Postoperative Death of a Young Adult with Acute Endocarditis Complicated by SARS-CoV-2 Infection Following a Routine Double Valve replacement and Extracorporeal Oxygenation membrane: A Case Report
Author'(s): Soumer Khedija1, Bousnina Mouna1, Azabou Nadia1, Ben Saida Fatma1*, Bennour Emna2 and Jemel Amine1
1Department of Cardiovascular Surgery, Abderrahmen Mami Hospital, Ariana, Tunisia.
2Departement of Cardiology, Abderrahmen Mami Hospital,Ariana, Tunisia.
*Correspondence:
Ben Saida Fatma, Department of Cardiovascular Surgery, Abderrahmen Mami Hospital, Ariana, Tunisia.
Received: 22 Dec 2022; Accepted: 25 Jan 2023; Published: 30 Jan 2023
Citation: Khedija S, Mouna B, Nadia A, et al. Postoperative Death of a Young Adult with Acute Endocarditis Complicated by SARSCoV-2 Infection Following a Routine Double Valve replacement and Extracorporeal Oxygenation membrane: A Case Report. Cardiol Vasc Res. 2023; 7(1): 1-4.
Abstract
At the time of the COVID-19 pandemic, practicing physicians are confronted with the challenge of distinction SARS-CoV-2 infection from other diagnostic entities but also the possibility of treating COVID-19 patients with other co-existing diseases. This challenge becomes even greater with infectious diseases like infective endocarditis given the similarity of clinical manifestation of the two diseases.
We report the case of a young adult who was diagnosed with acute infective endocarditis complicated by heart failure and who simultaneously contracted the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. He had double valve replacement but unfortunately, his clinical condition deteriorated rapidly with respiratory COVID-19 complications followed by multiorgan failure.
Physicians should maintain a high degree of clinical suspicion to diagnose COVID-19 concomitant with infective endocarditis. The task of distinguishing the two is based on RT-PCR testing but mainly on transesophageal echocardiography (TEE).
Keywords
Introduction
Although infection with SARS-CoV-2 virus is considered the main health problem currently, COVID-19 has not eliminated other diseases and multiple illnesses can complicate and coexist with it. Healthcare providers are faced with the challenge of differentiating COVID-19 infection from other diagnostic entities. This difficulty may increase in the presence of another cause of fever, hypoxic respiratory failure, and elevated inflammatory biomarkers. This applies to patients with infective endocarditis. IE is a serious life- threatening disease with high morbidity and mortality [1]. Early diagnosis and treatment is key to avoid major complications as heart failure, local extension of the infection with destruction of the valvular and peri-valvular tissue and embolic events [2].
This report describes a case of mitro-aortic valve IE complicated by heart failure in a patient who was later diagnosed with COVID-19.
Case Presentation
During the height of the COVID-19 pandemic, a 36-year-old man with a history of smoking and drug addiction presented to the hospital with fever and orthopnea 2 days before admission. He has no history of rheumatic fever. On initial presentation, the patient’s vital signs were as follows: heart rate 124 beats per minute, blood pressure 94/56 mmHg, oxygen saturation 94% on room air, respiratory rate 22 breaths per minute and temperature of 38,5°C. His physical exam was unremarkable except for an aortic diastolic murmur and bilateral lung crackles. Chest X-ray findings were compatible with pulmonary edema. The RT-PCR nasal swab for SARS-CoV-2 on admission was negative. Laboratory evaluation demonstrated hemoglobin of 11,3 g/dl, white blood cells of 8300/mm3, platelet count of 252000/mm3, and markedly elevated inflammatory markers C-reactive protein of 134 mg/l.
Blood cultures were positive for Enterococcus faecalis from consecutive specimens.
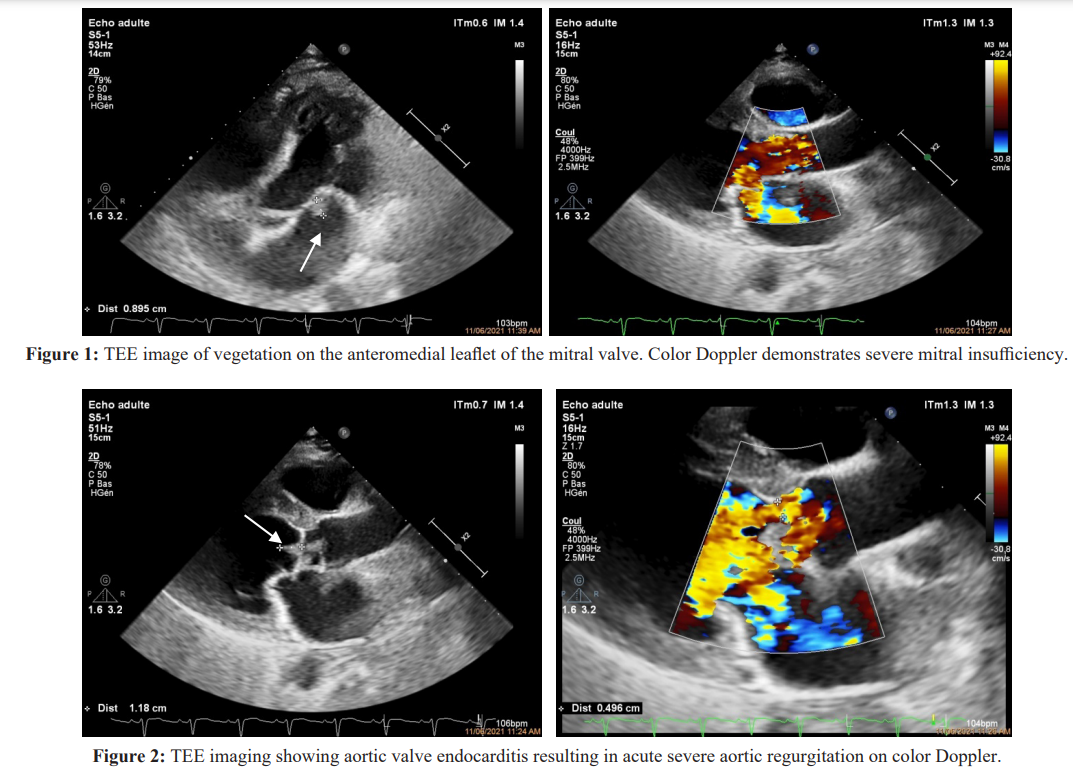
The patient was admitted to cardiology department to investigate for the etiology. Shortly after arrival, he underwent a transthoracic echocardiogram and transesophageal echocardiography for further evaluation. These showed good biventricular systolic function with an ejection fraction of 60% and revealed a 10 x 11 mm mobile vegetation attached to the anteromedial leaflet of the mitral valve associated with vegetations on all three aortic cusps with no paravalvular abscesses (Figures 1 and 2). Colour Doppler examination revealed a severe mitro-aortic regurgitation by valve destruction without signs of significant left ventricular volume overload or dilatation. The patient was initiated on an IV antibiotic according to the antibiogram; however, persistent bacteremia was noted despite several days of antibiotic therapy.
Given the severity of his mitro-aortic insufficiency and worsening symptoms of congestive heart failure, persistent bacteremia, and vegetation size > 10 mm, the patient was transferred to our department and a double valve replacement with prosthetic valve was urgently performed. He was found to have a complete destruction of the aortic valve, with vegetations present in the right and non-coronary cusps. There was also a perforation of the anterior leaflet of the mitral valve. The native mitral and aortic valve were resected and replaced with a 31 mm and 23 mm mechanical prosthesis, respectively, with partial preservation of the native mitral valve apparatus and the surgery was completed uneventfully.
The patient was placed in ICU where he was extubated a few hours following the surgery but rapidly the patient’s condition worsened with a persistent fever and an increase in oxygen requirements accompanied with a rapid progression of opacities in the thorax X-ray. He needed reintubation twenty hours after disconnection because of severe hypoxia. The culture of mitral and aortic valves grew the same organism Enterococcus faecalis and the patient continued to receive appropriate antibiotic therapy. Echocardiography showed that his heart function was satisfactory with normal functioning aortic and mitral prostheses. On the 3rd postoperative day, a second RT-PCR test was performed confirmed the diagnosis of an acute respiratory distress syndrome secondary to SARS-CoV-2 infection and then the patient was promptly isolated. Although the maximum ventilatory support including an FiO2 of 100% and a positive end-expiratory pressure of 20 mm H2O, the patient’s respiratory status continued to worsen. Unfortunately, the patient remained profoundly hypoxemic with impaired renal function requiring continuous hemodiafiltration. Arterial blood gas analysis was routinely examined showing a partial pressure of arterial oxygen-to-fraction of inspired oxygen ratio (PaO2/ FiO2) < 85 mmHg and uncompensated metabolic acidosis with pH < 7,15. Therefore, the patient was referred for veno-venous (VV) extracorporeal membrane oxygenation (ECMO) therapy for severe acute respiratory distress syndrome (ARDS) but he died 4 days after surgery as the result of COVID-19 pneumonia followed by multiorgan failure.
Discussion
During the time of COVID-19 pandemic, there is a great concern about the impact of the SARS-CoV-2 infection on the diagnosis and treatment of cardiovascular disease. This is manifest in patients with other infectious diseases like IE. Because of the similarity in clinical presentation between COVID-19 and IE, clinicians are confronted with the challenge of differentiating from each other. They have also to remain vigilant to the possibility of concomitant COVID-19 with IE. Most commonly, both diseases present with fever, dyspnea and cough or even relatively rapid decompensation as well as nonspecific laboratory values and chest X-ray findings [3,4]. In such situations, appropriate diagnosis tests (including blood cultures) but mostly TEE should be performed when patients show signs suggestive of endocarditis.
While RT-PCR has emerged as the test of choice for detection of infected individuals, establishing a diagnosis of COVID-19 using RT-PCR is not without its limitations and a negative RT-PCR test does not exclude the possibility of COVID-19 infection [5]. Due to the relatively long processing time of the RT-PCR ranging from 2 to 3 hours to days, patients who are undergoing major emergent operations are screened with rapid test or explored by computed tomography of the chest.
Although we could not determine at what time our patient, get infected with SARS-CoV-2 virus, we suspect it was preoperatively, given the time course of his clinical deterioration. It would have been very difficult to make a decision if we were aware of his COVID status before surgery. There are a few reports about the effects of COVID-19 pneumonia on bypass followed by mechanical ventilation during recovery and performing cardiac surgery in a COVID-19 positive patient would be risky. The risk of sepsis and thromboembolic events is increased when COVID-19 and IE are associated. Moreover, inflammatory cascade induced by cardiopulmonary bypass may worsen patient’s condition. But, on the other hand, and given that surgical intervention can be lifesaving in unstable patients with active valve endocarditis complicated by heart failure and because of the young age of the patient with no comorbidities, it remains ambiguous to propose such cases like the present report be postponed. In our patient, It is not yet known whether surgery has brought benefits to the patient or otherwise has worsen his clinical condition given that the patient deteriorated ultimately from respiratory COVID-19 complications rather than heart failure.
In SARS-CoV-2 infection, refractory hypoxemia is common in cases of ARDS despite invasive mechanical ventilation and is further complicated by multiple organ dysfunction syndrome, and even death. This difficult situation has required rescues therapies such as, prone positioning, and ECMO [6,7].
ECMO has been proposed in severely hypoxemic patients with Middle East respiratory syndrome (MERS) caused by a coronavirus who failed conventional strategies and needing respiratory or circulatory assistance if necessary [8]. At present, VV-ECMO mode is mostly used, but it is unknown in COVID-19 how many have or will develop myocarditis or circulatory failure. However, even with the use of ECMO, the mortality rates of severe and critical patients with COVID-19 are still very high and represent approximately 82,3% [7,9]. This was the case in our patient.
Early implementation of ECMO before multiorgan failure or severe ventilator-associated lung injury is recommended. In fact, recent studies have suggested that early initiation of ECMO in ARDS due to COVID-19 might be beneficial, especially among younger patients; otherwise, if ECMO is established more than 10 days after invasive ventilator use, the possibility of successful treatment is low [10,11]. The role of ECMO in rescuing critically ill patients with COVID-19 infection is still yet to be determined and several fundamental questions remain unanswered, including benefit, timing, indications and risks of ECMO. More studies are necessary to better use of ECMO against SARS-CoV-2 virus and thus improve the management of this novel disease.
Conclusion
Managing patients with IE and COVID-19 poses many challenges. Addionally, performing cardiac surgery in such unusual circumstances may be hazardous. For these reasons, heart team members involving cardiologists, anesthesists and cardiac surgeons should hold urgent meetings to discuss problematic cases such as young and healthy patients with IE but in critical condition due to COVID-19 in order to make a decision to continue medical therapy or to undergo cardiopulmonary bypass.
Cardiac surgery and bypass in active phase of COVID-19 may alter the clinical course of SARS-CoV-2 infection or contrary may have a begnin course. This is still yet to be determined and more studies are necessary to guide the best approach.
References
- Go YY, Kim YS, Cheon S, et al. Evaluation and clinical validation of two field-deployable reverse transcription- insulated isothermal PCR assays for the detection of the Middle East respiratory syndrome-coronavirus. J Mol Diagn. 2017; 19: 817-827.
- Habib G, Erba PA, Iung B, et al. On behalf of the EURO- ENDO Investigators. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J. 2019; 40: 3222-3233.
- Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. The New England Journal of Medicine. 2020; 382: 1708-1720.
- Zhou P, Liu Z, Chen Y, et al. Bacterial and fungal infections in COVID-19 patients: A matter of concern. Infect Control HospEpidemiol. 2020.
- Li Y, Yao L, Li J, et al. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J Med Virol. 2020.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. Lancet. 2020.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020.
- Alshahrani MS, Sindi A, Alshamsi F, et al. Extracorporeal membrane oxygenation for severe Middle East respiratory syndrome coronavirus. Ann Intensive Care. 2018; 8: 3.
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020.
- Crotti S, Bottino N, Spinelli E. Spontaneous breathing during veno-venous extracorporeal membrane oxygenation. J Thorac Dis. 2018; 10: 661-669.
- Kurihara C, Walter JM, Singer BD, et al. Extracorporeal membrane oxygen¬ation can successfully support patients with severe acute respiratory dis¬tress syndrome in lieu of mechanical ventilation. Crit Care Med. 2018; 46: e1070-e1073.