St-Elevation Myocardial Infarction (STEMI) Supported By National Emergency Medical Services (EMS): Prospective Study Over A 06-Month Period From January 01st To June 30th, 2023
Author(s): Papa Guirane Ndiaye1, Momar Dioum2*, Abdel Selloum2, Cheikh T Ndao3, Joseph S Mingou4,Cheikh Gaye2 and Mamadou D Beye5
1Cardiology Department, Idrissa Pouye Hospital, Senegal.
2Cardiology Department, Hospital CHNU Fann, Senegal
3Cardiology Department, Dakar Army Training Hospital,Senegal.
4Cardiology Department, Dalal Jamm Hospital, Dalal Jamm Hospital.
5National SAMU, Dakar, Senegal
*Correspondence:
Momar Dioum, Cardiology Department, Hospital CHNU Fann,Tel: 002217765518883.
Received: 05 Jun 2024; Accepted: 20 Aug 2024; Published: 29 Aug 2024
Citation: Papa Ndiaye G, Momar Dioum, Abdel Selloum, et al. St-Elevation Myocardial Infarction (STEMI) Supported By National Emergency Medical Services (EMS): Prospective Study Over A 06-Month Period From January 01st To June 30th, 2023. Cardiol Vasc Res. 2024; 8(2): 1-5.
Abstract
Introduction: ST-elevation myocardial infarction (STEMI) remains a major public health issue worldwide. The pre-hospital care by SMUR unit (medical emergency and resuscitation services) occupies an important place. The main objective of this study was to evaluate the quality of STEMI management by the Emergency Medical Services (EMS) in Senegal.
Methodology: It is a prospective, descriptive and analytical study over a period of 06 months from January 1st, 2023 to June 30th, 2023. All STEMI supported by the national EMS of Senegal were included in this study.
Results: We included 82 patients, which represented 0.01% of the EMS activity during this period. The sex ratio (M/F) was 1.9. The average age was 60 years. The interventions of the EMS in Dakar were the most important (82.3%). The most frequent mode of intervention was the search for a place and then transport (56.1%). The average number of structures contacted by the regulation in the search for a place was 2. EMS was mainly requested between 08:00 and 20:00 in 73.2% of cases. The majority of interventions (92.3%) were performed in medical facilities.
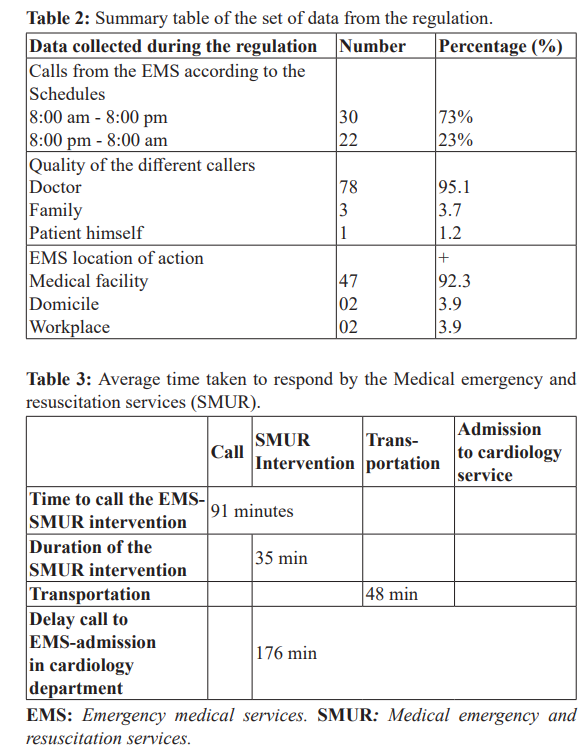
The average time between EMS call and SMUR arrival was 91 min. The average time for SMUR teams to respond was 35,2 min. The average time to transport the patient from the site of the intervention to the cardiology department was 48,8 min. The average time between emergency department call and admission to cardiology was 176 min.
Pre-hospital administration of anti-platelet therapy was effective in almost all patients (97.6%). The thrombolysis was mostly pre-hospital (31.7%) with a success rate of 57.7%. Revascularization by percutaneous coronary intervention (PCI) was performed in 40 patients (48.7%). We had noted 5 deaths at the sites.
Conclusion: The management of STEMI by the national medical service requires an improvement in deadlines to reduce morbidity and mortality
Keywords
Introduction
Coronary disease is caused by a decrease in blood flow to the coronary arteries, due to atherosclerotic lesions in most cases. The ST-elevation myocardial infarction (STEMI) is the most severe form because there is an occlusive coronary thrombosis responsible for myocardial necrosis. This disease is progressing in the world and particularly in Africa [1,2] despite important advances on the diagnostic and therapeutic levels.
Myocardial reperfusion is the cornerstone of treatment with two currently recommended strategies: intravenous thrombolysis and percutaneous coronary intervention (PCI) [3]. The speed and effectiveness of this reperfusion are the two factors that condition immediate and long-term morbidity and mortality. The whole issue is therefore to re-analyze the guilty artery and to reperfuser the myocardium that depends on it in the shortest possible time [4].
The challenge of this management is to shorten the time needed to reperfuse myocardial tissue as quickly as possible. The pre-hospital intake would play a very decisive role in the management of this sector. In order to improve the timing and quality of emergency response in Senegal, a structure called "National EMS (Emergency Medical Services)" was created. The aim of this structure is to provide a medical response adapted to any call from a person in distress or from the entourage or from a health worker. STEMI which is one of the first life-saving emergencies will naturally benefit from the largesse of this feat in emergency medicine.
The main objective of this study was to evaluate the quality of management of patients with STEMI by the National EMS. The specific objectives were to determine the prevalence of STEMI in the regulatory activity, to determine the time frame for patient care by the national EMS since the call, assess the quality of pre- hospital treatment and patient morbidity and mortality.
Methods
Our work was carried out at the National EMS with its various branches in Dakar, Saint-Louis and Diourbel-Touba, in collaboration with some public and private hospital structures. It was a multicenter, prospective, descriptive and analytical study over a period of 06 months (from January 1st, 2023 to June 30th, 2023).
All patients treated for STEMI during a procedure by the National EMS were included in this study during this period. The diagnosis of STEMI was based on clinical evidence (pain and its equivalents) and electrocardiogram (ECG) modifications with persistent ST segment elevation. Three modes of intervention were carried out by the EMS: consultation and transport, search for place and finally search for place then transport.
The following elements were analyzed:
- The epidemiological characteristics
- Characteristics of the emergency department response: origin of call, time of call, caller status, location and type of response, host structure
- The time taken in charge: the time between the call to the EMS and the arrival of the EMS on the scene of the intervention, the duration of the intervention (the time between arrival of EMS team at the intervention site and departure of the team with the patient), the duration of transport from the intervention structure to the cardiology department, the time between the call to the EMS and admission to the cardiology department,
- Cardiovascular risk factors, clinical and paraclinical data,
- Patient treatment: evaluated in the pre-hospital phases (conditioning, thrombolysis, other treatments received).
- The data and complications were also recorded.
The data were collected from the model (computer system) of the National EMS and medical records of patients in the reception structures. Data was captured with Excel software and ’analysis of data with SPSS Statistics 24 (IBM, Chicago, IL, USA), p<0.05.
Results
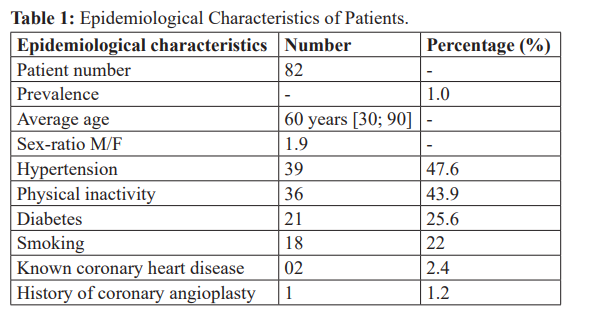
The total number of patients included in this study was 82, which represented 0.01% of the activity of the National EMS during this period. The predominance was male (65.9%) with a sex ratio (M/F) of 1.9. The average age was 60 years [30 and 90 years]. The age group between 60 and 69 years was most representative (37%). Table 1 shows the epidemiological characteristics of patients.
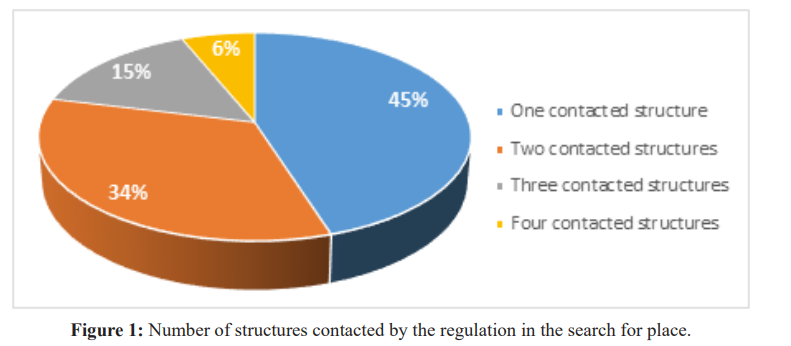
Most of the patients lived in Dakar and its suburbs (80%). The interventions of the EMS in Dakar were by far the most important (82.3%), followed by those of Saint-Louis (9%) and Diourbel- Touba (7%). The most frequent mode of intervention was search for a place and then transport (56.1%), followed by search for a place (37.8%) and consultation and then transport (6.1%). The EMS was mainly contacted by a doctor (95.1%), by the entourage (3.6%) or by the patient himself in 1% of cases. Most of the calls received by the EMS center were between 8:00 am and 8:00 pm, in 73.2% of cases. The average number of structures contacted by the regulator in the search for a place was 2 [1,4]. Figure 1 shows the number of structures contacted. The interventions were mainly performed in medical facilities (92.3%), two interventions were done respectively at home and at work. Patients were mostly treated in public hospitals (72%). Eleven (11) patients were
Hospitalized in hospitals outside of Dakar (Saint Louis and Touba). Table 2 summarizes all the data of the regulation. The average time between EMS call and SMUR arrival was 91 min [45 min and 150 min]. The average time of intervention of SMUR teams was 35.2 min [15 min and 100 min]. The average time to transport from the site of the intervention to the receiving cardiology department was 48.8 min [15 min; 200 min]. The average time between emergency department call and admission to cardiology was 176 min [100 min; 420 min]. Table 3 summarizes the different response times of the EMS.
The main cardiovascular risk factors were hypertension (47%), physical inactivity (43.9%), diabetes (25.6%) and smoking (22%). First degree coronary heredity was found in only one patient.
Chest pain was almost constant and was mostly typical in 68.3% of cases. Accompanying signs were noted such as vomiting (in 22 patients, 26.8%), dyspnea (in 14 patients, 17%). The physical examination at the entrance was without particularity with a stage KILLIP 1 in 70 patients (85%). Two patients were received at a KILLIP stage 4. The anterior territory was most affected (50%) at the electrocardiogram followed by the inferior territory (23.2%). For the treatment, the administration of the anti-platelet therapy (aspirin 300 mg and Clopidogrel 300 mg) was effective in almost all patients (80 patients, or 97.6%) pre-hospital. Regarding heparinotherapy, only low molecular weight heparin was used in 36 patients (43.7%) in pre-hospital.
The thrombolysis was performed mainly in pre-hospital (26 patients, 31.7%) with a success rate of 57.7%. Only five patients (6.1%) had a thrombolysis in hospital with a success rate of 60%. The overall success rate of thrombolysis was 58% in 31 patients who had it. Streptokinase was the only molecule used. Primary percutaneous coronary intervention (PCI) was performed in 17 patients (20%). For five patients with thrombolysis failure, a rescue angioplasty was attempted. For 18 patients (21%), PCI was scheduled during hospitalization. For thirty-seven patients (45.1%), the treatment was purely medical. The patients' development was mostly favorable. Complications were nevertheless noted: 7 cases of ventricular tachycardia, 4 cardio-respiratory arrests, 2 cases of atrio-ventricular block, 9 deaths (a mortality rate of 11%): 4 deaths occurred in hospital and 5 deaths occurred at the intervention sites [5].
Discussion
STEMI represented 0.01% of the main activity of the National EMS. This proportion seems a little underestimated in view of the evolution of this disease in recent years becoming one of the main causes of admission in cardiology. The low prevalence may also be related to the tendency of patients to see a doctor directly at the hospital. In our study, 1% of patients had contacted the EMS. An attitude that should not be encouraged knowing the importance of early pre-hospital care in prognosis.
The average age of patients was 60 and this age is relatively young as found in most African studies: Mboup [6] in Senegal, Yameogo in Burkina [7] and Khalfallah in Tunisia [8]. What has been observed in this part of the population is the high prevalence of certain cardiovascular risk factors. Hypertension was the most common risk factor in 47% of the population, as in the CORONAFRIC II study [9], which had a prevalence of 59.7%. This implies that the fight against this disease must imperatively pass through the prevention and effective control of risk factors [10]. The average time between EMS call and SMUR arrival was 91 minutes with extremes of 45 and 150 minutes (> 2 hours). Delarche found in France a delay of 25 minutes, which testifies to the effectiveness of SMUR interventions in France, which is most often done directly with the patient first for confirmation of the diagnosis and also for the regulation [11]. In Senegal, this delay is very long because of the enormous difficulties encountered in the regulation for places not available in cardiology services and sometimes also for logistical issues under emergency department (mbulances not available, team problem...).
The average time for SMUR teams was 35.2 minutes and the average time for transport was 48.8 minutes. The average time between EMS call and admission to cardiology was 181 minutes. These delays are particularly prolonged and knowing the prognostic role of the latter with their impact especially on morbidity and mortality [11,12], it is particularly important to make corrections very quickly. First, we need a national network of the activities of the EMS because the main part of these activities are in Dakar (82.3%) of cases. There is also a need for much more teams and communication about the value of using the services of the EMS, especially when it comes to acute chest pain.
Administration of the charge doses was done in 97%. Thrombolysis was performed in 31.7% with 57.7% success rate. This is in line with the recommendations that thrombolysis should be performed instead of angioplasty if the time for performing the angioplasty exceeds 120 minutes [13]. This pre-hospital thrombolysis remains a good alternative especially in our developing countries where interventional cardiology centers do not cover all regions. PCI remains the gold standard [14]. It was performed in 30% of patients, including 23% of primary PCI and 7% of rescue PCI. In Europe, according to the FAST-MI 2015 registry, primary angioplasty was performed in 76% of patients [15]. In the ACCESS study [16], 40% of patients had primary PCI. This rate was 58–64% [17] in the Euro Heart Survey (EHS-ACS-II). These better results observed in developed countries are favored by the existence of a well-organized network of treatment including the EMS, almost systematically with a larger supply of care.
These difficulties encountered in the management of these patients are not solved with a mortality rate of 11%. This rate remains high and not negligible and should encourage more to review the weak points of this care stream in order to find corrections as quickly as possible. The limitations of the study are the small sample of patients not really reflecting the epidemiology of STEMI and the collection of data with a significant risk of bias despite the fact that the study has been forward looking.
The improvement of the morbidity and mortality of acute coronary syndromes must be achieved by reducing the time taken to treat them. And to achieve this, the development of the pre- hospital sector including EMS remains an important pillar with more communication, The commission has also been working on a number of projects to raise awareness and decentralize the activities of these pre-hospital structures.
References
- Okrainec K, Banerjee DK, Eisenberg MJ. Coronary artery disease in the developing world. Am Heart J. 2004; 148: 7-15.
- Touze JE. Les maladies cardiovasculaires et la transition épidémiologique du monde tropical. Med Trop. 2007; 67: 541-542.
- Keeley EC, Hillis LD. Primary PCI for myocardial infarction with ST-segment elevation. N Engl J Med. 2007; 356: 47-54.
- Kushner FG, Hand M, Smith Jr SC, et al. 2009 Focused Updates: ACC/AHA Guidelines for the management of patients with ST Elevation myocardial infarction (Updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (Updating the 2005 Guideline and 2007 Focused Update): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009; 54: 2205-2241.
- Steg PG, Dabbous OH, Feldman LJ, et al. Global Registry of Acute Coronary Events Investigators. Determinants and prognostic impact of heart failure complicating acute coronary syndromes: observations from the Global Registry of Acute Coronary Events (GRACE). Circulation. 2004; 109: 494-499.
- Mboup MC, Diao M, Dia K, et al. Acute coronary syndromes in Dakar: therapeutic, clinical and evolutionary aspects. Pan Afr Med J. 2014; 19: 126.
- Yaméogo NV, Samadoulougou A, Millogo G, et al. Délais de prise en charge des syndromes coronariens aigus avec sus- décalage du segment ST à Ouagadougou et facteurs associés à un allongement de ces délais: à propos de 43 cas colligés au CHU Yalgado Ouédraogo. Pan Afr Med J. 2012; 13: 90.
- Khalfallah AB, Sanaa I, Annabi N, et al. Valeur prédictive des marqueurs de l'inflammation au cours des syndromes coronaires aigus. Arch Mal Coeur Vaiss. 2005; 98: 899-905.
- Ba SA. Epidémiologie de la coronaropathie en Afrique.Congrès. APPAC. 2016; 8-10.
- Delarche M. Évaluation de la prise en charge pré hospitalière et hospitalière des SCA ST+ de moins de douze heures sur le CHG de Libourne, entre 2008 et 2012. Médecine humaine et pathologie. 2017.
- Nallamothu. Acute myocardial infarction and congestive heart failure outcomes at specialty cardiac hospitals. Circulation. 2007; 116: 2280-2287.
- Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and doorto-balloon-time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000; 283: 2941-2947.
- Borja Ibanez, Stefan James, Stefan Agewall, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39: 119-177.
- Puymirat E, Ducrocq G. Comparison between European Society of Cardiology (ESC) and American College of Cardiology/American Heart Association (ACC/AHA) guidelines for initial management of ST-elevation myocardial infarction (STEMI). Ann Cardiol Angeiol (Paris). 2013; 62: 265-268.
- Loïc Belle, Guillaume Cayla, Yves Cottin, et al. French Registry on Acute ST-elevation and non-ST-elevation Myocardial Infarction 2015 (FAST-MI 2015). Design and baseline data. Arch Cardiovasc Dis. 2017; 110: 366-378.
- Schamroth C, investigators ASA. Management of acute coronary syndrome in South Africa: insights from the ACCESS (Acute Coronary Events-a Multinational Survey of Current Management Strategies) registry. Cardiovasc J Afr. 2012; 23: 365-370.
- Lori Mandelzweig, Alex Battler, Valentina Boyko, et al. The second Euro Heart Survey on acute coronary syndromes: Characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006; 27: 2285-2293.