Prevalence of Major Neurocognitive Disorder in Patients Admitted with Hip Fractures and the Associated Postoperative Delirium and Other Surgical Outcomes - A Prospective Cohort Study (Hippod Study)
Author'(s):Tammy KW Yuen1*, Mandy HM Chu1, Sally KY Liu2, Iris PF Chan2 and Frank SN Leung2
1 Department of Anaesthesia, Pamela Youde Nethersole Eastern Hospital, Chai Wan, HKSAR.
2 Department of Occupational Therapy, Pamela Youde Nethersole Eastern Hospital, Chai Wan, HKSAR.
*Correspondence:
Tammy Ka Wai Yuen, Department of Anaesthesia, Pamela Youde Nethesole Eastern Hospital, 3 Lok Man Road, Chai Wan, Hong Kong.
Received: 20 Jan 2021; Accepted: 21 Feb 2022; Published: 26 Feb 2022
Citation: Tammy KW Yuen, Mandy HM Chu, Sally KY Liu, et al. Prevalence of Major Neurocognitive Disorder in Patients Admitted with Hip Fractures and the Associated Postoperative Delirium and Other Surgical Outcomes - A Prospective Cohort Study (Hippod Study). Anesth Pain Res. 2022; 6(1): 1-7.
Abstract
Introduction: Major Neurocognitive disorder (NCD) and hip fractures are two serious problems in aging population. They are associated with morbidities including postoperative delirium (POD). We aimed to look at the prevalence of major NCD in hip fractures in our locality and their association with POD.
Methods: It was a prospective cohort study. Patients ≥ 65 years old with hip fractures communicable in Cantonese were included. They were screened with Hong Kong Montreal Cognitive Assessment 5-min protocol before operation. They were reviewed postoperatively with 3-Minute Diagnostic Interview for Confusion Assessment Method to assess the presence of POD. The primary outcome was the incidence of delirium between patients with or without preoperative major NCD. Secondary outcomes including surgical outcomes and length of hospital stay were investigated.
Results: The study was conducted between November 2020 and March 2021. One hundred ninety-two patients were screened, and 122 patients were included. Among the 192 patients screened, 97 (50.5%) were found to have major NCD. POD was found in 68.1% and 21.3% of patients with or without major NCD respectively. (p<0.001, odds ratio 4.857 (95% CI 2.046-11.531)). Total length of stay in hospital was longer when POD developed (p<0.05).
Conclusion: High prevalence of major NCD was found in geriatric hip fracture patients. Pre-existing major NCD was an independent risk factor in developing POD. Both major NCD and POD were prevalent but not sufficiently addressed in our locality. A multidisciplinary collaboration between anesthetists, geriatricians and allied health workers may help to prevent POD and reduce its severity.
Keywords
Introduction
Geriatric hip fracture is a global problem in aging population. It is associated with morbidities and high mortality [1,2]. The consequences are to not only patients but also their caretakers and the healthcare system. Different societies were trying to tackle this problem over the last decades however the outcomes were inconsistent [3]. One of the major postoperative morbidities was postoperative delirium.
Postoperative delirium (POD) is a postoperative state in which patients have disturbance of consciousness accompanied by impaired attention or ability to focus that cannot be explained by a pre-existing neurocognitive disorder. POD is associated with extended lengths of hospital stay, increased morbidities, and subsequent functional and cognitive decline [4,5]. Patients who have femoral neck fractures experience delirium three times more than patients undergoing non-orthopedic surgeries [6]. The incidence of POD in patients receiving surgeries for hip fractures varies between 9% to 65% from different studies due to the various criteria in defining delirium and heterogeneous clinical settings [7]. One local study demonstrated a 21.3% incidence of developing POD in orthopedic patients [8]. This figure included both patients with and without preoperative cognitive impairment. We expected the figures to be higher in the cognitive impaired group.
Patients with major NCD coming for hip surgeries might have more issues as with poorer capability in adapting to strange environment and tolerance to pain. The associated problems with major NCD will complicate the course of hospital stay and subsequent outcomes. The evidence for effective management and prevention of major NCD is still inadequate so far [9].
According to the figures quoted by the Legislative Council in 2017, prevalence of major NCD in Hong Kong was 5-8% among age over 65 [10]. We were expecting a severe under-reporting of this disease and it would be on the rise over the past few years. As with the shared risk factors for major NCD and hip fractures [11], the prevalence of major NCD in hip fracture patients was expected higher and was reported up to 75% [12-16].
In this study, we would like to survey the prevalence of major NCD in hip fracture patients in our locality and their associated surgical outcomes especially postoperative delirium comparing to patients without major NCD.
Methods
This was a prospective cohort study. Patients ≥ 65 years old admitted to Pamela Youde Nethersole Eastern Hospital (PYNEH) with hip fractures were screened with Hong Kong Montreal Cognitive Assessment 5-min protocol (HK-MoCA 5-min protocol). They were included if they were communicable in Cantonese and able to complete the HK-MoCA 5-min protocol.
The HKEC Research Ethics Committee approved the study. Informed consents were obtained from participants or their relatives according to their mental capacity. Due to COVID-19 pandemic during the study period, visiting was not allowed for non-critical patients. Verbal consents were obtained from the relatives over phone if the patient was not fit for consent. Written consents were obtained later in the relatives’ convenience.
Participants were excluded if they were not surgical candidates or unable to complete HK-MoCA 5-mins or scored zero in this test. Patients would only be recruited for their first operation if they had repeated operations during the same admission.
HK-MoCA 5-min protocol was used to assess the presence of major NCD as soon as possible after admission. Patients were excluded if the screening tests were not done before surgical fixation. HK- MoCA 5-min protocol was selected for the preoperative screening because it was easy to learn and administer. It was also shown to have high validity and was equally reliable as the full version of MoCA in patient screening [17-20].
Participants were reviewed postoperatively with 3-Minute Diagnostic Interview for Confusion Assessment Method (3D-CAM) to assess the presence of POD on postoperative day 1 to day 3, or on the day of discharge from the acute admission ward whichever earlier. The assessments were done by occupational therapists, anesthetists or nursing staffs who have been trained to perform the assessments on patients.
3D-CAM was selected for assessing postoperative delirium in our study. A standardized evidence-based tool enables non- psychiatrically trained staff to identify delirium quickly and accurately in both clinical and research settings [21-24].
The primary outcome was the incidence of postoperative delirium in patients with or without preoperative major NCD. We also measured a set of secondary outcomes including 30-day mortality, respiratory complications, cardiovascular complications such as acute coronary syndrome, congestive heart failure, new onset arrhythmia, thromboembolic events, gastrointestinal bleeding, acute renal failure as with creatinine >20% of the baseline, ICU admission, cardiac arrest, postoperative day 30 inpatient rate, new institutionalization, length of stay in acute admission ward and total length of hospital stay.
Statistics
We estimated 40% of our geriatric hip fractures patients had major NCD [11-16]. With a hypothesis that patients with preoperative major NCD would experience twice the risk in developing POD, a sample size of 120 patients was required to provide a power of 80% with 95% confidence interval. 122 patients were decided to be recruited to prepare for potential loss of data during follow-up.
Chi-Square test and Fisher’s exact test were used for categorical data. Mann-Whitney U test was used for continuous variables. All statistical analysis was done by SPSS Version 26. p-value <0.05 is considered significant.
In view of the bias associated with observational study, inverse propensity score weighting was used for data adjustment. Age, ASA classification, days of waiting before OT, mode of anesthesia and previous documented NCD were treated as potential confounders. Length of stay in acute ward and the presence of postoperative complications were also considered as factors potentially affecting the outcome. The predicted probability of each data was generated by performing binary logistic regression to each of the suspected confounders and factors affecting outcome. The weighting of each data set was then determined by using ATT (Average effect of the treatment on the treated) method (See Appendix 1).
Results
The study was conducted between 15th November 2020 to 28th March 2021. One-Hundred-ninety-two patients were screened of which 122 patients fulfilled the criteria and were included. The study was suspended between 7th December to 31st December 2020 due to severe manpower dearth in COVID pandemic.
Among the 192 patients screened, 97 (50.5%) were found to have major NCD. Only 13 of them were previously documented with this diagnosis. Three patients with documented NCD were not detected by the HK-MoCA-5min protocol.
Twenty-nine patients were excluded with MoCA score zero to eliminate possible preoperative delirium. Eighteen patients were excluded as MoCA test could not be done prior to operation. Other 12 patients were excluded for no consent. Five patients were transferred out of PYNEH before surgery and 6 patients were excluded as operation was finally not done. No patient dropped out from the study after inclusion (Figure 1).

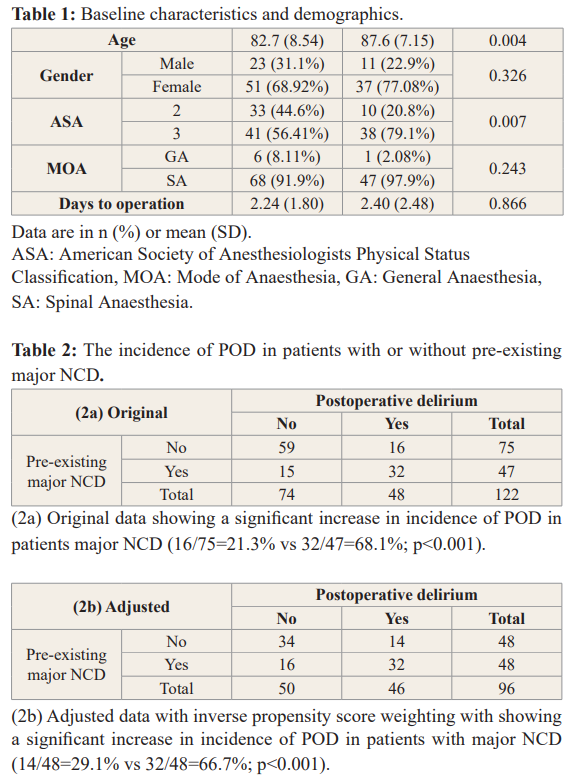
The mean age was 84.6 years old. Thirty-four (27.9%) patients were male and 88 (72.1%) were female. Major NCD was found in 48 (39.3%) patients while 74 (60.7%) patients were not. The baseline characteristics and demographics were shown in Table 1.
Forty-seven (38.5%) patients developed POD. Patients with pre- existing major NCD had a significant increased incidence of POD compared with patients without major NCD (32/47=68.1% vs 16/75=21.3%; p<0.001, See Table 2a).
Age and ASA classification were significantly correlated to preoperative NCD. In view of observational study subjected to bias from various confounding factors, inverse propensity score weighting was used for data adjustment to minimize bias caused by confounding factors.
After adjustment, we found that patients with pre-existing major NCD still had a significant increase in incidence of POD compared with patients without major NCD (32/48=66.7% vs 14/48=29.1%; p<0.001, Table 2b) with an odd ratio of 4.857 (95% CI 2.046- 11.531).
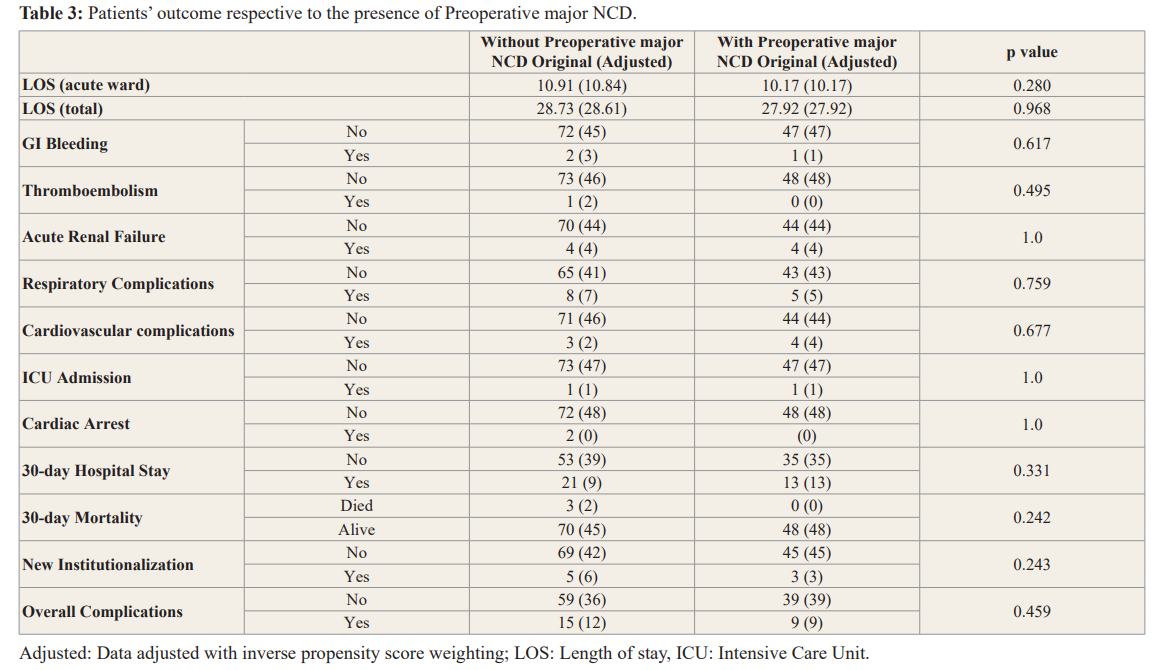
There was otherwise no significant difference in the secondary out comes measured (Table 3).
These secondary outcomes were also compared between patients who developed POD and those did not. We found that the total length of hospital stay (LOS) was significantly longer in the group of patients who developed POD (29.95, 95% CI 26.69-33.2 vs 26.87, 95% CI 24.03-29.71; p<0.05). (Table 4).
Discussion
High prevalence of major NCD was found in our patients. This was 50.5% in the total screened patients and 39.3% in included patients. The high prevalence should draw the attention from the public and the authorities.
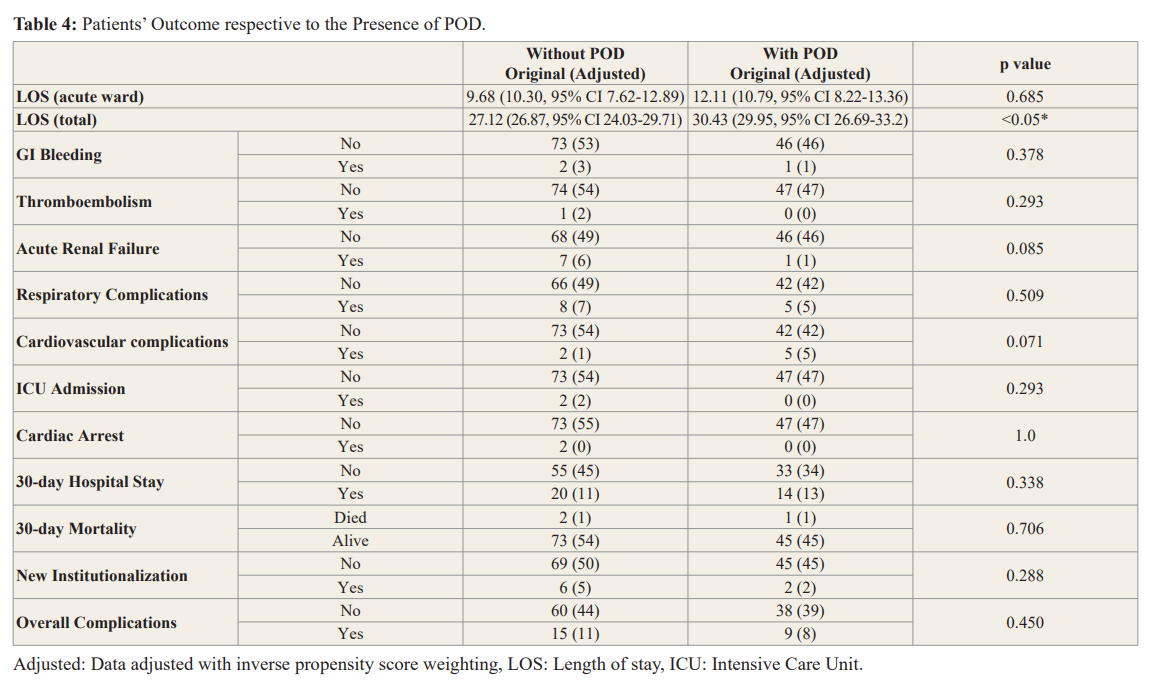
The LOS was significantly longer in patients developed POD (29.95, vs 26.87; p<0.05) which was consistent with previous studies [28]. The reason for prolonged stay was not further investigated. We expected the functional status was largely compromised when POD was developed which affected their capability for discharge. Multiple workups might also be done to rule out organic causes of delirium which prolonged their stay. The overall pressure put to the healthcare system was increased with increased cost and resources.
Major NCD was found severely under-reported. Among the 97 patients identified with major NCD in our study, only 13 (13.4%) were previously documented to have similar findings. Most of our MoCA tests were done shortly after admission. We expected a minimal impact on the score by the hip fracture. We were not surprised by the under-reporting of this disease. The stigmatization and confusion with normal aging contributed to the major barriers in disease recognition. More resources should be allocated to ameliorate this deficit in our service.
POD was also under diagnosed. Studies reported that more than 50% of patients with delirium were undiagnosed [31,32]. POD was easily missed as delirium assessment has never been a parameter to measure routinely during postoperative period. Most of the medical staff are not familiarized with the techniques and components of delirium. It might be misdiagnosed as residual anaesthetic effects. We collaborated with occupational therapists in our study for cognitive assessment. However, after appropriate training and practices, any medical professionals could actually conduct CAM. Our nurses in operating theatre were able to carry out this assessment after a few weeks of training. We encourage the use of various assessment tools in detecting NCD and POD so to enhance early detection and management.
Pre-existing major NCD is an important risk factor for POD. This was not only shown in our study but also in previous literature [28]. This association was also found in non-surgical patients, which highlighted the independence and significance of major NCD to delirium in hospitalized patients. A recent study of non-surgical patients reported pre-existing major NCD as the main risk factor for delirium after hospitalization [29]. Previous studies revealed that delirium might be preventable in 30-40% of hospitalized elderly patients [33,34]. Identification of high-risk patients could be helpful in preventing POD. A comprehensive delirium prevention and intervention program could reduce the incidence and severity of delirium as well as shorten the duration of the episode. These include environmental control, reorientation, optimized oxygenation and hydration, infection control, early mobility, appropriate pain management, medication review, nutritional support, sleep hygiene, hearing and visual aids [35]. Before we are able to handle delirium effectively, it would be essential to initiate the routine assessment of cognitive function and confusion status. It would be a gorgeous movement to launch such in clinical practices but worth it to implement. We would like to suggest hospitals to form groups for cognitive and confusion screening preoperatively on geriatric hip fracture patients. Proactive geriatric or psychiatric consultation may decrease the risk of POD. Geriatricians, anesthetists and other involved healthcare professionals should work together as a multidisciplinary team for successful management of POD.
Three patients known to have major NCD preoperatively were not detected by HK-MoCA-5min protocol. Although both HK- MoCA and HK-MoCA 5-min protocol have very high sensitivity, specificity and correlation, there may still be discrepancies and inaccuracies. We did not have detailed information on their previous documented major NCD and the tests they received for diagnoses for those three patients.
There were several limitations in our study. Firstly, this was an observational study without randomization for patients with and without major NCD. Age and ASA score were found to be significantly associated with the presence of preoperative major NCD. Hence, inverse propensity score weighting was used for data adjustment to minimize the bias from confounding factors. The premorbid status was also not explored in detail. Therefore, other potential risk factors such as pre-existing cardiovascular or cerebrovascular events were not investigated for their contribution to POD and other secondary outcomes. Six patients were only assessed with 3D-CAM for 1 day postoperatively as they were discharged shortly after operation. This might underestimate the overall figure of POD. Moreover, this study was performed in a single institute, which might be subjected to selection bias. It would be more preferable if more hospitals would perform similar assessment for the risk factors contributing to POD. This would help in increasing awareness and training of various medical professionals in performing assessment tests in routine clinical practices.
Conclusion
High prevalence of major NCD was found in hip fracture patients up to 50.5%. Pre-existing major NCD was shown an independent risk factor for developing POD with an odd ratio of 4.857 (95%CI 2.046-11.531). Both major NCD and POD were commonly seen and were overlooked in our clinical settings. A multidisciplinary approach to identify patients with major NCD and those at risk for POD might help to prevent POD and reduce its severity.
Acknowledgement
Special acknowledgement to the following Colleagues in PYNEH Mr. L C Mok, Ms M Y E Chan from Department of Orthopedics and Traumatology.
Ms. Winnie Kwun, Mr Ricky Leong from Department ofOccupational Therapy
Dr. P Y B Ho, Ms W L Fung, Ms G K Hui, Ms K W Chan, Ms M K Cheng, Ms Y W Pang from Department of Anaesthesia.
References
1.Hempsall VJ, Robertson DR, Campbell MJ, et al. Orthopaedic geriatric care-is it effective? A prospective population-based comparison of outcome in fractured neck of femur. J R Coll Physicians Lond. 1990; 24: 47-50.
2.Laxton C, Freeman C, Todd C, et al. Morbidity at 3 months after hip fracture:data from the East Anglian audit. Health Trends. 1997; 29: 50-55.
3.Kates SL. Hip fracture programs: are they effective? Injury.2016; 47: 25-27.
4.Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014; 383: 911-922.
5.Kistler EA, Nicholas JA, Kates SL, et al. Frailty and Short- Term Outcomes in Patients With Hip Fracture. Geriatr Orthop Surg Rehabil. 2015; 6: 209-214.
6.Jagmin MG. Postoperative mental status in elderly hip surgery patients. Orthop Nurs. 1998; 17: 32-42.
7.Goldenberg G, Kiselev P, Bharathan T, et al. Predicting post- operative delirium in elderly patients undergoing surgery for hip fracture. Psychogeriatrics. 2006; 6: 43-48.
8.Tsang LF, Yeung CH, Tse CC, et al. Developing a predictive tool for postoperative delirium in orthopaedic settings in Hong Kong. International Journal of Orthopaedic and Trauma Nursing. 2012; 16: 147-159.
9.Larsson SC, Markus HS. Does treating vascular risk factors prevent dementia and Alzheimer’s Disease? A systematic review and metaanalysis. J Alzheimers Dis. 2018; 64: 657-668.
11.Susan M Friedman, Isaura B Menzies, Susan V Bukata, et al. Dementia and Hip Fractures: Development of a Pathogenic Framework for Understanding and Studying Risk. Geriatric Orthopaedic Surgery Rehabilitation. 2010; 1: 52-62.
12.Seitz DP, Adunuri N, Gill SS, et al. Prevalence of dementia and cognitive impairment among older adults with hip fractures. J Am Med Dir Assoc. 2011; 12: 556-564.
13.Gruber-Baldini AL, Zimmerman S, Morrison RS, et al. Cognitive impairment in hip fracture patients: timing of detection and longitudinal follow-up. J Am Geriatr Soc. 2003; 51: 1227-1236.
14.Formiga F, Lopez-Soto A, Duaso E, et al. Characteristics of fall-related hip fractures in community-dwelling elderly patients according to cognitive status. Aging Clin Exp Res. 2008; 20: 434-438.
15.Konstantina G Yiannopoulou, Ioannis P Anastasiou, Theodore K Ganetsos, et al. Prevalence of Dementia in Elderly Patients with Hip Fracture. Hip Int. 2012; 22: 209-213.
16.Kasai M, Meguro K, Ozawa H, et al. Fear of Falling and Cognitive Impairments in Elderly People with Hip Fractures. Dement Geriatr Cogn Disord Extra. 2017; 7: 386-394.
17.Wong A, Nyenhuis D, Black SE, et al. Montreal Cognitive Assessment 5-minute protocol is a brief, valid, reliable, and feasible cognitive screen for telephone administration. Stroke. 2015; 46: 1059-1064.
18.Lonie JA, Kalu UG, Ebmeier KP. A systematic review of cognitive screening for mild cognitive impairment. Mind Brain J Psychiatry. 2010; 1: 1-8.
19.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005; 53: 695-699.
20.Yeung PY, Wong LL, Chan CC, et al. A validation study of the Hong Kong version of Montreal cognitive assessment (HK-MoCA) in Chinese older adults in Hong Kong. Hong Kong Med J. 2014; 20: 504-510.
21.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: The Confusion Assessment Method. A new method for detection of delirium. Ann Intern Med. 1990; 113: 941-948.
22.Wong CL, Holroyd-Leduc J, Simel DL, et al. Does this patient have delirium?: value of bedside instruments. Jama. 2010; 304: 779-786.
23.Pisani MA. The 3D-CAM provides a brief, easy to use, sensitive and specific delirium assessment tool for older hospitalised patients, both with and without dementia. Evidence-Based Mental Health. 2015; 18: 120.
24.Marcantonio ER, Ngo LH, O'connor M, et al. 3Dâ?CAM: derivation and validation of a 3â?minute diagnostic interview for CAMâ?defined delirium: a crossâ?sectional diagnostic test study. Ann Intern Med. 2014; 161: 554-561.
25.S Deiner, JH Silverstein. Postoperative delirium and cognitive dysfunction. British Journal of Anaesthesia. 2009; 103: 141-i46.
26.Galanakis P, Bickel H, Gradinger R, et al. Acute confusional state in the elderly following hip surgery: incidence, risk factors and complications. Int J Geriatr Psychiatry. 2001; 16: 349-355.
27.Lee HB, Mears SC, Rosenberg PB, et al. Predisposing factors for postoperative delirium after hip fracture repair in individuals with and without dementia. J Am Geriatr Soc. 2011; 59: 2306-2313.
28.Iamaroon A, Wongviriyawong T, Sura-Arunsumrit P, et al. Incidence of and risk factors for postoperative delirium in older adult patients undergoing noncardiac surgery: a prospective study. BMC Geriatr. 2020; 20: 40.
29.Gual N, Morandi A, Pérez LM, et al. Risk factors and outcomes of delirium in older patients admitted to postacute care with and without dementia. Dement Geriatr Cogn Disord. 2018; 45: 121-129.
30.Wang Cg, Qin Yf, Wan X, et al. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J Orthop Surg Res. 2018; 13: 186.
31.Ritter SRF, Cardoso AF, Lins MMP, et al. Underdiagnosis of delirium in the elderly in acute care hospital settings: lessons not learned. Psychogeriatrics. 2018; 18: 268-275.
32.Bellelli G, Nobili A, Annoni G, et al. Under-detection of delirium and impact of neurocognitive deficits on inhospital mortality among acute geriatric and medical wards. Eur J Intern Med. 2015; 26: 696-704.
33.Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999; 340: 669-676.
34.Marcantonio ER, Flacker JM, Wright RJ, et al. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001; 49: 516-522.
35.Delirium: prevention, diagnosis and management. National Institute for Health and Care Excellence. Clinical guideline [CG103]. London. 2010.