Reduction of Recurrent Severe Hypoglycemia and Hypoglycemia Unawareness in Type 2 Diabetes by Treatment Modification and Diabetes Education
Author'(s): Jose G. Jiménez-Montero, MD, FACE1,2*, María Laura Carvajal-Solórzano, Bsc2and Mayra Villegas-Barakat, RD3
1Department of Endocrinology Hospital CIMA, San José, Costa Rica.
2School of Medicine, Universidad de Ciencias Médicas San José, Costa Rica.
3Department of Nutrition, Universidad de Ciencias Médicas San José, Costa Rica.
*Correspondence:
Dr. José G. Jiménez-Montero, FACE. Universidad de Ciencias Médicas, PO Box 638 -1007, Centro Colón, San José, Costa Rica. Phone 506 2208 130.
Received: 02 May 2020 Accepted: 25 May 2020
Citation: Jose G. Jiménez-Montero, María Laura Carvajal-Solórzano, Mayra Villegas-Barakat. Reduction of Recurrent Severe Hypoglycemia and Hypoglycemia Unawareness in Type 2 Diabetes by Treatment Modification and Diabetes Education. Diabetes Complications. 2020; 4(2); 1-7.
Abstract
Introduction: Intensification of diabetes treatment can induce hypoglycemia, representing a barrier to achieve glycemic control increasing the risks of adverse events.
Objectives: To describe changes in the frequency and severity of hypoglycemia following treatment modification in high-complexity type 2 diabetics (T2DM).
Material and Methods: T2DM patients with chronic diabetes complications presenting severe, recurrent and reduced awareness of hypoglycemia (RAH) were analyzed before and three months after treatment modification and diabetes education.
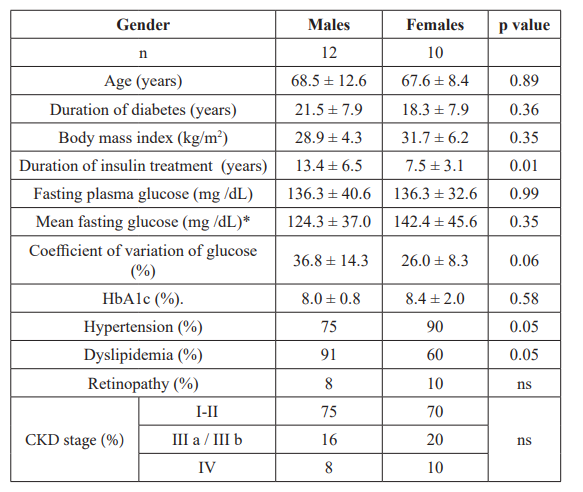
Results: Twelve males aged 68.5±12.6 years-old, BMI: 28.9 ± 4.3 kg/m2; glycosylated hemoglobin A1c (HbA1c) 8.0 ± 0.8% and ten females aged: 67.6 ± 8.4 years-old, BMI 31.7 ± 6.2.0 kg/m2, HbA1c 8.4 ± 2.0%, with multiple cardiovascular risk factors, previous cardiovascular disease or renal impairment, requiring insulin treatment alone or with oral agents, were evaluated. All had severe and recurrent hypoglycemia events. Nutritional counselling and diabetes education were provided to all the patients; the pharmacologic treatment was switched from human insulin to insulin analogues and to newer class of oral agents or to GLP-1 receptor agonists. With treatment modification and diabetes education, the frequency and severity of hypoglycemia events diminished. Further, mean insulin doses were reduced from 0.70±0.24 to 0.44 ± 0.9 U/Kg (p=0.01) and from 0.87 ± 0.41 to 0.47±0.21 U/Kg in males and females, respectively (p=0.0001). Concomitantly, HbA1c diminished in females (p=0.02) and for both males and females, the coefficient of variation of fasting glucose declined (p=0.03).
Conclusion: Recurrent severe hypoglycemia and RAH constitute a serious complication which hampers metabolic control and place patients at risk for cognitive dysfunction and cardiovascular complications. Reduction in the frequency, severity of hypoglycemia in high-complexity T2DM was observed after diabetes treatment modification.
Keywords
Introduction
Diabetes prevalence is rapidly increasing and represents a serious health problem worldwide [1-2]. Diabetes is associated with chronic complications, disabilities, premature death [3] and contribute to the impact on health care costs [4-5]. Long- term glycemic control reduces the risk of chronic complications and death [6-11].
In Latin America, it has been shown poor metabolic control and a high prevalence of microvascular and macrovascular complications in T2DM patients [12-14]. Along with these findings, all-cause mortality among people with diabetes doubles that of those without this condition [15]. Moreover, in Costa Rica, mortality due to diabetes nephropathy is increasing [16] and latest reports demonstrated inadequate metabolic control in our country [17].
Thus, actions have been taken to revert this trend. In consequence, the risks for hypoglycemia in people living with diabetes seem to be increasing. We previously described the occurrence of severe hypoglycemia in T2DM patients attended at the emergency department of a general hospital in San José, Costa Rica [18]. Yet, little is known with respect to hypoglycemia in T2DM patients attended in an out-patient settings in this country.
In this report we describe the clinical presentation, risk factors, potential causes of severe hypoglycemia and the effects of a short- term treatment modification inT2DM patients referred to our out- patient clinic. We aimed to raise glucose levels, avoid hypoglycemia and glucose variability in order to restore the sympathoadrenal response to hypoglycemia in high complexity T2DM.
Material and Methods
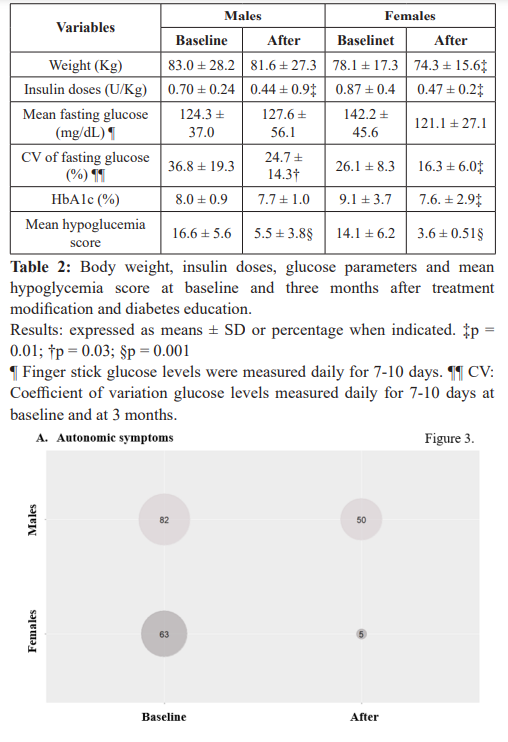
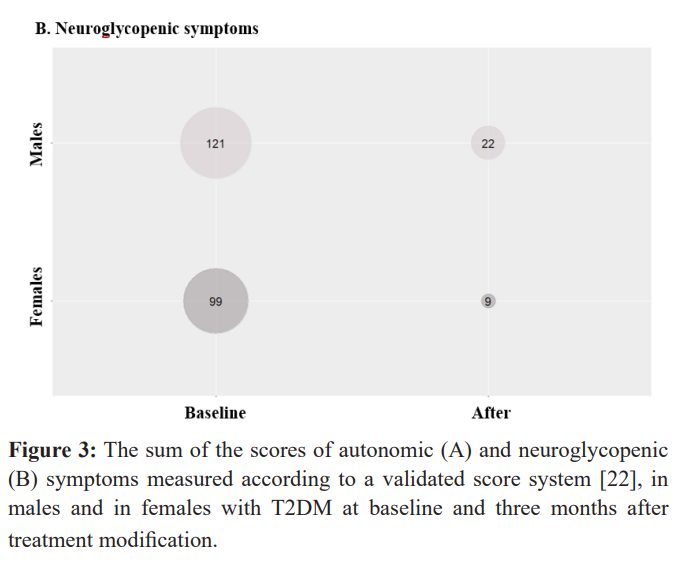
Twenty-two T2DM patients with long-term insulin usage and cardiovascular, neurologic or renal complications were referred to the Diabetic Clinic of Hospital CIMA due to severe, recurrent and RAH [19-21]. Hypoglycemia events occurred during the previous six months when insulin doses were changed aiming to improve glucose control. We used previously tested questionnaires to record the severity of the hypoglycemia events and to classify them according to a validated score system [22]. All the patients were accompanied with close relatives whom helped record hypoglycemia events. Age, sex, co-morbidities, clinical characteristics of the hypoglycemia events, it´s causes and risk factors were recorded. These events were register as an adverse event according to the regulation of the National System of Surveillance [23].
Nutritional counselling and diabetes education were provided to all the patients and family members as recommended [24-25] and consisted of: 1) understanding of the problem, 2) identification of hypoglycemia manifestations, 3) frequent capillary glucose monitoring, 4) personalized meal plan, 5) modification of pharmacologic treatment, 6) daily report of glucose monitoring and 7) treatment adjustment as necessary. The pharmacologic treatment was switched from human insulin to insulin analogues, to newer class of oral agents or to GLP-1 receptor agonists as necessary [24-25]. The patients were asked to make weekly telephone or email contacts with the health providers for insulin adjustments or dietary modifications. Lifestyle modifications, timing of insulin administration and meal patterns were closely supervised. The patients were seen monthly for three months. At each subsequent visit weight, hypoglycemia questionnaires, glucose monitoring and HbA1c were obtained. Results are expressed as mean ± SD. Differences between groups were analyzed using Student T test. All analyses were performed using Microsoft Excel and Epidat 4.2.
Results
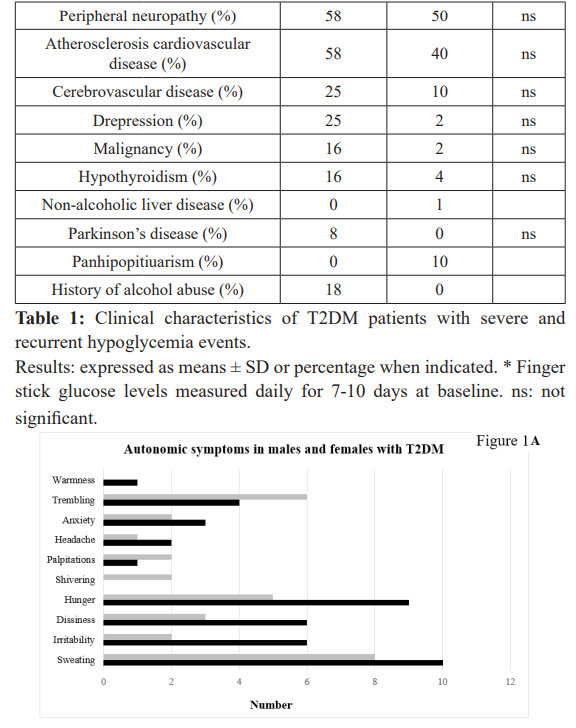
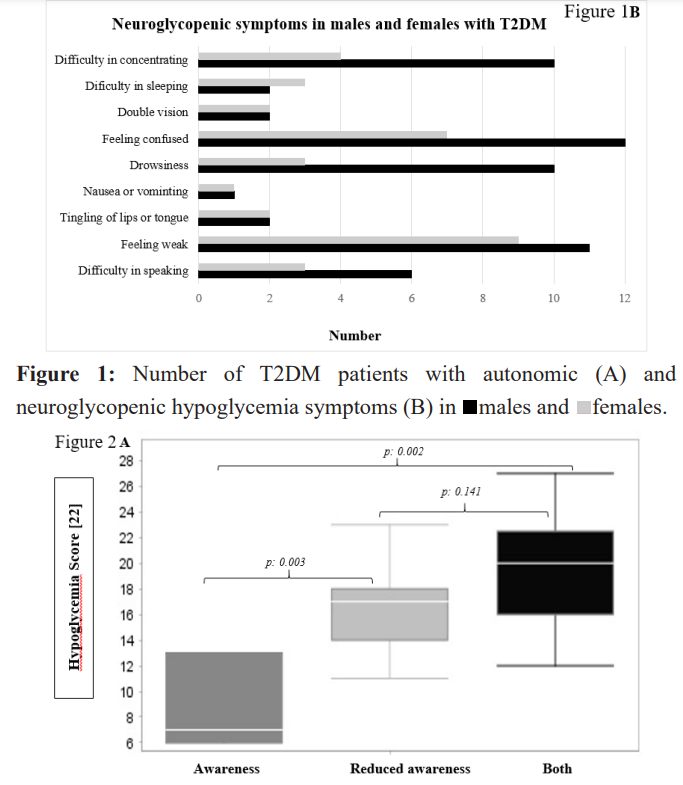
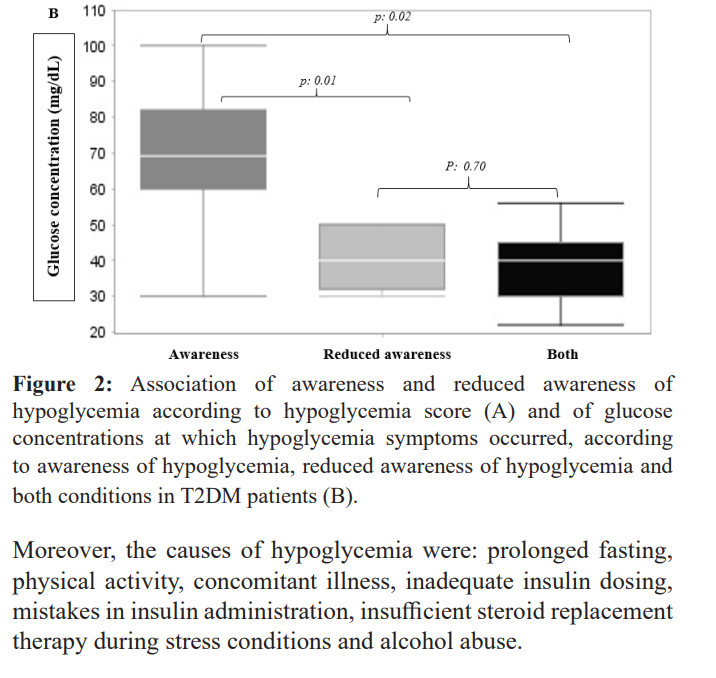
Twelve males (age: 68.5 ± 12.6 years old, BMI: 28.9±4.3 kg/ m2; fasting glucose:136.3 ± 40.6 mg/dL; HbA1c: 8.0±0.8%) and ten females (age: 67.6 ± 8.4 years old, BMI: 31.7 ± 6.2 kg/ m2, fasting glucose: 136.3 ± 32.6 mg/dL; HbA1c: 8.4 ± 2.0%) were evaluated. Baseline clinical characteristics are shown in table 1. The hypoglycemia events were documented by finger stick glucose levels measured at home, by paramedics or at the emergency department. There were five patients who had non- severe hypoglycemia and perceived hypoglycemia events within the past 6 months; however, they reported progression to reduced perception of hypoglycemia. Nineteen required third party assistance and twelve had cognitive dysfunction. Ten males and eight females presented RAH; three presented nocturnal jerks and jumps and other three had seizures. In eleven occasions emergency department/paramedic visits were required. The symptoms of the hypoglycemia events are illustrated in figure 1. As compared to females, more males had hypoglycemia symptoms. Based on those symptoms, T2DM patients were grouped as having awareness of hypoglycemia (n=5), RAH (n=9) or having both (n=7) according to the predominant symptom category. Patients with awareness hypoglycemia had lower hypoglycemia score and higher glucose concentrations at which the patients became symptomatic as shown in figure 2A and 2B, respectively.
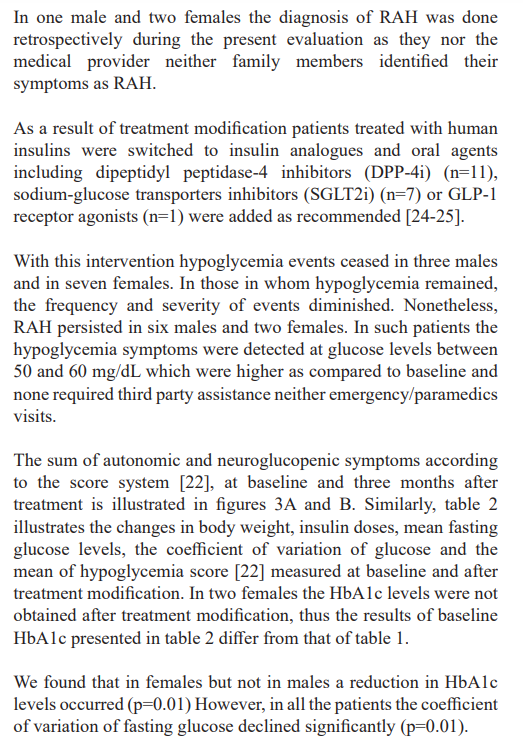
Discussion
Most clinical practice guidelines recommend aimed to HbA1c levels less than 6.5% to 7.0% [23-24]. In the UKPDS newly diagnosed T2DM patients changes of 0.9% in HbA1c over median 10.0 years resulted in a significant reduction of microvascular complications [7] and in the post-trial evaluation, cardiovascular benefits were observed in participants who had strict glucose control [9]. In contrast, in the ACCORD trial, T2DM patients with high cardiovascular risk, the intensive therapy increased mortality and did not significantly reduce major cardiovascular events after 3.5 years of follow-up [26]. Thus, T2DM patients with reduced life expectancy are less likely to derive long-term benefit from intensive glycemic control [26]. Moreover, the accumulated evidence suggests that with treatment intensification, hypoglycemia events are 2-3 times more frequent and it is associated with significant morbidity and even mortality in patients with ischemic heart disease, in aging population and hospitalized patients [27-35]. Currently, the importance of individualized glycemic goals and hypoglycemia avoidance are an essential component of diabetes management [24-25]. In particular, people living with diabetes who had suffered hypoglycemia or fragile patients with long diabetes duration and short life expectancy, a higher HbA1c level can be recommended [36].
The broad spectrum of clinical hypoglycemia in the elderly and high-complexity T2DM patients represent a challenge to the health care personnel. In patients with defective awareness of hypoglycemia the incidence of severe hypoglycemia was several fold higher than those with normal hypoglycemia awareness [37]. Further, T2DM patients with recurrent hypoglycemia events can develop RAH due to reduced hormonal and autonomic responses to subsequent hypoglycemia [27-32]. Nocturnal hypoglycemia and reduced perception of hypoglycemia may contribute to cardiovascular mortality in elderly patients [33-39].
Due to the recent deterioration in glycemic control in Costa Rica [12-14] intensification of diabetes treatment has been implemented. However, the risks of adverse events including hypoglycemia increased [18].
Our T2DM patients received an absolute or relative excess of insulin and had several risk factors for hypoglycemia events. As shown in Table 1, risk factors for hypoglycemia were: advance age, diabetes duration, the presence of cardiovascular, cerebrovascular disease, diabetes neuropathy, renal complications and a long-term insulin requirement. Of note, some of our patients who had non- severe hypoglycemia during the previous six months worseness the severity of hypoglycemia as reported before [38]. On the other hand, the potential causes of hypoglycemia were prolonged fasting, lower fasting glucose, high glucose variability, physical activity, concomitant illness, ill-timed or excessive insulin dosing and alcohol abuse [39].
In the present report we investigated the characteristics of severe hypoglycemia events in high-complexity T2DM attended in an outpatient setting. Patients had recurrent hypoglycemia events which often occurred at night. In some cases, even seizures occurred and alterations in patient´s mental state, freakish behavior, with scanty or none autonomous responses consistent with RAH were observed as depicted in figure 1. Of note, in comparison to females, severe hypoglycemia events and RAH were more commonly found in males, who were older and had longer duration of insulin treatment. They also had a higher prevalence of atherosclerosis cardiovascular disease.
Previous studies have shown that hypoglycemia associated autonomic failure represents the underlying mechanisms which occur in patients with severe and recurrent hypoglycemia [28-30]. In such events of non-symptomatic hypoglycemia, the defective contra regulatory mechanisms result in an inability to respond and recover to subsequent hypoglycemia [28-30]. As compared to type 1 diabetics, insulin treated T2DM patients have less hypoglycemia events but in long-lasting T2DM with prolonged insulin therapy the frequency and severity of hypoglycemia increases and RAH can occur [28-30], as seen in our patients.
Our intervention consisted of dietary counseling, behavioral intervention, changes in pharmacologic approach with close supervision of insulin administration. In the setting of diabetic ageing patients with cardiovascular complications and renal impairment, adjustments in insulin doses were made. This approach impacted the frequency and severity of hypoglycemia and RAH after three months treatment modification. There was an initial rise in glucose concentrations (data not shown), and at the end of the three-month period fasting glucose and HbA1c concentrations decreased in females. On the other hand, the coefficient of variation of fasting glucose declined significantly in both sexes indicating a reduction in glucose variability.
In our patients with RAH, a partial restoration of awareness of hypoglycemia took place. Interestingly, hypoglycemia symptoms occurred at higher glucose concentrations, suggesting that treatment modification helped recover the physiologic mechanisms which operate in response to declining glucose levels.
In the Hypo Compass [40-41], type 1 diabetes restored hypoglycemia awareness and prevented severe hypoglycemia events without a deterioration of glucose control. A systematic review and meta-analysis of clinical trials showed that a stepped- care approach including multiple intervention restore awareness hypoglycemia in T1DM [41]. This included structured diabetes education, individualized insulin regimens, adding behavioral therapies and diabetes technology, namely, sensors and insulin pumps. The latter is a well-known tool, which allows for better monitor complex diabetic patients [42]. Although, in our study continuous glucose monitoring system was not employed, which we recognized as an important limitation, our patients performed multiple fingerstick glucose measurements allowing us to modify diabetes treatment when necessary. Another limitation, which needs to be addressed, is the fact that we documented hypoglycemia events retrospectively. However, in previous reports the association between retrospective and prospective records of hypoglycemia symptoms was positive [22]. In addition to that, we also revised the hypoglycemia symptoms in each visit, thus we believe that our results are well founded.
In conclusion, this study reflects the seriousness of hypoglycemia in patients with a high hypoglycemia risk. Besides, highlights that hypoglycemia has deleterious consequences and hamper metabolic control. With treatment modification we were able to mitigate recurrent severe hypoglycemia and RAH through minimizing glycemic variability and improved HbA1c concentrations.
Finally, it is important to acknowledge that current pharmacologic approaches and diabetes education programs for people living with diabetes require revision in Costa Rica. Improvements in diabetes education and adherence to international guidelines are mandatory actions strongly recommended [43-44].
Acknowledgments
The authors would like to thank Dr. Berny Roldan, Lic. Daniela Rojas and Lic. Jerson Giron-Porras for their helpful comments.
This report was conducted under the regulation of the National System of Surveillance [23].
References
- Whiting DR, Guariguata L, Weil C, et al. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and Diabetes Research and Clinical Practice. 2011; 94: 311- 321.
- Diabetes and Intermediate Hyperglycemia Among Adults From the First Multinational Study of Noncommunicable Diseases in Six Central American Countries The Central America Diabetes Initiative CAMDI. Diabetes Care. 2012; 35: 738-740.
- Stamler J, Vaccaro O, Neaton JD, et al. Diabetes other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993; 16: 434-444.
- Barcelo A, Aedo C, Rajpathak S, et The cost of diabetes in Latin America and the Caribbean. Bulletin of the World Health Organization. 2003; 81: 19-27.
- Zhao Y, Shi Q, Wang Y, et Economic burden of hypoglycemia Utilization of emergency department and outpatient services in the United States 2005-2009. J Med Econ. 2016: 19: 852- 857.
- Nathan DM, Genuth S, Lachin J, et The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993; 329: 977-986.
- UK Prospective Diabetes Study UKPDS Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS 33 Lancet. 1998; 352: 837-853.
- Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin- dependent diabetes mellitus a randomized prospective 6-year Diabet Res Clin Pract. 1995; 28: 103-117.
- Holman R, Paul SK, Bethel AM, et al. Long-Term Follow up after Tight Control of Blood Pressure in Type 2 Diabetes. N Engl J Med. 2008; 359: 1565-1576.
- Diabetes Control and Complications Trial DCCT Epidemiology of Diabetes Interventions and Complications EDIC Study Research Mortality in type 1 diabetes in the DCCT EDIC versus the general population. Diabetes Care. 2016; 39: 1378-1383.
- Nathan D, Bayless M, Cleary, et al. For the DCCT EDIC Research Group. Diabetes Control and Complications Trial Epidemiology of Diabetes Interventions and Complications Study at 30 Years Advances and Contributions. Diabetes. 2013; 62: 3976-3986.
- Brenes G, Rosero Metabolic control in a nationally representative diabetic elderly sample in Costa Rica: patients at community health centers vs patients at other health care settings. BMV International Health and Human Rights. 2008; 8: 1-13.
- Lopez G, Tambascia M, Guzmán JR, et Control of type 2 diabetes mellitus among general practitioners in private practice in nine countries of Latin America. Rev Panam Salud Publica Pan Am J Public Health. 2007; 22: 12-20.
- Chen Ku CH, Gonzalez-Galvez G, Vásquez M, et Vascular complications in patients with type 2 diabetes: prevalence and comorbidities in 6 countries of Latin America A Cohort of the DISCOVER STUDY PROGRAM. Endocrine Practice. 2019; 25; 994-1002.
- Carrillo-Larco RM, Barengo NC, Albitres-Flores L, et The risk of mortality among peoples with type 2 diabetes in Latin America A systematic review and meta-analysis of population-based cohort studies. Diabetes Metab Res Rev. 2019; 35: e3139.
- Jiménez-Montero JG. Mortality rates due to diabetes mellitus in Costa Rica 2007-2017. Poster Presentations Epidemiology 2019; 68: 1616.
- Cortes-Ruiz A, Gómez Esquivel P, Molina-Granados Evaluación del control metabólico en las personas con diabetes mellitus tipo2 en Atención Primaria una mirada operativa al seguimiento de las Enfermedades Crónicas no Transmisibles. 2017. Caja Costarricense de Seguro Social Gerencia General Dirección de Compra de Servicios de Salud.
- Jiménez-Montero JG, Hernández-Saborío I, Cob-Sánchez
- Severe Hypoglycemia in an Emergency Department of a General Hospital in Costa Rica. Diabetes Complications. 2019; 3: 1-5.
- National Kidney Foundation K DOQI clinical practice guidelines for chronic kidney disease Evaluation classification and Am J Kidney Dis. 2002; 39: S1.
- Frier BM. Hypoglycaemia in diabetes mellitus epidemiology and clinical Nat Rev Endocrinol. 2014; 10: 711- 722.
- Cryer PE. Individualized Glycemic Goals and an Expanded Classification of Severe Hypoglycemia in Diabetes. Diabetes 2017; 40: 1641-164.
- Pedersen-Bjergaard U, Pramming S, Thorsteinsson B. Recall of severe hypoglycaemia and self-estimated state of awareness in type 1 Diabetes Metab Res Rev. 2003; 19: 232-240.
- Reglamento de Buenas Practicas de 2016; 39417-S.
- American Diabetes Standard of Care in Diabetes. 2020; 43: S1- S212.
- Garber AJ, Handelsman Y, Grunberger G, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm 2020 Executive Endocrine Practice. 2020; 26: 107- 129.
- Action to Control Cardiovascular Risk in Diabetes Study
- Gerstein HC et al. Effects of intensive lowering in type 2 diabetes N Engl J Med. 2008; 358: 2545-2559.
- Shorr RI, Ray WA, Daugherty JR, et al. Incidence and risks factors for serious hypoglycemia in older persons using insulin or sulphonlyureas. Arch of Intern Med. 1997; 157: 1681-1686.
- Segel SA, Paramore DS, Cryer Hypoglycemia-Associated Autonomic Failure in Advanced Type 2 Diabetes. Diabetes. 2002; 51: 724-733.
- Adler GK, Bonyhay I, Failing H, et Antecedent Hypoglycemia impairs autonomic cardiovascular function implications for rigorous glycemic control. Diabetes. 2009; 58: 360-366.
- Dunning T, vanden HeuvelI, Dickmann et al. Hypoglycemia aggravates critical illness-induced neurocognitive dysfunction. Diabetes Care. 2010; 33: 639-644.
- Garg R, Hurwitz S, Turchin A, et al. Hypoglycemia with or without insulin therapy is associated with increased mortality among hospitalized patients. Diabetes Care. 2013; 36: 1107-
- Dunning T, vandenHeuvelI, Dickmann A, et Hypoglycemia aggravates critical illness-induced neurocognitive dysfunction. Diabetes Care. 2010; 33: 639-644.
- Garg R, Hurwitz S, Turchin A, et al. Hypoglycemia, with or without insulin therapy, is associated with increased mortality among hospitalized patients. Diabetes Care. 2013; 36: 1107-
- Mahoney GK, Henk HJ, McCoy RG. Severe Hypoglycemia Attributable to Intensive Glucose-Lowering Therapy Among US Adults With Diabetes Population-Based Modeling Study 2011-2014. Mayo Clin Proc. 2019; 94: 1731-1742.
- Desouza C, Salazar H, Cheong B, et Association of hypoglycemia and cardiac ischemia: a study based on continuos monitoring. Diabetes Care. 2003; 26: 1485-1489.
- Moghissi E, Ismal-Beigi F, Cammarota Devine Hypoglycemia: minimizing its impact in type 2 diabetes. Endocr Pract. 2013; 19: 526-535.
- Schopman JE, Geddes J, Freir BM. Prevalence of impaired awareness of hypoglycemia in insulin-treated Type 2 Diabetes Research and Clinical Practice. 2010; 87: 64-68.
- Misra Hebert AD, Xinge JI, Patalone KM, et Risk predictors for severe hypoglycemia in type 2 diabetes population with previous non-severe hypoglycemia. J Diabetes Complications. 2020; 34: 1-5.
- Torimoto K, Okada Y, Hajime M, et al. Risk Factors of Hypoglycemia in Patients with Type 2 Diabetes Mellitus A Study Based on Continuous Glucose Monitoring. Diabetes Technol 2018; 20: 603-612
- Little SA, Leelarathna L, Walkinshaw E, et al. Recovery of Hypoglycemia Awareness in Long-standing Type 1 Diabetes A Multicenter Factorial Randomized Controlled Trial Comparing Insulin Pump With Multiple Daily Injections and Continuous With Conventional Glucose Self-monitoring Diabetes Care. 2014; 37: 2114-2122.
- Little SA, Speight J, Leelarathna L, et Sustained Reduction in Severe Hypoglycemia in Adults With Type 1 Diabetes Complicated by Impaired Awareness of Hypoglycemia Two- Year Follow-up in the HypoCOMPaSS Randomized Clinical Trial. Diabetes Care. 2018; 41: 1600-1607.
- Yeoh E, Choundhary P, Nwokolo M, et Interventions That Restore Awareness of Hypoglycemia in Adults with Type 1 Diabetes. A Systematic Review and Meta-analysis. Diabetes Care. 2015; 38: 1592-1609.
- Baily TS, Grunberger G, Bode BW, et American Association of Clinical Endocrinologists and American College of Endocrinology 2016 Outpatient Glucose Monitoring Conssensus Statament. Endocrine Practice. 2016; 22: 231-261.
- Mechanick JI, Harrel RM, Allende Vigo M, et AACE ACE Transculturalization Recommendations for Developing Latin American Clinical Practice Algorithms in Endocrinology- Proceedings of the 2015 Pan-American Workshop by the American Association of Clinical Endocrinologists and American College of Endocrinology. Endocrine Practice. 2016: 2: 476-501.