trauma associated with cardiothoracic surgery and accidental or iatrogenic trauma associated with percutaneous coronary intervention. Its definition includes the terms postinfarction pericarditis, post traumatic pericarditis, and postpericardiotomy syndrome. Its pathogenesis is explained by an autoimmune response and a pleuropericardial inflammatory state triggered by tissue injury in the absence of infections or other etiologies. We present the case of a 31-year-old male patient who developed post-traumatic pericarditis secondary to chest trauma who had an adequate response to management with acetylsalicylic acid and did not develop complications.
Keywords
Case Report
A 31 year old male patient presents polytrauma secondary to paraglider fall, having an open tibia and fibula fracture and chest trauma. The patient required bilateral closed thoracostomy due to hydropneumothorax, and also debriding, cleansing and external tutor tibia fixation. Secondary vascular injuries include grade III aortic trauma and distal third aortic arch pseudoaneurysm. The patient required aortic arch repair, aorta carotid bridge, left aorta subclavian bridge closed thoracotomy and thoracic aorta endovascular percutaneous repair.
On his 4th day aortic repair post op he registered fever temperatures without identifiable infectious origin. Blood tests report leukocytosis and neutrophilia. Further blood culture reports are negative. 2 days after the fever starts the patient narrates thoracic retrosternal puncturing progressive pain 8/10 on the analogous pain scale which exacerbates on mahometan position and with valsalva. An EKG was ordered (Figure 1), which reported sinus tachycardia with 125 bpm, normal axis, concave diffuse ST elevation and Spodick sign in DII. Further transthoracic echocardiogram (Figure 2) demonstrated moderate pericardial effusion predominantly over the anterolateral recess with a maximum interphase of 14mm without cardiac tamponade evidence. Suspecting pericardial syndrome with probable infectious etiology a pericardiocentesis was performed with pericardial fluid culture which demonstrated neutrophilic exudate and hemopericardium without positive gram stain and cultures. Thanks to the latter findings the patient was diagnosed with pericarditis with possible traumatic origin and acetylsalicylic acid 1000mg/day was formulated with posterior adequate recovery and without cardiac function compromise.
Discussion
Post cardiac injury lesion syndrome compiles pericarditis leading to inflammation and injury of the pericardial tissue. This includes post myocardial infarction pericarditis, post pericardiotomy syndrome and post traumatic pericarditis. This syndrome is associated with
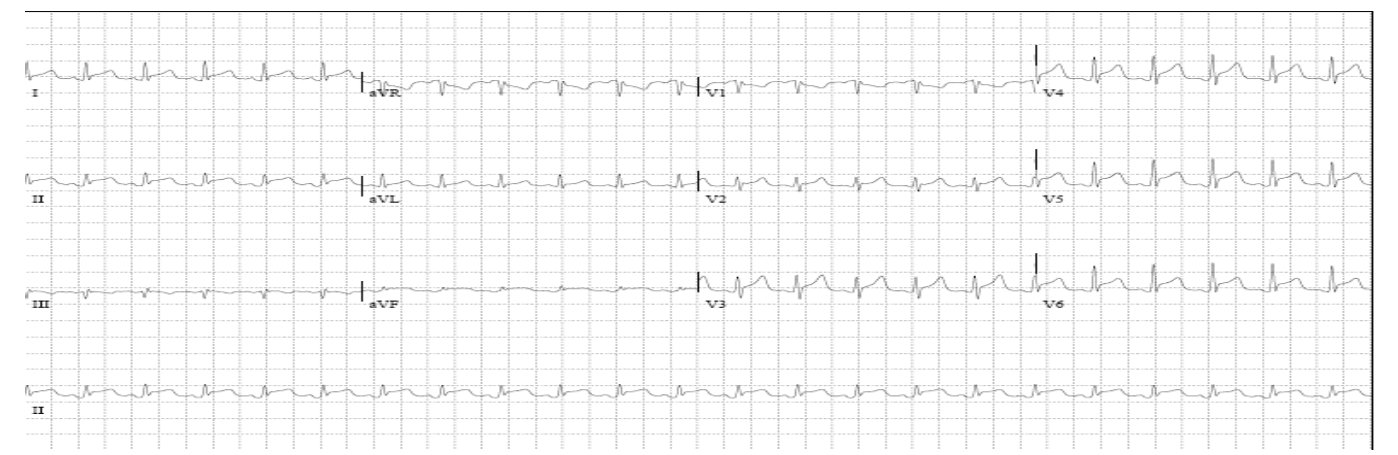
Figure 1: Electrocardiogram showing a sinus tachycardia rhythm and a diffuse concave elevation of the ST segment in both frontal and precordial leads associated with PR segment depression and the presence of Spodick sign visible predominantly in DII.
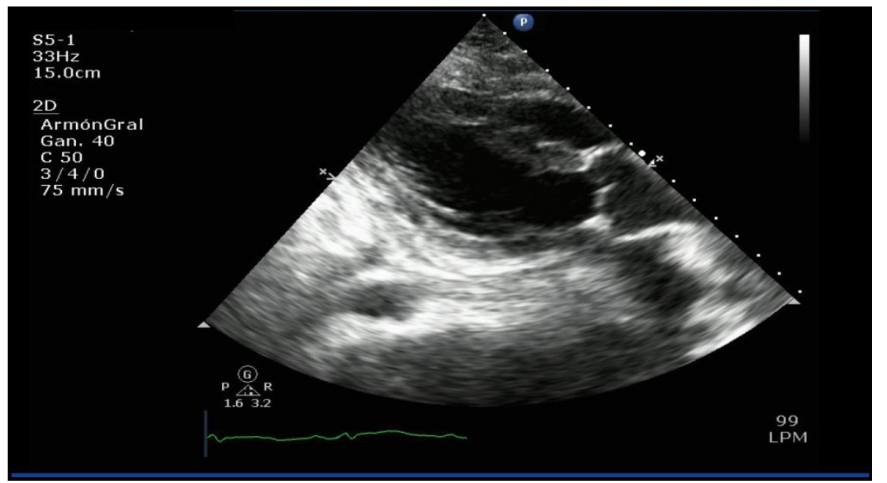
Figure 2: Transthoracic echocardiogram with evidence of predominantly moderate pericardial effusion over the anterolateral recess with a maximum interface of 14 mm.
prolonged hospital admission days, longer rehab days and major probability for readmission [1]. We present the case of a patient with post cardiac lesion who developed acute pericarditis due to severe polytrauma and aortic surgical intervention.
Post cardiac lesion syndrome incidence is variable and depends on the contect. For example, post infarction incidence is less than 5% and descending due to improvement of pharmacological reperfusion strategies and percutaneous primary coronary intervention [2,3]. On the other hand, patients led to cardiac intervention have an estimated post pericardiotomy pericarditis around 10-40% [2], and most number of cases present after aortic valve replacement (HR, 1.97; 95% CI95, 1.58–2.46; P<0.001), mitral valve replacement (HR, 1.97; 95% CI95,, 1.58–2.46; P<0.001) and aortic surgery (HR, 3.06; 95% CI95,, 2.24–4.16; P<0.001) comparing with bypass coronary surgery [3].
Although the etiopathology is unclear, it is hypothesized to occur due to pericardial tissue immune response from myocardial necrosis (post infarction pericarditis), surgical trauma (post pericardiotomy pericarditis), accidental or iatrogenic thoracic trauma (post traumatic pericarditis) [1] (Figure 3). Mesothelial cellular damage is related to irritant substance exposure to the pericardial sac such as blood, which triggers an immune and humoral response, elevating cytokines and cardiac tissue specific antibodies. Cardiovascular surgical patients in studies demonstrate elevated anti myocardial antibodies correlate with post cardiac lesion syndrome, its severity and prognosis, specifically with anti myosin and anti actin antibodies. Nevertheless, multiple anti cardiac antibodies have been able to be detected in blood after myocardial or pericardial injury [3].
We theorize immune complex formation mediated by specific myocardial and mesothelial T CD4+ lymphocytes acting as markers for autoantigens, and generating an auto inflammatory response. Pericardial and mesothelial tissue shows greater sensitivity to this inflammation than muscular and interstitial myocardial tissue. This manifests clinically as pleuro-pericarditis.
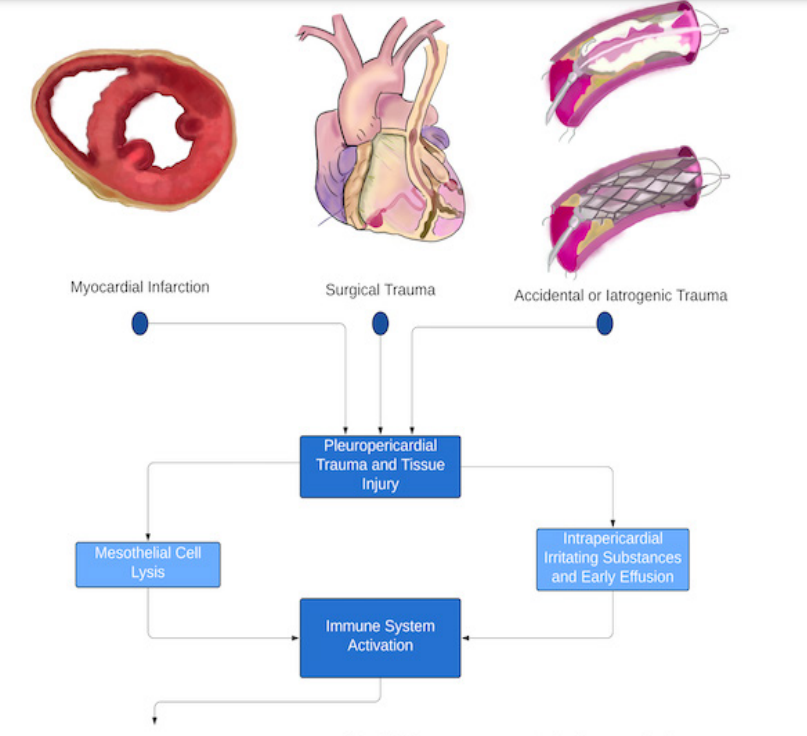
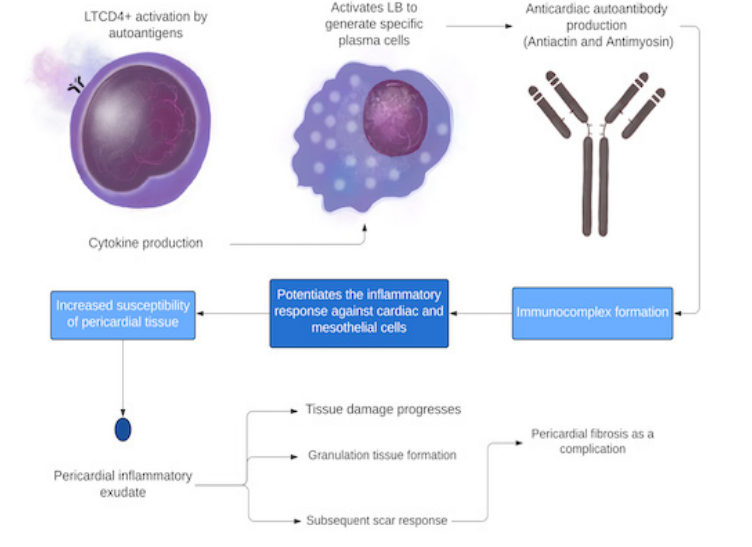
Figure 3: Etiopathogenesis of post-cardiac injury syndrome. Adapted from [2]. The presence of pleuropericardial tissue trauma and the entry of irritating substances into the pericardial sac lead to the activation of CD4+ T lymphocytes, which will give rise to the stimulus leading to the production of antibodies directed against tissues of the myocardium and pericardium, leading to thus generating an inflammatory pericardial exudate that accentuates the initial noxa and gives rise to the clinical picture.
Cellular and humoral activation leads to inflammatory pericardial exudate which furthers tissue injury, granulation tissue and posterior fibrosis that replaces affected mesothelial cells. Antigens released into the bloodstream, joined with the innate immunity activation can explain this adaptive response [5].
Two further reasons supplement this autoimmune theory: The latency between the initial injury and clinical manifestation which correlates with the time the adaptive immune response activates and the effective response after giving anti-inflammatory treatment to these patients which will be further developed.
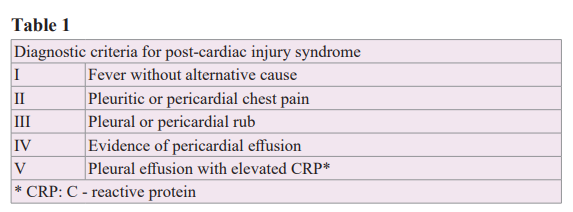
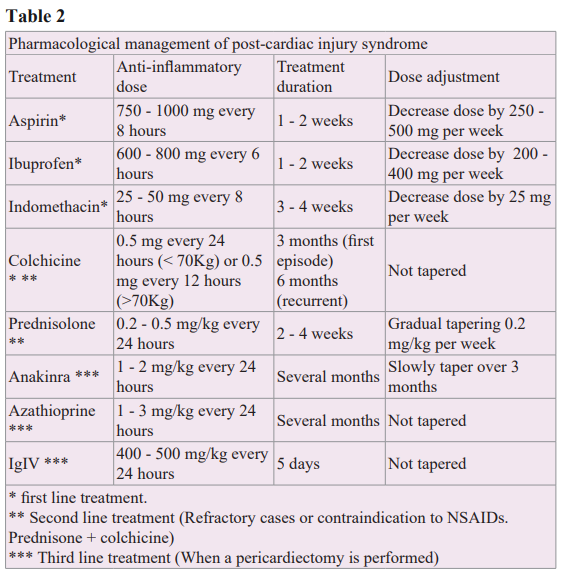
The European Society of Cardiology [5] established at least two of the following criteria to confirm post cardiac lesion syndrome: Fever with no other apparent cause (i), Thoracic pain with pericardial or pleuritic characteristics (ii), pericardial or pleural friction rub (iii), imagenological evidence of pericardial effusion (iv) and imagenological evidence of pleural effusion with acute phase molecules such as RPC elevated (v) [6]. Therefore it is crucial to examine thoroughly with a complete clinical history, physical exam and complementary paraclinical tests to confirm this diagnosis (Table 1).
Further diagnostic tools include EKG, Chest X Ray, and chest echography. Every patient with a suspected post cardiac lesion syndrome must have at least one echocardiogram [6]. This evaluates the presence of pericardial effusion, quantifies the size of the effusion and detects echographic signs of cardiac tamponade as an associated complication. In most of the cases a transthoracic echocardiogram might suffice but in other patients with limited window such as post op patients, transesophageal echocardiogram can be useful [7].
The most suggestive EKG finding consists of diffuse ST elevation with PR segment depression as with other etiological non post cardiac lesion syndrome pericarditis. Another important finding is called the Spodick sign which references a descending slope on the TP segment, visualized more clearly in DII and lateral precordial derivations [8]. Chest X ray discards differential diagnosis and can show pleural effusion with or without pulmonary infiltration, augmented cardiac silhouette in the contexts of another cardiac disease and also shows the presence of pericardial effusions with a volume greater than 200mL [9]. Current European Cardiological Society guidelines are from 2015 [6], which establish that the correct patient treatment with post cardiac lesion pericarditis after doing an adequate diagnosis are similar to those patients with other etiological pericarditis. As mentioned before, the etiological cause is mainly an immune inflammatory response which needs to be controlled with empirical anti inflammatory therapy, which reduces symptoms and improves the patient overall.
Acetylsalicylic acid (Aspirin) is the first line pharmacological treatment for post infarction pericarditis, especially in those patients receiving prior anti platelet aggregation therapy. As the second alternative, NSAID as ibuprofen can be selected, having considered the contraindications and patient comorbidities. Regarding the use of colchicine, the European Cardiology Society as part of the pharmacological therapeutic plan recommends 1. adding colchicine with NSAID like with other pericarditis, 2. consider implementing colchicine for a month in the context of cardiovascular surgeries to prevent post pericardiotomy syndrome [9]. On the contrary colchicine is not recommended to treat post op effusions without systemic inflammation symptoms and also NSAID is not recommended with asymptomatic post op effusions. Alternatives such as ketorolac are recommended with patients with severe symptoms and patients who can not tolerate oral feeding [10]. Different dosage and treatment managements are described in table 2.
Prognosis for this syndrome is good, with complication probability less than 4% for recurrence development, less than 2% associated with cardiac tamponade and approximately 3% for constrictive pericarditis [7]. Although literature reports low probability for complications, every post cardiac lesion syndrome patient must be followed up and examined every six to twelve months with ecography or before if symptoms are present to discard constrictive pericarditis.
Conclusion
Medical advances have augmented life expectancy and also the number of surgical procedures. Knowledge about post cardiac lesion syndrome within the acute pericarditis spectrum is therefore relevant. This includes various entities of pericardial inflammation due to myocardial infarction, direct or indirect trauma, and surgical invasive procedures. Therefore there must be a high suspicious mentality for this diagnosis and correlate clinical findings to further confirm the diagnosis. Having knowledge of every lab exam and image to assess these cases helps confirm the diagnosis, severity and finally the adequate management and treatment for the patient based on the best evidence to avoid recurrences and avoid complications such as cardiac tamponade and constrictive pericarditis.
References
- Imazio M, Brucato A, Rovere ME, et al. Contemporary features, risk factors, and prognosis of the postpericardiotomy syndrome. Am J Cardiol. 2011; 108: 1183.
- Imazio M, Hoit BD. Post-cardiac injury syndromes. An emerging cause of pericardial diseases. Int J Cardiol. 2013; 168: 648-652.
- Malik J, Zaidi S, Rana A, et al. Post-cardiac injury syndrome: An evidence-based approach to diagnosis and treatment. American Heart Journal Plus: Cardiology Research and Practice. 2021; 12: 100068.
- Lehto J, Kiviniemi T, Gunn J, et al. Occurrence of Postpericardiotomy Syndrome: Association With Operation Type and Postoperative Mortality After Open-Heart Operations. J Am Heart Assoc. 2018; 7: e010269.
- Sasse T, Eriksson U. Post-cardiac injury syndrome: Aetiology, diagnosis, and treatment. ESC EJ. Cardiol Pract. 2017; 15: 21- 31.
- Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015; 36: 2921.
- Izadi Amoli A, Bozorgi A, HajHossein Talasaz A, et al. Efficacy of colchicine versus placebo for the treatment of pericardial effusion after open-heart surgery: A randomized, placebo-controlled trial. Am Heart J. 2015; 170: 1195.
- Chaubey VK, Chhabra L. Spodick's sign: a helpful electrocardiographic clue to the diagnosis of acute pericarditis. Perm J. 2014; 18: e122.
- Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010; 121: 916.
- Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of Acute and Recurrent Pericarditis: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020; 75: 76-92.