Stroke Subtypes, Risk Factors and Treatment Outcomes at A Tertiary Hospital Situated in Rural Southwestern Nigeria: A Five- Year Restrospective Observational Study
Author'(s): Azeez Oyemomi IBRAHIM, MBCHB, FMC-FM1, Paul OLOWOYO, MBBS, FWACP2, Adewumi Oluwaserimi Ajetunmobi, MBBS, FWACP3, Abayomi AYODAPO, MBChB, FMCFM4 , Waheed Olalekan ISMAIL, MB.CH.B, FWACP5, and Gbadebo Oladimeji AJANI, MB.CH.B, FWACP6
1Family Medicine Department, Federal Teaching Hospital, IdoEkiti, Ekiti State, Nigeria. Orcids No: 0000-0002-2395-9551.
2Department of Medicine, College of Medicine and Health Sciences, Afe Babalola University, Ado-Ekiti, Ekiti State, Nigeria, Orcid No: 0000000208028505
3Federal Teaching Hospital, Ido Ekiti, Ekiti State, Nigeria, Orcid no: 0000000154839328
4Department of Family Medicine, University College Hospital, Ibadan. Nigeria, Orcid No: 0000000242857622.
5Waheed Olalekan ISMAIL (MB.CH.B, FWACP), Department of Family Medicine, Obafemi Awolowo University, Ile- Ife, Osun State, Nigeria.
6Department of Medicine, College of Medicine and Health Sciences, Afe Babalola University, Ado-Ekiti, Ekiti State, Nigeria, Orcid No: 0000000275517835.
*Correspondence:
Azeez Oyemomi, IBRAHIM (MBCHB, FMC-FM), Family Medicine Department, Federal Teaching Hospital, Ido-Ekiti, Ekiti State, Nigeria, Orcid no: 0000-0002-2395-9551.
Received: 14 October 2021; Accepted: 10 November 2021
Citation: Ibrahim AO, Olowoyo P, Ajetunmobi AO, et al. Stroke Subtypes, Risk Factors and Treatment Outcomes at A Tertiary Hospital Situated in Rural Southwestern Nigeria: A Five- Year Restrospective Observational Study. Cardiol Vasc Res. 2021; 5(6): 1-8.
Abstract
Introduction: Despite the high burden of stroke globally, there is an observed paucity of data regarding its subtypes, risk factors and treatment outcomes in rural Southwestern Nigeria. The study ascertained the subtypes, risk factors and treatment outcomes of stroke at the adult Accident and Emergency Department of a tertiary hospital in a rural Southwestern Nigeria.
Materials and methods: A retrospective survey using data form and standardized questionnaire was used to review the patients admitted for stroke between January 2015 and December 2019. The data were analyzed using SPSS Version 22.0. The results were presented in descriptive and tabular formats.
Results: In this study, 276 stroke patients comprised Ischemic (60.1%) vs Hemorrhagic (39.9%) strokes were studied. The mean age of the patients was 67.3±11.1 years. The majority were males and were older than 65 years. The independent predictors of stroke admissions were Informal education [(AOR = 0.288; 95% CI: (0.120-0.691), p = 0.005)], low income earners [(AOR = 0.452; 95% CI: (0.230-0.888), p = 0.021)], obesity [(AOR = 0.080; 95% CI: (0.019-0.347), p= 0.001)], heart failure [(AOR= 9.152; 95% CI: (2.325-41.266), p < 0.001)], atrial fibrillation [(AOR = 0.136; 95% CI: (0.068-0.891),p = 0.001)], tobacco smoking [(AOR = 0.350; 95% CI: (0.137-0.891), p = 0.028)], and poorly controlled blood pressure [(AOR = 0.107; 95% CI: (0.033-0.348), p <0.001)]. The mortality rate was 10.1%.
Conclusion: The results of this study further support the argument on the higher prevalence of stroke admission in rural areas of Southwestern Nigeria. There may be need for public awareness on primary stroke prevention and early identification of the risk factors in order to reduce the prevalence and mortality of stroke in the rural Southwestern Nigeria.
Keywords
Introduction
Stroke is defined as rapidly developing clinical signs of focal or global disturbance of cerebral function, with symptoms lasting more than 24 hours, leading to death, with no apparent cause other than a pathological process of blood vessel [1]. Stroke is one of the common causes of morbidity and mortality worldwide, affecting both male and female subjects, prompting research into this challenge [2]. The World Health Organization estimates that by 2030, about 80% of strokes will occur in people living in developing countries of the world [3]. In Nigeria, stroke is a major cause of neurological admissions and its incidence is expected to increase in future as the population undergoes a health transition from communicable to non-communicable related diseases [4]. This observation is due to rising adoption of western life styles and dietary changes by people of low- and middle- income countries (LMICs) including Nigeria [4,5].
The current prevalence of stroke in Nigeria is 1.14 per 1000 populations while the 30-day case fatality is as high as 40% [6]. In a Nigeria hospital, stroke accounted for 3.7% of emergency admissions and 8.7% of medical admissions [7]. Stroke is broadly classified into Ischemic and Hemorrhagic [8]. In most of the studies conducted in Africa, the prevalence of Ischemic Stroke is relatively higher than Hemorrhagic stroke [9]. In a study in South-East Nigeria, 65% had Ischemic stroke while 35% had Hemorrhagic stroke, with intra cerebral hemorrhage accounting for 31% and subarachnoid hemorrhage accounting for 4% [10].
There have been variations in the prevalence of major risk factors among the stroke subtypes due to differences in race, genetic and environmental factors, demonstrating that knowledge of patho- physiology is crucial to the care and outcome of stroke patients [11]. Previous studies have established that the risk factors for stroke are multi-factorial [7,10]. However, more than 80% of published reports in Sub-Sahara Africa (SSA) have identified hypertension as the most common co-morbid ailment associated with stroke [7,12]. Other studies found diabetes mellitus, obesity, dyslipidemia, heart failure and atrial fibrillation as important co- morbid ailments linked with the development of stroke [13,14]. Unhealthy lifestyles such as tobacco smoking, alcohol abuse and sedentary life have also been documented in the literatures as risk factors for stroke [7,13,14]. In addition, age, sex and family history are non modifiable risk factors linked with the development of stroke in several studies [14,15]. In LMICs of Africa, majority of the people lives in rural areas where awareness about risk factors for stroke is poor due to high level of poverty, illiteracy and non accessibility to quality health care [7,16]. Most of the data that were used in the prevention and management of stroke were from studies carried out in developed countries [8,17]. Few related studies in Africa were conducted in hospitals located in urban centers, and obviously, left out the rural areas where majority of the population resides. Hence, this study would generate evidence based data for improving the prevention strategy of stroke and contribute to better management of stroke in rural setting. The objectives of this study were to ascertain the risk factors and treatment outcomes of stroke admissions at a tertiary hospital in rural southwestern Nigeria.
Materials and Methods
Study setting
The study was carried out at the adult Accident and Emergency Department (AED) of the Federal Teaching Hospital, Ido-Ekiti (FETHI). Ido Ekiti is located in one of the rural communities of Ekiti State, Southwestern Nigeria. It has a total land area of 332km2, and as at last population census of 2006, it had a total population of 159,114. It also has an annual growth rate of 3.2%, with a projected population (by 2019) of 225,305 [18]. The people are mainly farmers and traders in the informal sector with a relatively small portion of the working population and retirees in the formal sector. FETHI is the main public referral hospital in the State and has 180 beds. The AED of the hospital has 14 male and 10 female beds with an average of 200 new admissions per month. Many of the patients including patients with stroke were either referred from nearby private and government owned health facilities or brought in by relations without prior appointment. In FETHI during the study period, the department of medicine had 12 Consultant specialists, including a Consultant Neurologist, who is the head of the team responsible for the management of stroke patients at AED.
Study design
This was a descriptive, retrospective review of hospital records of stroke admissions at adult AED between 1st January 2015 and 31st, December 2019.
Study population
This included all stroke patients who were registered and admitted at adult AED between 2015 and 2019.
Sample size
A total of 276 patients with stroke whose medical records were complete and diagnoses confirmed by the Computed Tomography (CT) imaging were purposively selected for this study. This was derived from the total number of 341 patients admitted for stroke. Among these admissions, three hundred and nine (309) were confirmed by Computed Tomography (CT) imaging to have suffered as stroke. Of these admissions, only 276 patients who had complete medical records were used for this study.
Inclusion criteria
Stroke patients who were confirmed by CT imaging as per WHO Criteria for diagnosis of stroke during the period under review.
Exclusion criteria
Stroke patients whose data were incomplete, not available or whose initial diagnosis of stroke was later changed to other cause (rule out stroke).
Data collection instruments and method
The researchers of this study designed and developed the instruments for data collection, which were data form and standardized questionnaire containing the variables to be measured based on the previous literature from the WHO step wise approach to stroke surveillance [19]. The case records of each stroke patient and admissions and discharge from the Nursing Report Books were manually retrieved and inputted into the data form. Information retrieved included the date and year of admission, socio- demographic profile, types of stroke (judged by the final assessment of the Consultant Neurologist using the report of imaging (CT scan) in line with WHO Criteria). The risk factors related to stroke were systematically extracted from the patient’s records: hypertension, diabetes mellitus, dyslipidemia, obesity, history of alcohol intake, tobacco smoking and cardiac disease were recorded. The electrocardiogram (ECG) report of atrial fibrillation was also recorded. Admission blood pressure, random plasma glucose and body mass index were also extracted and recorded. The treatment outcomes as retrieved were to show if the patient was discharged home, discharged against medical advice (DAMA), referred to other facility or died. The data were collected by two trained casualty officers and nurses and supported by one resident doctor from stroke unit and were cross-checked by the principal investigator.
Data entry and analysis
All data collected were checked for completeness and entered into Epi info Version 7, and were later exported to SPSS version 22.0 for analysis. Continuous variables were expressed as Mean standard deviation, while categorical variables as frequencies and percentages. The relationship between various socio-demographic profile and stroke subtype was analyzed with cross tabulation and Chi-square Student’s t-test analysis was used to determine the association between numeric variables and stroke. The Univariate regression analysis was done to identify the risk factors associated with stroke. This was followed by an unconditional multivariate logistic regression model to determine the independent predictors of stroke admissions. Unadjusted and adjusted odds ratio (AOR) were developed with the corresponding 95% CI and p < 0.05 was considered statistically significant.
Ethical Clearance and Consideration:
The Institution’s Ethics and Research Committee (ERC) gave approval for the study ( ERC/2020/08/25/402A). Information obtained for each patient was kept anonymous and confidential. Only the principal investigator had access to the data.
Results
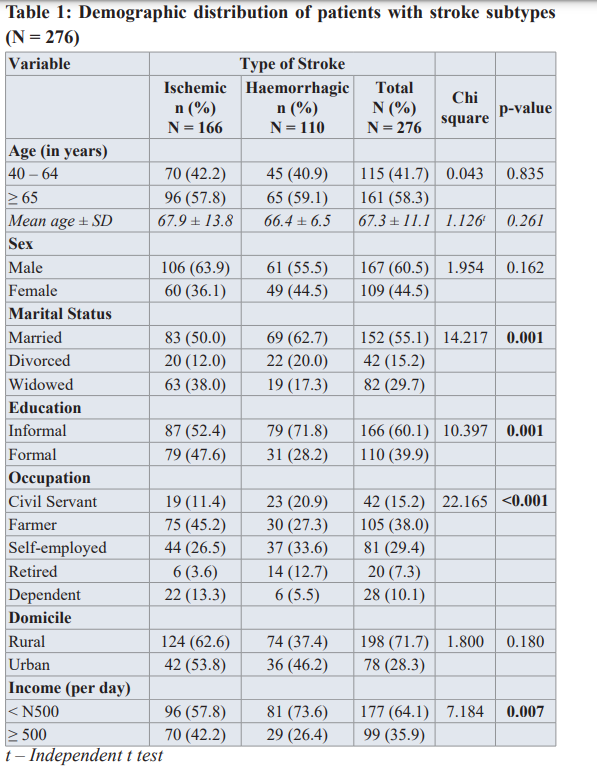
There were 5944 admissions at the adult Accident and Emergency Department of the FETHI during the study period (Medical admissions 3511 (59.1%) vs surgical admissions 2433 (40.9%). Among the medical admissions, 309 (8.8%) were confirmed by CT imaging as stroke patients. Of these admissions, the medical records of only 276 (89.3%) stroke patients were retrieved from records office and were included in the study. The medical records of the remaining 33 (10.7%) stroke patients were not analyzed since they had incomplete data. The mean age of the patients was 67.3 ± 11.1 (ranged 40-92) and 161(58.3%) were older than 65 years. The majority were males 167(60.5%), married 152 (55.1%) and had no formal education 166 (60.1%). Over one -third, 105 (38.0%) were farmers. The majority were rural dwellers 198 (71.7%) and low income earners 177 (64.1%). There was a statistically significant difference between the stroke subtypes and marital status (p=0.001), education (p=0.001), occupation (p<0.001) and income (p=0.007) (Table 1).
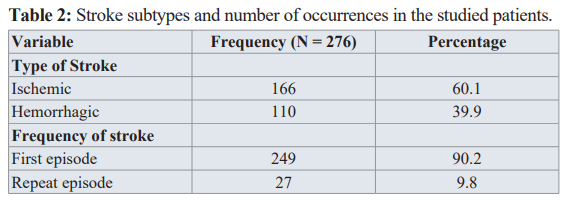
In this study, there were 166 (60.1%) patients diagnosed as Ischemic stroke (IS) and 110 (39.9%) as Hemorrhagic stroke (HS). The majority, 249 (90.2) presented with first episode of stroke (Table 2).
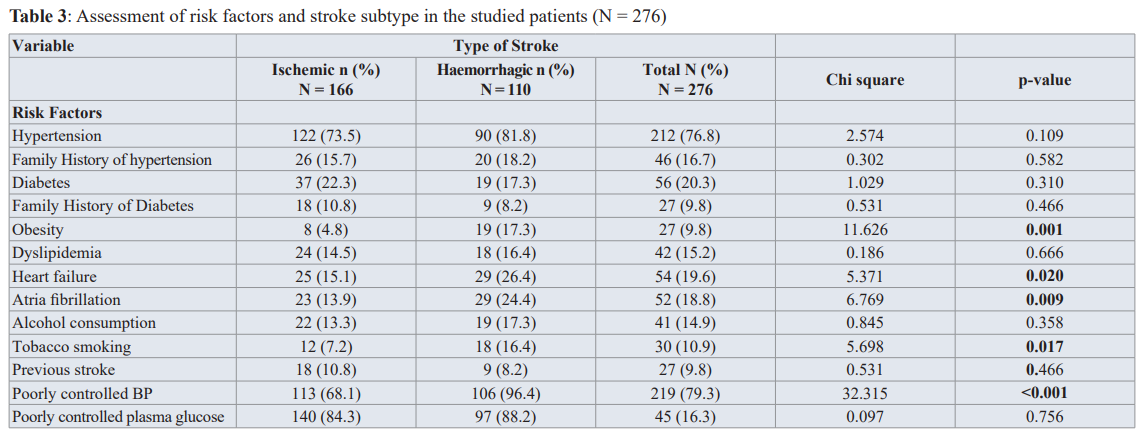
The most common identified risk factors in all the stroke patients was hypertension 212 (76.8%). This was followed by diabetes, 56 (20.3%), heart failure, 54(19.6%) and atrial fibrillation, 52 (18.8%). The majority 219 (79.3) had uncontrolled blood pressure at admission. There was a statistically significant difference between the stroke subtypes and obesity (p =0.001), heart failure (p = 0.020), atrial fibrillation (p = 0.009), tobacco smoking (p = 0.017) and poorly controlled blood pressure (p< 0.001) (Table 3).
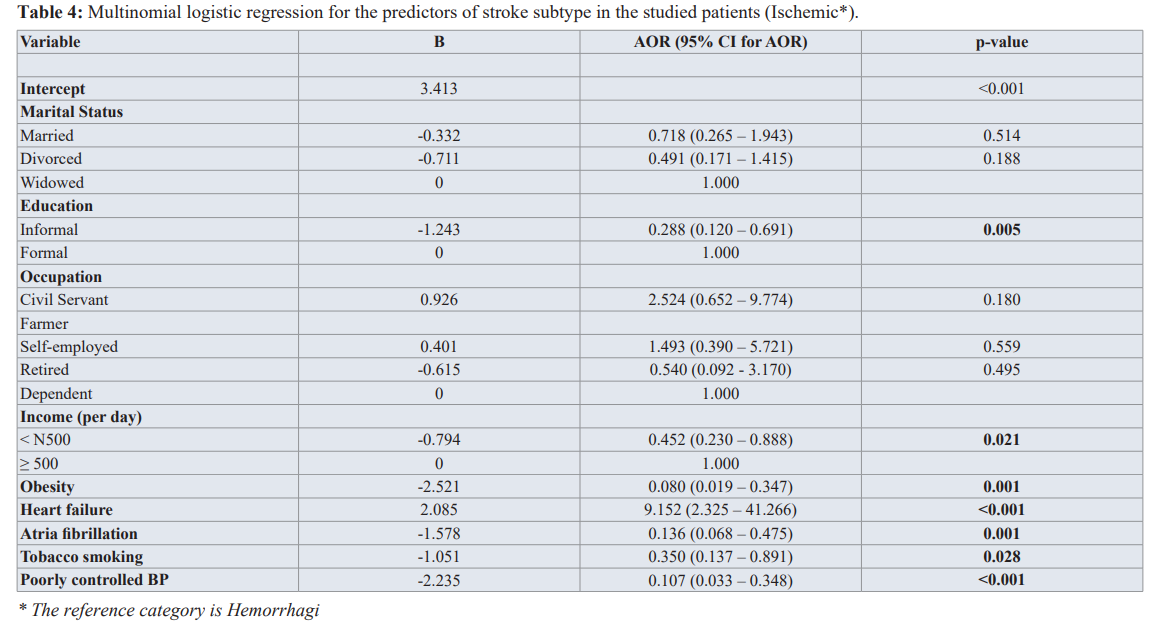
Stroke patients with the above risk factors were subsequently subjected to multivariate logistic regression modeling to identify the independent predictors of stroke admissions. The analysis revealed that Informal education [(AOR = 0.288; 95% CI: (0.120- 0.691), p = 0.005)], low income earners [(AOR = 0.452; 95% CI: (0.230-0.888), p = 0.021)], obesity [(AOR = 0.080; 95% CI: (0.019-0.347), p= 0.001)], heart failure [(AOR= 9.152; 95% CI: (2.325-41.266), p < 0.001)], atrial fibrillation [(AOR = -0.891),p = 0.001)], tobacco smoking [(AOR = 0.350; 95% CI: (0.137-0.891), p = 0.028)], and poorly controlled BP [(AOR = 0.107; 95% CI: (0.033-0.348), p <0.001)] were the independent predictors of stroke subtypes admission (Table 4).
The treatment outcomes showed that 28 (10.1%) died on admission. There were more deaths 20 (18.2%) in Hemorrhagic than 8 (4.8%)

Ischemic strokes. There was a statistically significant difference between the stroke subtypes and the treatment outcomes (p < 0.001), Table 5.0
Discussion
This retrospective survey shows that stroke accounted for 8.8% of medical and 5.2% of adult hospital emergency admissions respectively. This finding is similar to 8.7% medical admissions found by Ogun et al. [20] and 11.6% found by Eze et al. [10]. This is due to similarity in the setting and study design. This further strengthens the argument of higher prevalence of stroke in rural Southwestern Nigeria. However, it was higher than 5% found by Walker et al. [21], but lower when compared with finding by Danesi et al. [5]. The differences could be due to variation in the prevalence of major risk factors for stroke due to differences in race, genetic and environmental factors.
In this study, the mean age of the patients was 67.3 ± 11.1 years. This is in line with other studies in developing countries where the mean age of stroke patients was at the 6th or 7th decade [7,10]. The risk factors for stroke are most prevalent in the above age range. However, our mean age was higher than the reported mean age in other studies [14,22]. The difference may be due to hospital based setting, selection bias and poor risk factors control. Thus, community based studies are required to clarify and compare the incidence as well as prevalence of stroke by age in our area. The higher percentage of stroke in male over female patients in this study is consistent with other previous studies [6,7,10,13- 14]. These studies have attributed the male preponderance to the high incidence of alcohol abuse and tobacco smoking which have been identified as a significant risk factors for stroke in males than females [10,14]. Other studies have also identified vascular protection of endogenous estrogen which were absent in males as the reason for high occurrence of stroke in males [7,10,13]. However, there is no significant sex predilection to a particular stroke subtype and this is consistent with finding by Feigin et al. [8]. In this study, the majority of our patients were farmers and predominantly with informal education. This is consistent with other studies [7,14]. Lack of information and ignorance of the risk factors among these set of patients might be responsible for this observation. Our study also showed that the majority of our patients were rural dwellers and is consistent with similar finding in LMICs [23], but opposite to finding by Fekadu et al, where the majority were urban dwellers [14]. The location and catchment area of the study centre determine the kinds of patients visiting the hospital. The high burden of stroke in the rural area may be due to ignorance, poor control of risk factors and poor access to quality health care services. The increased proportion of patients with low income earners in this study is a reflection of the general trend in rural Nigeria where the majority of the rural dwellers are poor. However, this should be interpreted with caution because of the skewed distribution of socioeconomic status in Nigeria.
In this study, we found Ischaemic stroke (IS) to be the most common type of stroke among our patients. This is consistent with several other studies in Africa [10,13,14]. This may be due to similarity in race and genetic composition. IS was said to be higher in Africa and Europe compared to Asia [24]. Contrary to this finding, other studies found haemorrhagic stroke as the most common form of stroke [10,13,14]. This may be due to difference in age distribution of the population, study setting, admission policy and risk factors between different populations. In this study, a repeat stroke (9.8%) is higher when compared to reports of other studies [22,25]. The difference may be due to difference in stroke awareness, poorly control of vascular risk factors and access to quality health care among the previously diagnosed first ever stroke patients [13]. The reason for high rate of repeat stroke in our study may be due to multi factorial risk factors and co-existing potential causes of stroke [26]. Hypertension was identified as the most common risk factor in this study and is consistent with other African studies where hypertension was documented to account for between 82.5- 91.7% risk factors [12,13,22]. This may reflect the poor community awareness and poor health seeking behavious, an indication that hypertension is under diagnosed and less treated in the community. This finding calls for public awareness to address the risk factors for hypertension in order to reduce the trend of stroke among the study population. Diabetes mellitus (DM) is another risk factor for stroke in this study. Diabetes (DM) was diagnosed as comorbidity in 20.3% of our patients. The prevalence of DM was closely similar to 19.5% found by Owolabi et al. [27] due to similarity in the study design and socio-demographic factors [25]. However, it was lower when compared to 26.3% found by Walker et al. [21] and 46.8% by de Carvalho et al. [28] but was higher when compared with 10.1% by Watila et al. [29] and 7.8% by Deresse et al. [12]. The difference could be due to the setting, referral bias and single hospital based design of our study. Future research on multi-centered studies is recommended to ascertain the risk of diabetes in Nigeria stroke patients. Diabetes is a major risk factor for the development of atherosclerosis and the excess risk of stroke in patient with DM is about four times higher when compared with normal individuals in a general population [7,13,14]. Therefore, strategy for good glycemic control in DM patients is advocated to prevent the development of stroke. Atrial fibrillation (AF) and heart failure were commonly associated with the development of stroke in our study and is consistent with finding by previous study [14]. The proportion of patients with AF in of our study is higher than 6.1% found by Russell et al. [13] and 3.7% by Lekoubou et al. [30]. The higher AF in our study may be due to the availability of ECG scan at the time of admissions. Unlimited access to ECG was also reported by Fekadu et al. [14], unlike other studies [13,30]. Obesity is a risk factor for stroke in our study and is consistent with other studies [25,31]. However, our proportion of patients with obesity was lower when compared with 18.0% by Obiako et al. [25] and 60.8% by Ekeh et al. [31]. This may be due to the lifestyles of our patients as the majority were rural dwellers and farmers. Tobacco smoking is identified as a risk factor in our study and is consistent with 11.3% found by another study in Nigeria [21]. However, it was higher than 6% found in Saudi Arabia [32] but less than 50% found by Fekadu et al. [14]. The difference may be due to abuse of social drug and the implementation of anti- smoking law by the respective countries. Coexistence of poorly controlled blood pressure and plasma glucose in this study are risk factors for stroke among our patients. Findings from several other studies have shown that stroke increases as mean systolic and diastolic blood pressure increase and that lowering of B.P could prevent the risk of stroke by 70% [7,23]. Poorly controlled plasma glucose in this study suggests a possible combination of reactive hyperglycemic due to a major stress response and pre-existing DM [25,33]. Factors contributing to poor glycemic control in stroke patients are multi factorials [25,33]. Recognition of these factors will enhance good glycemic control and a further reduction in the risk of stroke.
In this study, the independent predictors of stroke were informal education, low-income earners, obesity, heart failure, atrial fibrillation, tobacco smoking and poorly controlled blood pressure. Informal education is linked with increased risk of stroke in this study. This may be due to lack of information, ignorance of the risk factors and inability to manage such risk factors among these set of patients. Even, when they are aware of the risk factors and its intervention, they failed to adhere and follow it properly [7,14]. The low-income earners are linked with risk of stroke due to poor health seeking behavious. Some patients with modifiable risk factors like hypertension and diabetes lack the needed funds to purchase their medications and therefore not compliant [31]. Obesity is this study is linked with stroke. Previous study has established the association between obesity and increased risk of stroke to insulin resistance, pro-thrombotic state, excessive secretion of free fatty acids and activation of sympathetic nervous system and these may result in catabolic imbalance [14]. Besides, sedentary life style in obese patients can affect the post stroke recovery and outcomes and may lead to repeat stroke that may have been observed among our patients [14]. Atrial fibrillation, which is a predictor of stroke in this study, is consistent with other studies and may be due to the occlusion of cerebral arteries [13,14]. Also, tobacco smoking is a predictor of stroke in this study and is consistent with other studies [7,14,21]. Smoking predisposes blood vessels to thrombosis and facilitates platelet aggregation, probably by causing an imbalance between brain vascular coagulation and abnormal fibrinolysis [14]. This may lead to alteration of the function of blood brain barrier and endothelial cell function [14]. Therefore, strategies for stopping smoking in the study area and elsewhere in the country should be implemented. Poorly controlled blood pressure (B.P) in this study is an independent predictor of stroke and may be related to poor adherence and lack of frequent monitoring of their B.P. Adherence to treatment of hypertension requires understanding of the problem, funds to purchase medications and regular follow up clinic appointment. This is a great challenge to sustain among these set of patients who were mainly of low-income earners. Also, uncomplicated hypertension is usually asymptomatic and denial of the disease is common [14]. A rise of 10mmHg in the mean arterial pressure leads to about 20-30% increase in stroke risk [7,14,21]. Therefore, management of hypertension and strategies for the control of the risk factors for hypertension are recommended.
The outcomes of admissions in this study appear to be good with respect to the number of patients that were successfully treated and discharged or referred to other facilities. The availability of CT scan imaging and ECG for all our patients among other factors may be responsible for these outcomes. However, the high number of patients that were DAMA was a source of concern. Some DAMA patients lacked the funds to pay for the services required. Some patients lose all hope, especially when recovery was slow, and prefer to die at home or obtain treatment from alternative medical practitioners. DAMA most often, were observed to be due to wrong cultural or religious beliefs or attributing the cause of illness to spiritual attacks. Therefore, effective and sustained health education and communication strategies are needed to improve in the area of early presentation and access to quality health care services. Continuing enrolment of citizens on National Health Insurance Scheme (NHIS) should be intensified to reduce the incidence of DAMAs due to financial constraint in our hospitals.
In this study, the pattern of mortality agrees with the pattern observed in the aggregated data from WHO study [34]. The percentage mortality reported in relation to the total emergency admissions may appear small but when viewed along the line of total emergency medical admissions, the burden of stroke mortality becomes more significant. Our study showed that mortality for HS was significantly higher than IS stroke and is consistent with other studies reported in Africa [9,12,13]. Stroke mortality varied across several Africa studies reflecting the differences in access to quality health care services, absence of qualified personnel, poor state of ICU, lack of diagnostic equipment, inappropriate treatment and lack of dedicated stroke unit [9]. Considering the fact that knowledge and perception of stroke mortality are low in rural community, strategies for primary stroke prevention and early recognition of the risk factors for stroke may be needed in order to reduce the prevalence and mortality of stroke in the rural setting.
Strength and Limitation
Despite the fact that the study centre is a rural community, availability of CT imaging and ECG by the patients validates the study. As part of the limitations, the study is a retrospective, single center hospital-based with a small sample size. Hence, it may be subjected to referral bias and might not reflect the true prevalence of stroke admission in the community. Lack of postmortem on the possible cause of death is also a limitation.
Conclusion
In this study, 276 stroke patients comprised Ischemic (60.1%) vs Hemorrhagic (39.9%) strokes were studied. The independent predictors of stroke admissions were informal education, low- income earners, obesity, heart failure, atrial fibrillation, tobacco smoking and poorly controlled BP. The mortality rate was 10.1%. The results of this study further strengthening the arguments on high prevalence of stroke admissions in rural Southwestern Nigeria. Therefore, there may be need for public awareness on primary stroke prevention and early identification of the stroke risk factors to reduce stroke prevalence and mortality in rural Southwestern Nigeria.
Acknowledgement
Appreciation goes to the casualty officers and nurses at accident and emergency department. The authors also thank staff of the records department for supplying the needed information in their archives.
References
- Mensah GA, Nurrving B, Feigin VE. The global burden of Neuro-epidemiology. 2015; 45: 143-145.
- Mackay J, Mensah The atlas of Heart Disease and stroke. World Health Organization (WHO), Geneva, Switzerland. 2004.
- Mathers CD, Loncar Updated projections of global mortality and burden of disease,2002-2030: data sources, methods and results. Evidence and information for policy working paper. Geneva: World Health Organization. Plos Med. 2006: 3: e442.
- Osuntokun BO. Stroke in Africans. Afri J Med Sci. 1997; 6: 39-55.
- Danesi MA, Oyesola JA, Onitiri AC. Risk factors associated with cerebrovascular accident in Nigeria. East Afri Med J. 1983; 60: 190-195.
- Owolabi MO, Akarolo- Anthony S, Akinyemi R, et al. The burden of stroke in Africa: a glance at the present and a glimpse into the Cardiovasc J Afr. 2015; 26: 26-38.
- Desalu OO, Wahab KW, Fawale B, et al. A review of stroke admissions at a tertiary hospital in rural Southwestern Ann Afr Med. 2011; 10: 80-85.
- Feigin VL, Forouzanfar MH, Krishnamurthi R. Global and regional burden of stroke during 1990-2010: Findings from the Global burden of Disease Study 2010. The Lancet. 2014; 383: 245-255.
- Lisk DR, Ngobeh F, Kumar B, et Stroke in Sierra Leonean Africans; perspectives from a private health facility. West Afr Med J. 2020; 37: 420-424.
- Eze CO, Agu CE, Kalu UA, et The pattern and presentation of Stroke in Federal Teaching Hospital Abakaliki, South-East Nigeria. Journal of Biology Agriculture and Health care. 2013; 3: 141-144.
- Al-Hashel JY, Al-Sabah AA, Ahmed SF, et al. Risk factors, subtypes and outcome of Ishemic Stroke in Kuwait: a National J Stroke Cerebrovasc Dis. 2016; 25: 2145-2152.
- Deresse B, Shaweno Epidemiology and in-hospital outcome of stroke in South Ethiopia. J Neurol Sci. 2015; 355: 138-142.
- Russell James BW, Charles E, Conteh V, et al. Risk factors, clinical outcomes and predictors of stroke mortality in Sierra Leoneans: A retrospective hospital cohort study. Ann Med 2020; 60: 293-300.
- Fekadu G, Chelkeba L, Kebede Risk factors, clinical presentations and predictors of stroke among adult patients admitted to stroke unit of Jimma University medical center, south west Ethiopia: prospective observational study. BMC Neurology. 2019; 19: 187.
- Boehme AK, Esenwa C, Elkind MSV. Stroke risk factors, genetic and prevention. Circ Res. 2017; 120: 234-239.
- Ogun SA, Oluwole O, Fatade B, et Comparison of the Siriraj stroke score and the WHO criteria in the clinical classification of stroke subtypes. Afr J Med Sci. 2002; 31: 13-16.
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke Statistic-2016 update: a report from the America Heart Circulation. 2016; 133: e38-360.
- slideshare.net/EkitiState
- World Health The WHO step wise approach to stroke surveillance; Geneva 2006. Available at http:// www,who,int/chp/steps/stroke/en/accessed Feb 12 2021.
- Ogun Acute Stroke Mortality at Lagos University Teaching Hospital-A five-year review. Nig Q J Hosp Med. 2000; 10: 8-10.
- Walker RW, Rolfe M, Kelly PJ, et al. Mortality and recovery after stroke in Stroke. 2003; 34: 1604-1609.
- Fekadu G, Wakassa H, Tekle F. Stroke Event factors among adult patients admitted to stroke unit of Jimma University medical center: Prospective Observational Stroke Research and Treatment. 2019; 4650104.
- Njoku CH, Aduloju AB. Stroke in Sokoto, Nigeria: A Five year retrospective Ann Afr Med. 2004; 3: 73-76.
- Poungverin N, Viriyavejaku A, Kpmontric CS. Stroke score validation study to distinguish supratentorial intracerebral haemorrhage from infarction. Br Med J. 1991; 302: 1563-
- Obiako OR, Oparah SK, Ogunniyi A. Prognosis and outcome of acute stroke in the University College hospital, Ibadan, Nigeria Journal of Clinical Practice. 2011; 14: 359-362.
- Yamamoto H, Bogousslavsky J. Mechanism of second and further strokes. J Neurology, Neurosurgery and Psychiatry. 1998; 64: 771-776.
- Owolabi MO, Agunloye AM. Which risk factors are more associated with Ischemic rather than Hemorrhagic stroke in black Africans?. Clin Neurol Neurosurg. 2013; 115: 2069-
- De Carvalho JJF, Alves MB, Viana GAA, et Stroke epidemiology, patterns of management, and outcomes in Fortaleza, Brazil: a hospital based multicenter prospective study. Stroke. 2011; 42: 3341-3346.
- Watila MM, Nyandaiti YW, Ibrahim A, et al. Risk factor profile among black stroke patients in Northeastern Nigeria. Neurosci Biobehav 2012; 4: 50-58.
- Lekoubou A, Nkoke C, Dzudie A, et al. Recurrent stroke and early mortality in an urban medical unit in J Stroke Cerebrovasc Dis. 2017; 26: 1689-1694.
- Ekeh BC, Ogunniyi AO, Isamade Stroke risk factors among patients in a Nigeria Teaching Hospital. J Med Trop. 2013; 15: 74-79.
- Rajeh S, Awada A, Niazi G, et al. Stroke in a Saudi Arabian National Guard Community Analysis of 500 Consecutive Cases from a population- Based Stroke 1993; 24: 1635-1639.
- Capes SE, Hunt D, Maimberg K, et al. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic A systematic overview. Stroke. 2001: 32: 2426-2432.
- World Health The WHO step wise approach to stroke surveillance; Geneva. 2006. Available at http:// www,who,int/chp/steps/stroke/en/accessed Feb 12 2021.