Predictors of Adherence to Self-Care Amongst Patients with Type 2 Diabetes Mellitus in Bulawayo Central
Author(s): Usai Tecklah1*, Nyoka Ruth2, Wekwete Benhilda2, Mugani Mollen2, and Chirimubwe Ropafadzo2
1Department of Science Technology Design Education, Midlands State University, Zimbabwe.
2Department of Food Science and Nutrition, Midlands State University, Zimbabwe.
*Correspondence:
Usai Tecklah, Department of Science Technology Design Education, Midlands State University, Zimbabwe.
Received: 30 Aug 2024 Accepted: 05 Oct 2024
Citation: Tecklah U, Ruth N, Benhilda W, et al. Predictors of Adherence to Self-Care Amongst Patients with Type 2 Diabetes Mellitus in Bulawayo Central. Diabetes Complications. 2024; 8(4); 1-9
Abstract
Self-care behaviour adherence is the cornerstone in diabetes care. The success of long-term maintenance therapy for diabetes depends largely on the patients’ adherence to self-care behaviour. The objective of the study was to assess levels and predictors of adherence to self-care behaviour among adults with Type 2 Diabetes in Bulawayo central focusing mainly on Mpilo central Hospital health staff and diabetic patients. A cross sectional study was used in which interviewer administered questionnaires were used to collect data. The questionnaires instrument was designed to understand the content of the programmes on diabetes self-care, to determine the parameters which patients are required to adhere to, to identify accessible diabetic health care services, and to identify key outcomes that determine successful self-care. The Statistical Package for Social Science (SPSS) version 20.0 were employed for analysis of collected. Descriptive statistics, the chi-square was employed to determine the presence of association between adherences to self-care behaviour with other variables (p<0.05) at P-value less than 0.05 while logistic regression was performed to identify independent predictor’s self-care behaviour adherence selfcare domains inclusive of; diet, medication, self-monitoring of blood glucose, physical activity, foot care and diabetes complications examinations. The study showed that social support, dietary counselling, selfdetermination, perceived benefits of dietary regimen are significant facilitating predictors of good adherence to self-care. The study identified financial constraints, forgetfulness, lack of time, reluctance, and reliance on social support as major barriers resulting to poor adherence to self-care adherence particularly undertaking physical activity and foot care. The study recommends targeted interventions that strengthens educational programmes to educate individuals living with diabetes on the importance of self-care.
Keywords
Background of the Study
World Health Organisation [1] Diabetes describes diabetes as a group of metabolic disorders that is characterized by evident hyperglycaemia. It is associated with long-term complications which include neuropathy, retinopathy and nephropathy amongst a number of other complications. The cases of diabetes are steadily rising particularly in the low and middle economically developed countries than high economically developed countries [2,3]. Type 2 diabetes mellitus (M2DM) is a serious global health disease that has evolved due to rapid economic, social and cultural changes, ageing populations, increased urbanization and changes in dietassociated consumption of high caloric processed foods and beverages [4]. Sedentary lifestyles, reduced physical activity and certain unhealthy behavioural are associated with the development of M2DM [5]. It is estimated that diabetes mellitus will be the seventh leading cause of mortalities. 463.0 million adults between 20–79 years worldwide are diabetic with 79.4% living in low and middle economically developed countries [2-4]. It is predicted that by 2030, 578.4 million and by 2045, 700.2 million adults (20–79 years) will be living with diabetes respectively. Diabetes accounts for 4.2 million deaths globally [6,7]. In Africa, there is a high number of undiagnosed diabetes (60%) cases of the adult population (20–79 years). There are about 19.4 million individuals with diabetes in the African and it is predicted that cases will rise to 28.6 million and 47.1 million by 2030 and 2045 respectively [8,9]. Diabetes also accounts for 366,200 deaths in the African. Furthermore, 73.1% deaths are attributed to individuals under 60 years and most of these deaths occur in low and middle-income countries at a percentage rate of 41.8% and 58.2%, respectively and higher in women than men.
Lipscombe et al., [9] stipulates that the main goal in diabetes treatment is to adopt and adequately perform self-care management practices that in turn regulate blood sugar levels which avoiding complications that can alter the day-to-day life of the individual. Diabetes self-management is a key factor in controlling development of complications/reducing rates of re-admission [10,11]. Some hospitals adequately prepare patients through therapeutic advances through new technologies, development of medication drugs, education programmes so that they are able to self-manage after discharge. Despite hospitalisation and stabilisation from an acute care setting to home care setting, some patients succeed in selfmanagement while some patients still struggle evidenced by high and frequent attendance and hospitalisation of some patients.
Poor adherence to self-care in diabetes has broad socio-economic consequences and threatens national productivity and economic development initiatives in Zimbabwe. This study then seeks to identify in the Zimbabwean context, the determinants or factors, which may predict or act as the enablers of proper self-care practices among people who have T2DM. Health care workers and policy makers could then use these predictors as a standard information in planning and implementing strategies to help patients’ successfully self-manage diabetes.
Research Methodology
A cross sectional research design was used to carry out a survey on the predictors of adherence to self-care practices amongst adults who are living with type 2 diabetes mellitus. The study was conducted at Mpilo Central Hospital Bulawayo. The hospital is one of health care centre in Zimbabwe where regular diabetes care is provided to a large population in a structured way.
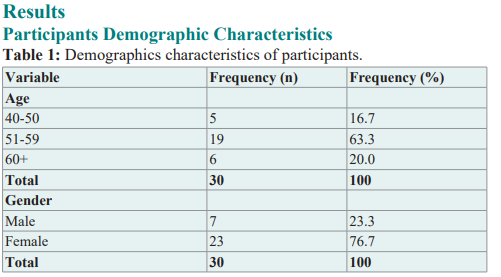
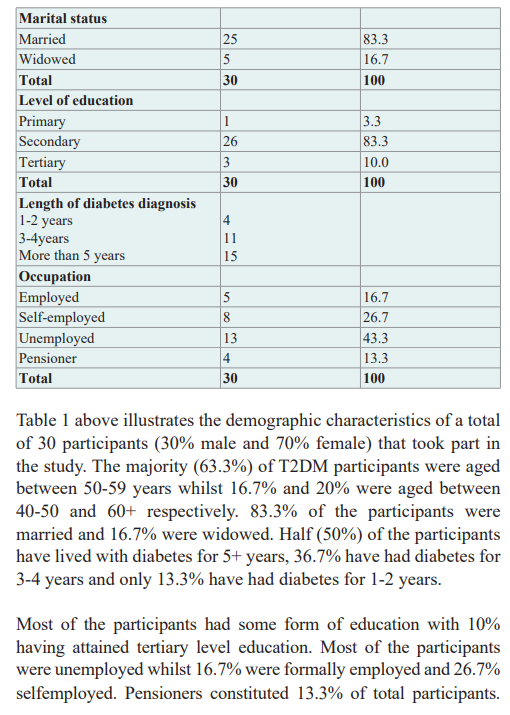
The study consisted of 5 health care providers and 30 male and female diabetic patients diagnosed with T2DM and on treatment. The inclusion criteria required participants who were diagnosed with T2DM for at least a year and within the ages of 30 and 65 years.
Convinience sampling was used to select 30 patients who took part in the study. Participants were selected basing on their availabiity during the time of data collection. Five health care provider (three hospital food service supervisors and the two doctors) participants were purposefully selected for informant interviews basing on their experience and interaction with diabetic patients.
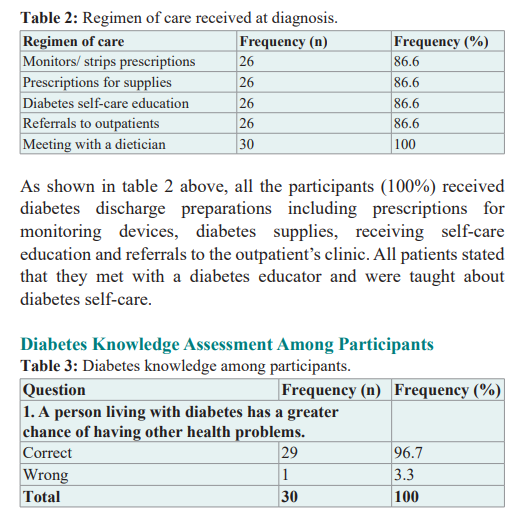
The data collection tools included a questionnaires for participants with T2DM and an interview guide for the health care providers. Key informant interviews were conducted with the health care providers incharge at the diabetes outpatients clinic. Interview questions formulated were to address the objectives of the study; to understand the content of the programmes on diabetes self-care, to determine the parameters which patients are required to adhere to, to identify accessible diabetic health care services, and to identify key outcomes that determine successful self-care.
The questionnaire was developed using variables from diabetes management questionnaire tools i.e. the Natividad revised diabetes self-management questionnaire designed by the Natividad Medical Centre from Monterey County of California, the Diabetes Case Manager Interview Guide from the care Path healthy engagements programme developed by Janssen pharmaceuticals and the diabetes self-management questionnaire (DSMQ) developed by Schmith, Gahr, Hermanns and Kalzer. The questionnaire open ended and closed ended questions where designed to provide information on; patient - participants personal and demographic characteristics, diabetes history, diabetes knowledge, dietary recommendations adherence, medication adherence, performance of SMBG, engagement in physical activity, risk reducing behaviours and stress management. The questionnaires were pretested to check clarity and suitability.
Data analysis were carried out using the statistical package for social sciences SPSS (version 20). The patients socio demographic characteristics, diabetets history and knowledge were analysed using frequency distribution tables. Level of adherence to the main self-care domains were analysed using the multiple response analysis tool to provide overall percentages. The Likert scale questions were scored (where never=0, rarely=1, sometimes=2, most times=3 and always=4) and categorized into adherence or non-adherence which was the dependent / outcome variable. All parameters assessed for each of the self-care domains were treated as the independent variables. Pearson chi-square test were used to assess strength of associations between the predictor variables and the outcome variables, while the logistic regression was used to identify the statistically significant predictors. A consent to carry the study was sought and granted by Midlands State University (Zimbabwe) Research Board (FSNnutri001/01/2020), and the Clinical Director of Mpilo central Hospital, Bulawayo. Participants signed consent forms after the aims and procedures of the research were explained. Participant’s names were excluded from the questionnaire for confidentiality purposes.
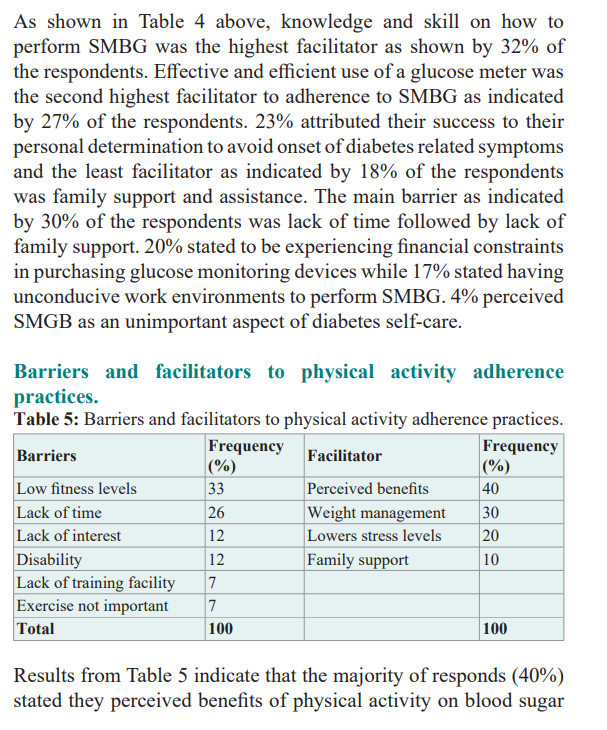
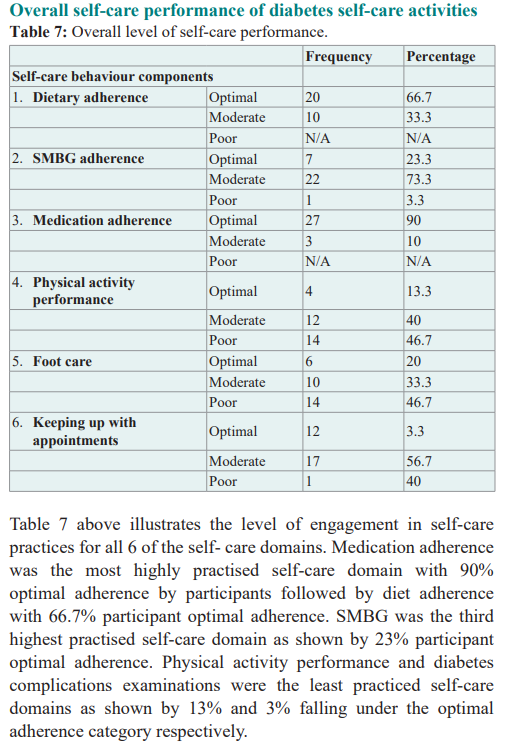
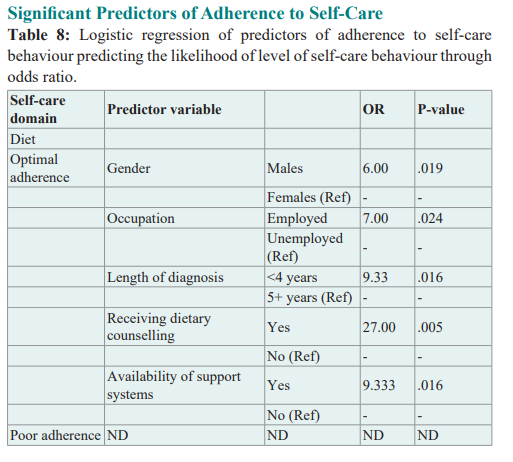
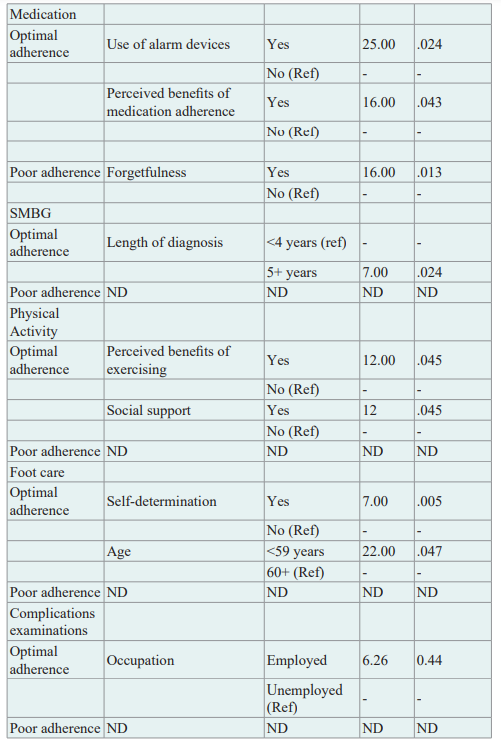
The results in table 8 above indicate the likelihood of level of selfcare behaviour through odds ratio. Variables that were significantly associated with diet adherence included gender, availability of family support, receiving dietary counselling, occupation status as well as length of diagnosis. Factors that were significantly associated with medication adherence included use of reminder apps and alarm devices, perceived benefits if medication and forgetfulness. Length of diagnosis was associated with adherence to performance of SMBG. Occupation status was also seen to be significantly associated with getting diabetes complications examinations performed. Under physical activity, several factors were found to be significantly associated with level of adherence to physical activity adherence. Factors included perceived benefits of exercise of blood glucose regulation, weight management, and family support, lack of time and length of diabetes diagnosis. Lastly age was associated with the level of daily foot care examinations.
Interview Responses
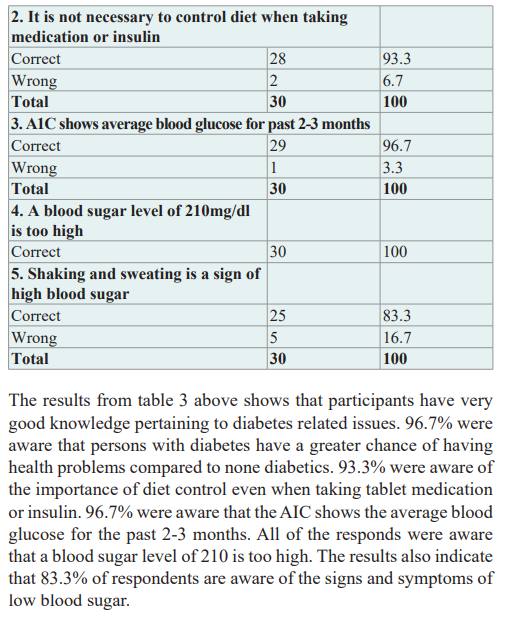
Interviews were carried out with the health care providers with the intention of identifying discharge programs for T2DM provided at health care facilities, to assess the self-care parameters targeted by these programs and to assess parameters that indicate self- care. They stated that they usually emphasize on health education during admission and after discharge of the patient. They make use of the acronym DIET to help patients fully understand and remember these self-care behaviours. D is an acronym for diet where they are they are advised to adopt certain dietary habits such as consuming more fruits, vegetables and whole grains, foods in fat and calories and cut down on animal products and confectionary. I an acronym for insulin injection i.e. and they are taught how to store insulin, the type of injections they can use to administer and how to selfadminister the insulin through injection sites. E is the acronym for exercise where they are advised to exercise for at least 30mins and choose activities they enjoy, such as walking, swimming or cycling. They are also advised checking the sugar levels or if they do not have glucometers they are advised to eat before exercising. T is the acronym for treatment. Depending on their type of Diabetes the medication prescribed is explained to them including the intervals of taking that medication. Glycated haemoglobin (A1C) test. Care carried out after every 2-3 months. The A1C level varies from patient to patient but the overall A1C target is set at 7 and below. Patients are advised to monitor and record their blood sugar and depending on the treatment plan they are advised to test their blood glucose four to eight times a day. Treatment options vary from insulin and oral medications a diet plan, maintaining a healthy weight and participating in regular activity also are important factors in diabetes self-care. Metformin (Glucophage, Glumetza, others) is generally the first medication prescribed for type 2 diabetes. Doctors use certain signs as indicators of trouble/ difficulty with the management of in any type of diabetes. These include hyperglycaemia, increased ketones in patient’s urine (diabetic ketoacidosis), hyperglycaemic hyperosmolar non-ketotic syndrome (Signs and symptoms of this life-threatening condition include a blood sugar reading over 600 mg/dL (33.3 mmol/L), hypoglycaemia and lose of excess weight.
Discussion
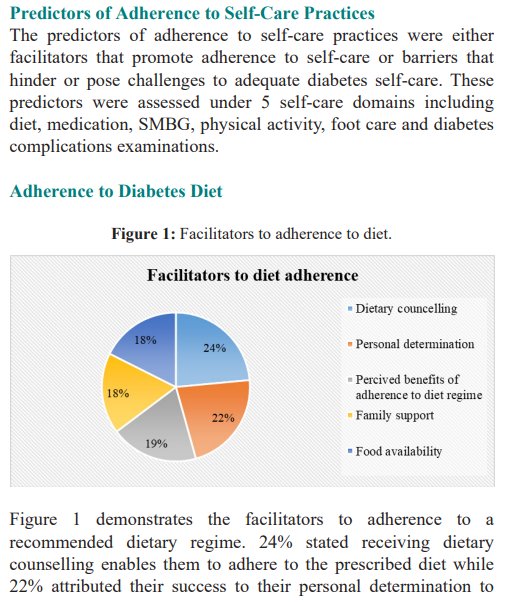
Diabetes self-care is an important aspect of diabetes management strategies which target lifestyle adjustments to achieve optimal glycaemic control in T2DM [10,11]. The study investigated the situation of adherence to self-care for T2DM adults and factors that determine the efficiency of adherence to self-care behaviours within the Bulawayo central district. The study showed that diet adherence, a necessity for effective therapy and regular glycaemic control [3], was the second most achieved self-care domain. Significant predictors of good adherence to dietary factors included demographic characteristics such as gender, occupation and length of diabetes diagnosis, patient’s self-determination to keep blood glucose levels normal, receiving dietary counselling and family support.
Males were more likely to be adherent to dietary recommendations compared to females. This may be attributed to the availability of support systems in males compared to females e.g. their spouses could be their support systems especially in the preparation of food which in turn assists males to be more adherent. Contrary to a study by Alhariri et al., [12] amongst the Yemeni society women were more amenable to diet adherence than men mainly because in the Yemeni society food preparations are usually done by females which better explains adherence to the dietary regimen compared to men. Participants who were employed were more likely to be adherent to dietary regimes compared to those who were nonemployed this is in line with a study carried out in Yemen where employed participants were more likely to be adhere to diet regimen than the unemployed ones. Being employed would mean having a source of income which will then enable them to secure food and be able to be adherent to demands of dietary regimen [10,11].
Participants with a shorter diabetes duration were more likely to be adherent to dietary regimes compared to those with a longer diabetes duration. A possible explanation for this could be increased awareness amongst patients with a shorter diabetes duration due to regular diabetic dietary counselling campaigns and patient education at diabetic clinics.
Participants’ perceived benefit of a diet adherence in regulating their blood sugar was a significant predictor of diet adherence. Adhering the recommended diet regimen helped in the regulation of glucose levels. This is consistent with a study carried out by Mulligan et al., [13] where participants believed that healthy eating was a way to manage their diabetes and stay healthy. Another facilitator was receiving dietary counselling by health workers on what foods to consume to their benefits which is highly evidenced by the fact that all participants receive dietary counselling during admission and after discharge (through) attendance diabetes classes. Availability of support systems was also cited as a significant facilitator in diet adherence as they help with food preparations, as well as financial support.
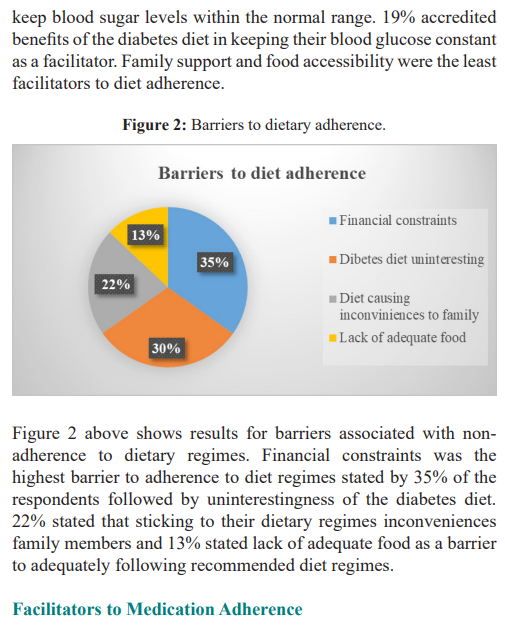
Stress was significantly associated with non-adherence to dietary recommendations (p< 0.05). Some of the stressors mentioned by participants were financial constraints, being unable to cope with diabetes demands, which are some of the important determinants in the adherence to dietary regimen. Diet adherence was found to be a stressor as it affected dietary aspects such as correct food choices, meal frequencies, meal timings and composition. Cost of food was the major reason for non-adherence to recommended diet. This is evidenced by 20% of participants who stated that they did not afford food. This may be attributed to the regular increases in food costs that are being experienced in the country which negatively affects patient’s access to the recommended diet. Another barrier included having to eat the same food as the rest of the family to avoid inconveniences. This in turns makes it challenging diabetes individuals to follow recommended diets that are different from the rest of the family.
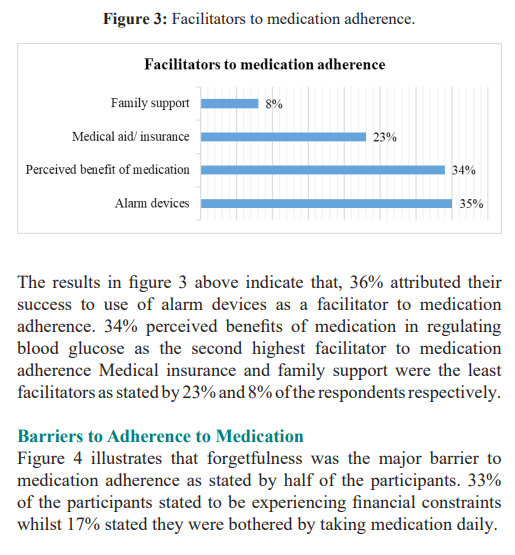
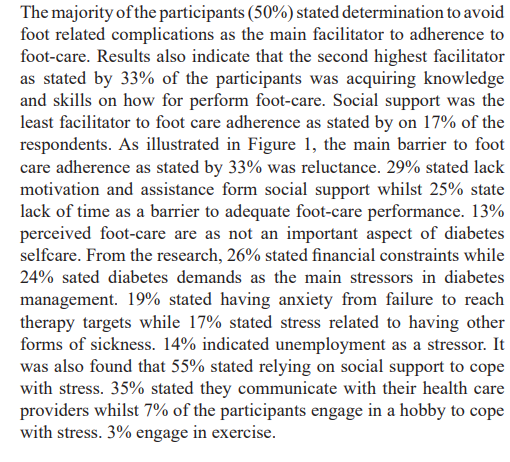
Medication adherence (90%) is the most achieved self-care domain in this study. This is in-line with a study carried out in by Ayele et al., [14] in Harare where medication adherence was the most archived self-care domain relative to physical activity, diet, glucose monitoring. One of the main significant facilitators of medication adherence was the perceived benefits of medication in the control of blood sugar. Participants who found that medication was associated with positive health outcomes were more likely to be adherent than respondents who did not. Participants who made use of reminder applications or alarm devices more likely to be adherent. This is also in line with a study carried out by M.D. et al., [15] where participants who stated that the use of reminder applications as alert devices improved medication adherence behaviours. Family support viewed in the study as a contributor to medication adherence through reminding and collection or purchasing of medication. Having medication insurance was seen as a facilitator to medication adherence although not statistically significant.
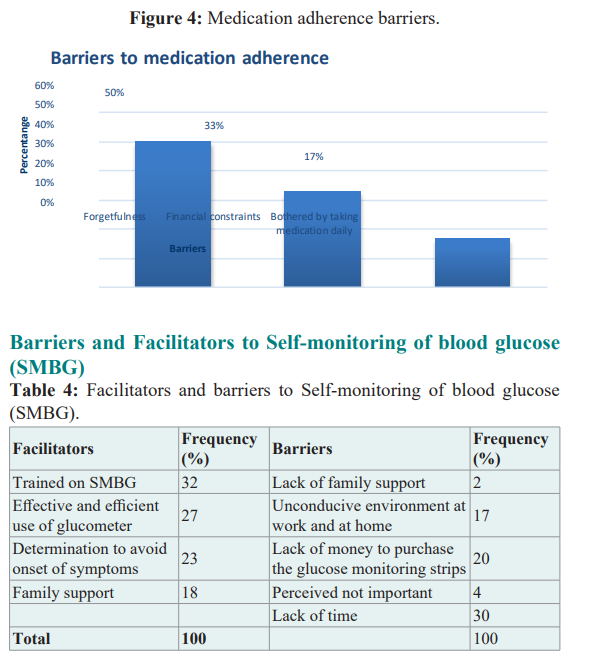
Non-adherence to diabetes medication was mainly associated with factors such as forgetfulness, being away from home and lack of finance. Forgetfulness was significantly associated with non-adherence to medication and this was consistent with a study carried out by Hernández-Ronquillo et al., [16] where most patients who took hypoglycaemic drugs stopped taking them mainly due to forgetfulness and being away from home. Lack of finance affected the ability to purchase diabetes supplies such as medication/ insulin.
Logistic regression indicated that participants who were diagnosed for more than 5 years were likely to perform optimal SMGB compared to those with a shorter diabetes duration. These findings are consistent with a study carried out by Hagerstrom, [17] who discovered that the longer individuals has lived with diabetes, the more frequently they monitored their blood sugar. SMBG does not affect actual blood sugar levels, but provides the patient with information on the current sugar levels which then act as indicators for intervention measures. As diabetic individual ages, more intense blood glucose monitoring is required and since the length of diabetes may be associated with progression of beta cell dysfuctioning and development of diabetes related complications, such factors can act as catalysts in encouraging more active performance of diabetes self-care [10,11]. These findings can also be attributed to better acceptance of the disease condition self- efficacy of the individual enabling them to become proficient with the self-care behaviours and how to incorporate them in their of lifestyles [5]. In this study facilitators such as acquiring knowledge and skill on how to perfume SMBG as well as effective and efficient use of a glucose meter, although not statistically significant, were stated parameters that were attributed to success in SMBG. This is in line with a study by Gertie [18], were glucose monitors, and insulin pumps acted as supporting tools, which enhanced better self-management of diabetes. Patients owning glucose metres were said to be more likely to adhere to self-care practices compared to those without. Studies have shown that psychosocial and economic factors such as low self-efficacy, interferences with lifestyle, inconveniences, pain and cost are hindrances that can adversely affect adherence to self-monitoring [10,11,13]. The study showed that lack of time due to busy schedules, lack of assistance and financial constraints were hindrances to adherence to self-care practices, adherence to SMBG and eventually poor glycaemic control. Lack of money would cause failure to access glucose strips and monitors [20].
Physical activity was the least practiced self-care domain. This study mainly focused on adults aged 45 years and above and it is around that age that older adults experience a decline in motor abilities as well as comorbid disease making it difficult to perform regular physical exercises [5]. The study showed that perceived benefits of exercise was a significant predictor of adherence to physical activity. Patients are likely to engage and maintain in a certain behaviour when they feel that a behaviour is beneficial to them or associated with positive health outcomes. This is what most participants who were adherent to physical activity stated, they found that adhering to physical activity helped keep their blood glucose levels normal. Social influence is able to predict intention to engage in physical activity, a patient’s high adherence rate to physical activity is highly influenced by pressure from the support system i.e. the spouse, family members, friends and health care providers [10,11,21]. This was evident in the study. Participants with family support were more associated with the intention to perform optimal physical activity compared to those without. In the study, the need to be healthy, wanting to lose weight or maintain weight was a significant predictor of adherence to exercise. Although no factors were significantly associated with poor adherence to physical activity, 31.1% of the participants mentioned perceived low levels of fitness as a factor associated with noncompliance to physical activity. This result was also found in a study by Shiriyedeve et al., [22] were there was a weak negative correlation between age and physical activity levels, as diabetes patients got older their physical activity levels decreased (Table 8). Other factors associated with poor adherence to physical activity were lack of interest and time especially amongst the employed due to busy work schedules.
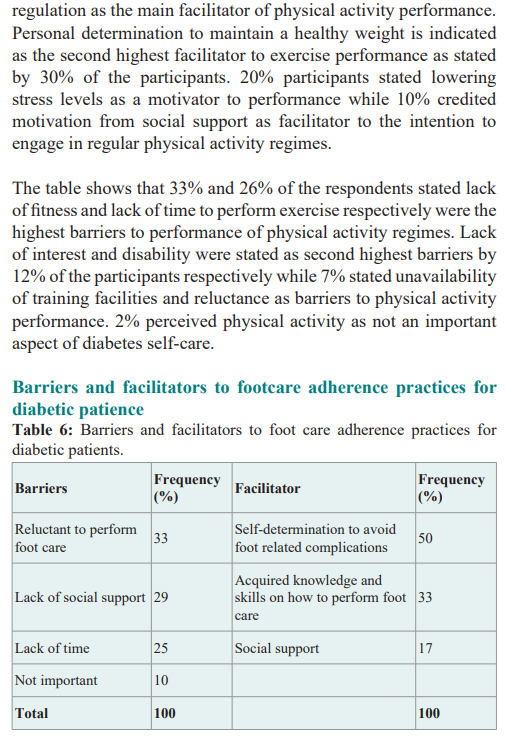
In this study there were significant relationships between adherence to foot-care and diabetes duration, determination and reluctant. Participants who were aged <60 were more to foot care performance compared to the ones who have had a short diabetes duration. This could be attributed to the fact that the elderly are more prone to diabetes related complications. It motivates them to actively engage in foot care practices compared to the newly diagnosed. Determination to avoid foot related complications was associated with adherence to daily foot care examination. Participants with self-determination were more likely to be adherent to foot care compared those without. This then explains why having a higher level of perceived susceptibility to diabetes complications increase the intention to perform foot care. Although not significant in this study, other facilitators stated by respondents, that help facilitate the performance of foot care included family support and receiving knowledge on how to carry out foot care. Reluctance to carry out foot examinations was highly associated with poor adherence to self-care. This means that participants do not perceive the importance of carrying out foot care examinations compared to all the other self-care, which eventually leads to then negligence.
Conclusion
The study showed that participants were highly knowledgeable on issues relating to diabetes. Facilitators such as having social support, receiving dietary counselling, financial stability, selfdetermination, and perceived benefits of regimen having a longer diabetes duration were identified in the study as significant predictors of good adherence to self-care. The study identified barriers such as financial constraints, forgetfulness, busy work schedules, reluctance, age and reliance on social support as predictors of poor adherence to self-care adherence particularly to physical activity and foot care. Optimal adherence were in medication and diet. Adherence to physical activity, foot care and diabetes complications examinations were the least practiced selfcare domains.
References
- Good CB, Kolb NR, Meyer M. World health organization guidelines on medicines for diabetes treatment Ann intern med. 2018; 169: 398-400.
- Dennis JM, Mateen BA, Sonabend R, et al. Type 2 diabetes and COVID-19 related mortality in the critical care setting a national cohort study in England March-July 2020. Diabetes 2021; 44: 50-57.
- Fina Lubaki JP, Omole OB, Francis JM. Glycaemic control among type 2 diabetes patients in sub-Saharan Africa from 2012 to 2022 a systematic review and meta-analysis. Diabetol Metab 2022; 14: 134.
- Yuen L, Saeedi P, Riaz M, et Projections of the prevalence of hyperglycaemia in pregnancy in 2019 and beyond Results from the International Diabetes Federation Diabetes Atlas. Diabetes res clin pract. 2019; 157: 107841.
- Tokhirovna EG. Risk factors for developing type 2 diabetes Education Science And Innovative Ideas In The World. 2024; 36: 64-69.
- Massika N. Type 1 and Type 2 Diabetes Mellitus Worldwide.
- Hailu SS, Ababiya RH, Nurfeta RA, et al. Knowledge and Attitude Towards Insulin Therapy in Type 2 Diabetes Mellitus Patients and Associated Factors at an Adult Endocrine Clinic of SPHMMC Addis Ababa Ethiopia. Int J Diabetes Endocrinol. 2024; 9: 22-38.
- Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes res clin pract. 2019; 157:
- Lipscombe L, Butalia S, Dasgupta K, et al. Pharmacologic glycemic management of type 2 diabetes in adults 2020 Can J Diabetes. 2020; 44: 575-591.
- ElSayed NA, Aleppo G, Aroda VR, et al. 8 Obesity and weight management for the prevention and treatment of type 2 diabetes Standards of Care in Diabetes-2023. Diabetes care. 2023; 46: S128-S139.
- Groothof D, Bais T, Bakker SJ, et al. Association of body weight time in target range with the risk of kidney outcomes in patients with overweight/obesity and type 2 diabetes Diabetes Care. 2024; 47: 371-378.
- Alhariri A, Daud F, Almaiman A, et Factors associated with adherence to diet and exercise among type 2 diabetes patients in Hodeidah city Yemen. Diabetes Manag. 2017; 7: 264-271.
- Mulligan K, McBain H, Lamontagne-Godwin F, et Barriers to effective diabetes management a survey of people with severe mental illness. BMC Psychiatry. 2018; 18: 1-15.
- Ayele BH, Mengesha MM, Tesfa T. Predictors of self-care activities of outpatient diabetic residents in Harar and Dire Dawa A hospital-based cross-sectional study. SAGE Open 2019; 7.
- Mary DA, Usman HM, Aduli EO, et al. Enablers and barriers to effective diabetes self-management A multi-national PLoS ONE. 2019; 14: e0217771.
- Hernández-Ronquillo L, Téllez-Zenteno JF, Garduño-Espinosa J, et al. Factors associated with therapy noncompliance in type-2 diabetes patients. Salud Publica Mex. 2003; 45: 191-
- Hagerstrom GE. Personal Factors Perceptions Influences and Their Relationship with Adherence Behaviors in Patients with Georgia State University. 2010.
- Davis B, Jansen C. Educating vulnerable communities about diabetes Can a fotonovela work. Health Education Journal. 2024; 83: 269-281.
- Vidal Florc M, Jansà Morató M, Galindo Rubio M, et al. Factors associated to adherence to blood glucose self- monitoring in patients with diabetes treated with insulin. The dapa Endocrinol Diabetes Nutr. 2018; 65: 99-106.
- Wambui Charity K, Kumar AMV, Hinderaker SG, et al. Do diabetes mellitus Patients adhere to self-monitoring of blood glucose SMBG Experiences from a SMBG program in western Diabetes Res Clin Pract. 2016; 112: 37-43.
- Mirahmadizadeh A, Khorshidsavar H, Seif M, et Adherence to Medication, Diet and Physical Activity and the Associated Factors Amongst Patients with Type 2 Diabetes. Diabetes Therapy. 2020; 11: 479-494.
- Shiriyedeve S, Dlungwane TP, Tlou B. Factors associated with physical activity in type 2 diabetes mellitus patients at a public clinic in Gaborone Botswana in 2017. Afr J Prim Health Care Fam 2019; 11: e1-e7.