Subclinical Hypothyroidism in Type 2 Diabetes Mellitus Patients Attending In a Tertiary Care Hospital in Bangladesh
Author'(s): Mohammad Afjal Hossain1, Atiquzzaman2, Mohammed Shafiqul Islam Bhuiyan3, Mohammad Saifuddin4, Farzana Amin5, Md. Musab Khalil6, Md. Lutful Kabir7 and Mirza Sharifuzzaman4
1Assistant Professor, Department of Endocrinology, US- Bangla Medical College, Narayanganj, Bangladesh.
2Assistant Professor, Department of Medicine, US- Bangla Medical College, Narayanganj, Bangladesh.
3Associate Professor, Department of Gastroenterology, US- Bangla Medical College, Narayanganj, Bangladesh.
4Assistant Professor, Department of Endocrinology, Dhaka Medical College, Dhaka, Bangladesh.
5Medical Officer, South East Model Hospital, Dhaka, Bangladesh.
6Assistant Registrar, Sheikh Russel National Gastroliver Institute & Hospital, Dhaka, Bangladesh.
7Assistant Professor, Department of Endocrinology, Rangpur Medical College, Rangpur, Bangladesh.
*Correspondence:
Mohammad Afjal Hossain, Assistant Professor, Department of Endocrinology, US- Bangla Medical College, Narayanganj, Bangladesh.
Received: 29 November 2020 Accepted: 22 December 2020
Citation: Hossain MA, Atiquzzaman, Bhuiyan MSI, et al. Subclinical Hypothyroidism in Type 2 Diabetes Mellitus Patients Attending In a Tertiary Care Hospital in Bangladesh. Diabetes Complications. 2020; 4(3); 1-5.
Abstract
Background: Type 2 diabetes mellitus (DM) and subclinical hypothyroidism (SCH) are common endocrine disorders in general population. This study was conducted to observe the frequency of SCH in type 2 DM and to compare different demographic, anthropometric and laboratory data between the type 2 diabetic patients with SCH and euthyroidism.
Materials and Methods: This cross sectional observational study was conducted among 100 (one hundred) previously diagnosed type 2 DM patients with unknown thyroid functional status which included equal number of male and female patients. Various demographic, anthropometric and clinical data were recorded and biochemical parameters like thyroid stimulating hormone (TSH), free thyroxine (FT4 ) & HbA1c were measured. SCH was diagnosed when TSH ≥5.1 µIU/ml and Free T4 remained in reference range (0.83-1.8 ng/dl). Statistical analysis was done by IBM SPSS version 22.0. A P value <0.05 was considered as statistically significant.
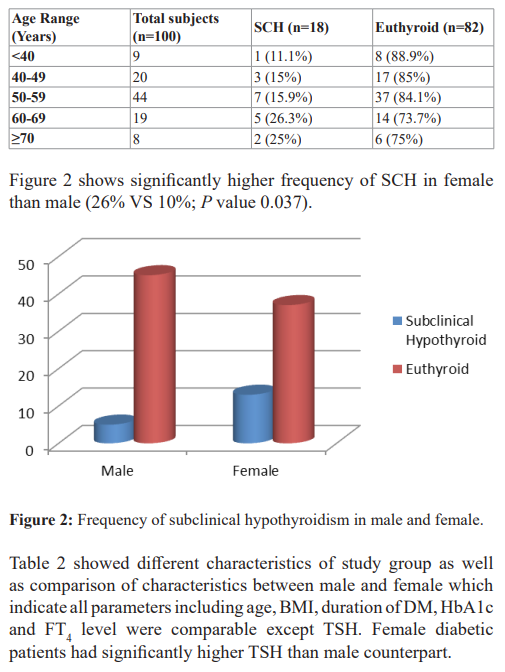
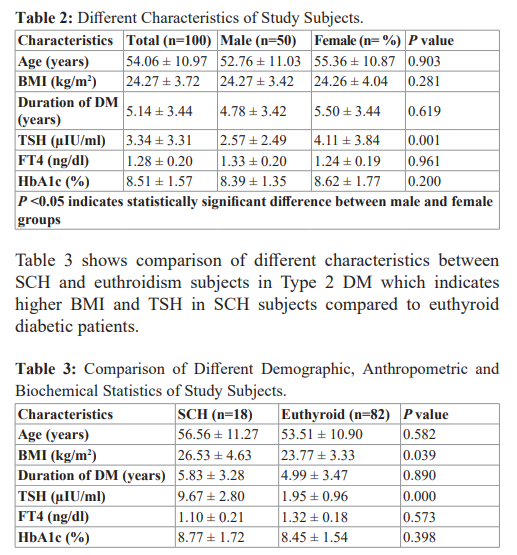
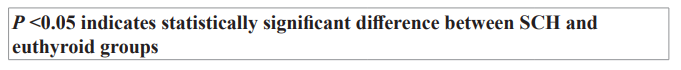
Results: Frequency of SCH in Type 2 DM was 18%. Frequency of SCH increased with age and highest frequency was found in 60-69 years age group (26.3%). Females were more affected with SCH than males (26% VS 10%, P value 0.037). Moreover females had higher mean TSH value than males (4.11 ± 3.84 µIU/ml VS 2.57 ± 2.49 µIU/ml, P value 0.001) where FT4 were comparable between them (1.24 ± 0.19 ng/dl VS 1.33 ± 0.20 ng/dl, P value 0.961). Type 2 DM patients with SCH had significantly higher BMI and TSH compared to euthyroid subjects (26.53 ± 4.63 kg/m2 VS 23.77 ± 3.33 kg/m2 , P value 0.039 and 9.67 ± 2.80 µIU/ml VS 1.95 ± 0.96 µIU/ml, P value 0.000 respectively) where age, duration of DM, FT4 and HbA1c were comparable between them (56.56 ± 11.27 years VS 53.51 ± 10.90 years, P value 0.582; 5.83 ± 3.28 years VS 4.99 ± 3.47 years, P value 0.890; 1.10 ± 0.21 ng/dl VS 1.32 ± 0.18 ng/dl, P value 0.573 and 8.77 ± 1.72% VS 8.45 ± 1.54%, P value 0.398 respectively).
Conclusions: SCH is common in type 2 diabetic patients especially in elderly, female and obese subjects.
Keywords
Introduction
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by hyperglycemia either due to impaired insulin secretion or insulin action or both [1]. It is the most common endocrine disorder which prevalence varies in different studies. Diabetes mellitus is associated with increased risk of cardiovascular diseases. The global prevalence is predicted to be 11.1% by 2033, affecting 600 million people [2]. Exact prevalence of DM in Bangladesh is not known. About 6.9 million adult Bangladeshi population had DM in 2017; it is predicted that the total number of patients will increase to 13.7 million by 2045 [3].
On other hand, thyroid disorder is another common endocrine condition in general population. Among thyroid disorders subclinical hypothyroidism (SCH) is one of the most prevalent conditions. SCH is a mild form of hypothyroidism which is usually asymptomatic and defined biochemically as a state where thyroid stimulating hormone (TSH) is mildly elevated but circulating free thyroid hormones concentration are within normal limit [4].
Type 2 DM is the most common type of diabetes worldwide where type 1 contributes minor numbers. As type 1 DM and thyroid disorders both are autoimmune conditions, there is close relationship between them. Actually thyroid disorders are the most common autoimmune disorder associated with type 1 DM [5]. American Thyroid Association (ATA) and Europium Thyroid Association (ETA) recommend screening for thyroid disorders in type I DM annually [6,7].
Although thyroid disorders are mostly associated with type 1 DM, some studies showed higher prevalence of it in type 2 DM patients than in general population [8-11]. It is well established that there is higher prevalence of overt hypothyroidism in type 2DM than in general population [12,13]. But the association between SCH and type 2 DM remains controversial. This study was conducted to see the frequency of SCH in type 2 DM patients and to compare different demographic, anthropometric and biochemical parameters between type 2 diabetic patients with SCH and euthyroidism.
Materials and Methods
This cross sectional observational study was conducted in Medicine and Endocrinology Outpatient Department of US- Bangla Medical College and Hospital over the period of 9 (nine) months dated from July 2019 to March 2020. Previously diagnosed diabetic patients as per WHO 2006 or ADA 2019 criteria [14,15] with unknown thyroid functional status were included in the sample. Diabetes diagnosed at or after the age of 25 years, not presented as diabetic ketoacidosis initially, and which was controlled initially or thereafter with oral antidiabetic drugs for at least 6 months was considered as type 2 DM. SCH was diagnosed when TSH ≥ 5.1 µIU/ml and Free T4 remained in reference range (0.83-1.8 ng/dl).
Euthyroidism was diagnosed when both TSH and FT4 were within normal limit (0.5-5.0 µIU/ml and 0.83-1.8 ng/dl respectively). Patients with previously known thyroid disorder or taking drugs affecting thyroid function, patients with chronic diseases or acute illness or pregnancy or patients who refused to take part in the study were excluded. Patients who showed abnormal thyroid function other than SCH on screening were also excluded. Total 100 (one hundred) type 2 DM patients (50 male & 50 female) as per inclusion and exclusion criteria were taken for the study. After taking informed written consent detailed clinical history was taken and physical examination was done. Various demographic, anthropometric and clinical data were recorded in a data collection sheet. TSH and FT4 were measured by ELFA (Enzyme Linked Fluorescent Assay) method in Biomerieux Mini Vidas Automated Immunoassay Analyzer, France. Current glycemic status was evaluated by measuring glycated hemoglobin (HbA1c) using enzymatic method in Selectra pro M, France.
Statistical analysis was done by IBM Statistical Packages for the Social Sciences (SPSS) version 22.0 software. Qualitative data were expressed as percentage and quantitative data were expressed as mean ± standard deviation (SD). Comparison of two groups was done by chi square test and student’s t test. A P value lees than 0.05 was considered as statistically significant.
Discussion
Type 2 DM and subclinical hypothyroidism (SCH) are two common endocrine disorders among general population. Actual prevalence of SCH in general population of Bangladesh is not known. It is estimated that about 3% to 8% of the population without known thyroid status are affected with SCH [16]. This study was conducted to observe the frequency of SCH in type 2 DM as well as to compare different demographic, anthropometric and biochemical data between SCH and euthyroid type 2 diabetic patients.
In this study, total 100 known cases of type 2 DM patients were included with equal number of male and female. Overall frequency of SCH in study subjects was 18% which is much higher than the general population. One previous study [17] found that SCH was the most common form of thyroid disorder among Bangladeshi patients with type 2 DM and frequency of SCH was 14.1% which supports our result. Some other studies conducted in Indian subcontinent also observed higher prevalence of SCH in diabetic patients. Kumar et al., Demitrost et al., Singh et al. and palma et al. found frequency of SCH in type 2 DM patients were 11.5%, 16.3%,15% and 12% respectively which also support our finding [18-21].
It is well established that prevalence of thyroid dysfunction increases with ageing [22]. In this study, it is observed that frequency of SCH in diabetic patients was increased with age and highest frequency was found in 60-69 years age group (26.3%). A study in West Bengal also found higher frequency of SCH in elderly diabetic patients and frequency was highest in same age group which supports our finding [23].
Frequency of SCH may be higher in female as thyroid dysfunction is more commonly found in them [22]. In this study, 26% female and 10% male with type 2 DM had SCH and difference was significant. Higher frequency of SCH in female diabetic patients were also found by some previous studies [17,19]. We also found significantly higher TSH in female compared to male in our study subjects. A large Chinese population based study which included 83643 individuals showed significantly higher TSH in female than male in all age groups in general population [24].
As thyroid hormones play important role in regulation of normal growth, intermediary metabolism and weight, thyroid dysfunction leads to alteration of body weight. Thyroid hormones deficiency leads to weight gain where excess leads to weight loss. As SCH is a state of slight thyroid hormones deficiency, it may leads to weight gain and increased BMI. Some studies suggest SCH is highly prevalent in people with higher BMI [25]. In this study, we also found significantly higher BMI in SCH subjects compared to euthyroid type 2 DM. Our finding is also supported by Kamrul- Hasan AB et al. which found higher BMI in type 2 DM patients with thyroid dysfunction than without thyroid dysfunction [17]. Demitrost et al. found patients with BMI> 25 kg/m2 had increased risk of having SCH in diabetic patients [19].
Relationship between glycemic statuses with SCH is still controversial. Billic-Kumarica et al. found a significant correlation of TSH level with HbA1c [26]. That study also found improvement of HbA1c after improving TSH level with proper treatment in patients with SCH [26]. In contrast to that finding, some other study did not found any correlation between them. Sharma P et al. found comparable HbA1c between subclinical hypothyroid and euthyroid diabetic individuals and concluded that high TSH is not a predictor of poor glycemic control [27]. Our study also found comparable HbA1c and duration of DM in both groups of individuals which are supported by Sharma P et al. [27].
Some studies suggest that SCH is associated with hypertension, dyslipidemia and abnormal homocysteine level and thus these patients have higher risk of metabolic syndrome, atherosclerosis and cardiovascular diseases [28-30]. As DM is also associated with similar type of metabolic abnormalities, presence of SCH further increases cardiovascular mortality and morbidity. As most of the patients of SCH in type 2 DM are obese and elderly which are established independent risk factors for development of cardiovascular disease, these patients are at highest risk of future adverse cardiovascular outcomes.
Limitations
The major limitation of our study is lack of healthy control subjects. Moreover we did not measure thyroid autoantibodies. We did not evaluate relationship between diabetes related complications and thyroid functional status.
Conclusions
High frequency of subclinical hypothyroidism was observed in Bangladeshi type 2 DM patients. SCH is more frequent in female, elderly patients and subjects with higher BMI. Routine screening of thyroid function test especially TSH should be done in all patients with type 2 DM especially in elderly, female and obese individuals.
Acknowledgements
We are thankful to the all lab stuffs of US- Bangla Medical College and Hospital for their technical support. We are grateful to all participants for their kind cooperation.
References
- Wild S, Roglic G, Green A, et Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004; 27: 1047-1053.
- Surks MI, Ortiz E, Daniels GH, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and JAMA. 2004; 291: 228-238.
- International Diabetes IDF Diabetes Atlas. 8th ed. Brussels, Belgium: International Diabetes Federation. 2017.
- Tunbridge WM, Evered DC, Hall R, et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf). 1977; 7: 481-493.
- Radetti G, Paganini C, Gentili L, et Frequency of Hashimoto & thyroiditis in children with type 1 diabetes mellitus. Acta Diabetol. 1995; 32: 121-124.
- Pearce SH, Brabant G, Duntas LH, et 2013 ETA Guideline: Management of Subclinical Hypothyroidism. Eur Thyroid J. 2013; 2: 215-228.
- Garber JR, Cobin RH, Gharib H, et Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012; 22: 1200- 1235.
- Papazafiropoulou A, Sotiropoulos A, Kokolaki A, et Prevalence of thyroid dysfunction among Greek type 2 diabetic patients attending an outpatient clinic. J Clin Med Res. 2010; 2: 75-78.
- Akbar DH, Ahmed MM, Al-Mughales Thyroid dysfunction and thyroid autoimmunity in Saudi type 2 diabetics. Acta Diabetol. 2006; 43: 14-18.
- Radaideh AR, Nusier MK, Amari FL, et Thyroid dysfunction in patients with type 2 diabetes mellitus in Jordan. Saudi Med J. 2004; 25: 1046-1050.
- Maxzud MC, Rasjido LG, Fregenal M, et al. Prevalence of thyroid dysfunction in patients with type 2 diabetes mellitus. MEDICINA (Buenos Aires). 2016; 76: 355-358.
- Distiller LA, Polakow ES, Joffe BI. Type 2 diabetes mellitus and The possible influence of metformin therapy. Diabet Med. 2014; 31: 172-175.
- Hollowell JG, Staehling NW, Flanders WD, et Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002; 87: 489-499.
- World Health Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: Report of a WHO/IDF consultation. January 14, 2006.
- American Diabetes 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019; 42: S13-S28.
- Fatourechi Subclinical Hypothyroidism: An update for Primary Care Physician. Mayo Clin Proc. 2009; 84: 65-71.
- Kamrul-Hasan AB, Akter F, Selim S, et al. Thyroid function and autoantibody status in Bangladeshi patients with type 2 diabetes Thyroid Res Pract. 2018; 15: 132-137.
- Kumar RA, Narasimhasetty KR, Lalitha R, et Prevalence of thyroid dysfunction among type 2 diabetes subjects in South India. Int J Clin Cases Invest. 2013; 5: 93-94.
- Demitrost L, Ranabir Thyroid dysfunction in type 2 diabetes mellitus: A retrospective study. Indian J Endocrinol Metab. 2012; 16: S334-335.
- Singh G, Gupta V, Sharma AK, et al. Frequency of thyroid dysfunction among diabetes in Punjabi Adv Biores. 2011: 2; 3-9.
- Palma CC, Pavesi M, Nogueira VG, et Prevalence of thyroid dysfunction in patients with diabetes mellitus. Diabetol Metab Syndr. 2013; 5: 58.
- Canaris GJ, Manowitz NR, Mayor G, et al. The Colorado thyroid disease prevalence Arch Intern Med. 2000; 160: 526-534.
- Sinha A, Mukherjee Prevalence of Subclinical Hypothyroidism Among Type 2 Diabetes Mellitus Patients At-tending the Diabetes Clinic in A Tertiary Care Medical College and Hospital of West Ben-gal. Indian Journal of Applied Research. 2019; 9: 1-5.
- Chen X, Zheng X, Ding Z, et Relationship of gender and age on thyroid hormone parameters in large Chinese population. Archives of Endocrinology and Metabolism. 2020; 64: 52-58.
- Sami A,Iftekhar MF,Rauf MA,et Subclinical Hypothyroidism among local adult obese population. Pakistan Journal of Medical Sciences. 2018; 34: 980-983.
- Billic-Kumarica E, Beciragic A, Junuzovic The Importance of HbA1c Control in Patients with Subclinical Hypothyroidism. Mater Sociomed. 2012; 24: 212-219.
- Sharma P, Sinha R, Prasad A, et al. Lack of Association between Poor Glycemic Control in T2DM and Subclinical Journal of thyroid Research. 2020; 4.
- Vanderpump MP, Tunbridge WM, French JM, et The incidence of thyroid disorders in the community: a twenty- year follow-up of the Whickham Survey. Clin Endocrinol (Oxf). 1995; 43: 55-68.
- Kabadi UM. Subclinical hypothyroidism. Natural course of the syndrome during a prolonged follow-up Arch Intern Med. 1993; 153: 957-961.
- Tunbridge WM, Brewis M, French JM, et al. Natural history of autoimmune thyroiditis. Br Med J. (Clin Res Ed). 1981; 282: 258-262.