Surgical Treatment of Basedow's Disease at the Louga Regional Amadou Sakhir Mbaye Hospital in the ENT Department
Author(s): Fall Ndiouga1, Sow Djiby1,2, Fulgence A Faye5, Fall Alioune B3, Saou Houleye1, Mbaye Pape A3, Tall Hady3, Ndiaye Ciré4
1Abass Ndao Hospital, Dakar, Senegal.
2Cheikh Anta Diop University Faculty of Medicine, Senegal.
3Louga Regional Hospital Amadou Sakhir Mbaye ENT Department, Senegal.
4Center Hospitaler National of Fann ENT Department, Senegal.
5Faculty of Medicine University of Bambey, Senegal.
*Correspondence:
Fall Ndiouga, Abass Ndao Hospital, Dakar, Senegal, Tel: 0022177 6593608.
Received: 02 Nov 2023 Accepted: 04 Jan 2024
Citation: Fall Ndiouga, Sow Djiby, Fulgence A Faye, et al. Surgical Treatment of Basedow's Disease at the Louga Regional Amadou Sakhir Mbaye Hospital in the ENT Department. Diabetes Complications. 2024; 8(1); 1-4.
Abstract
Introduction: Graves' disease (BD) is a dysimmune disorder. It is the most frequent cause of hyperthyroidism and can have a considerable impact on patients' quality of life. The aim was to study the frequency of BD and associated factors in the ENT department of Louga Hospital.
Patients and Methods: This was a cross-sectional, descriptive and analytical study conducted from June 20, 2019 to June 20, 2021. It focused on hospitalized patients with basedow disease. Epidemiological, clinical, paraclinical, therapeutic and evolutionary data were evaluated.
Results: Forty (40) cases of Graves' disease (8.52%) were collected. The mean age was 32 years, with extremes of 18 and 60 years. Females predominated (39 cases), with a sex ratio of M/F 0.26. The duration of the disease ranged from 1 month to 2 years, with an average of 19 months. All our patients presented with diffuse goiter and signs of thyrotoxicosis. Serum TSH levels decreased in 39 cases. Ultrasound scans performed in 100% of cases showed a homogeneous diffuse goiter, 87.5% of which was hypervascularized. Total thyroidectomy in all our patients (100%). The average hospital stay was (2.25) days (extremes: 2 and 4 days). Postoperative management was straightforward in all patients. No deaths were reported. Two cases of intermittent dysphonia were recorded. Histology was compatible with BASEDOW disease in 38 cases; the remaining 2 cases showed atypical nodules.
Conclusion: MB remains the main etiology of hyperthyroidism. Certain signs are almost constant, such as cardiovascular signs and goiter. Despite the effectiveness of medical treatments and radioactive iodine, surgery is playing an increasingly important role in the treatment of MB.
Keywords
Introduction
Graves' disease is a dysimmune disorder. It is the most common cause of hyperthyroidism and can have a considerable impact on patients' quality of life. It results from a conflict between TSH receptor antibodies and the thyroid gland [1]. To our knowledge, only one study has been carried out in this field in Louga in 2020, which motivated us to carry out this study, the aim of which was to describe the epidemiological, diagnostic, therapeutic and evolutionary aspects of basedow's disease at the amadou Sakhir Mbaye regional hospital in Louga.
Materials and Methods
The study was carried out in the ENT department of the Amadou Sakhir Mbaye hospital in Louga. Our study took place in the Otolaryngology and Cervicofacial Surgery Unit. Our patients were recruited over two years (June 20, 2019 to June 20, 2021). The study population consisted of patients who were consulted and operated on for Graves' disease. Included in our work were any patient presenting with MB and operated on during the recruitment period, with a complete medical record. A standard questionnaire was drawn up to serve as the basis for data collection for patients included in the study. It covered civil status, clinical manifestations, and biological, biochemical and imaging analyses of the goiter.
Data were collected from the records of patients meeting the inclusion criteria and consulted during the study period. Questionnaires were filled in from hospitalization records, reporting patients' clinical and paraclinical findings. Data were collected on:
Socioeconomic profile
Age, gender, occupation, marital status, address and level of education.
Clinical parameters:
- Clinical examination data
- Medical history
- Surgical history
- Family history
Paraclinical parameters
Blood count, liver function tests, TSHus, T3L and T4L, HbA1c, creatinine, lipid profile, renal function, electrocardiogram (ECG), TSH receptor antibodies, TPO antibodies and TG antibodies. Morphological assessment (ultrasound and thyroid scintigraphy). Data were entered into Microsoft Office Excel and analyzed using epi info 2000 version 3.3.2. Analysis was descriptive and analytical.
Ethical considerations
Data were collected anonymously and treated as confidential.
Results
Socio-demographic characteristics
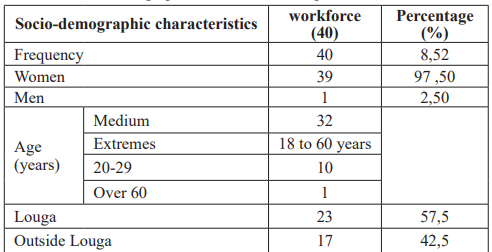
During the study period, we collected 469 patients operated for goiter, including 40 for Graves' disease (8.52%). Patients ranged in age from 18 to 60, with an average age of 32. The 30-39 age group was in the majority, at 40% (Table 1).
Table 1: Socio-demographic characteristics of patients.
Clinical data
The duration of the disease ranged from 1 month to 2 years, with an average of 19 months. A family history of goiter was found in 11 patients (27.5% of the 40 cases). One patient was known to be hypertensive and on treatment. No diabetic patients or other particular antecedents were found. A total of 38 of our patients (95%) presented with diffuse goiter. Elastic goitres were found in 38 cases, with a hard consistency noted in only one patient. Vertical mobility was found in all patients. Nodularity: 2 cases of nodular goiter (2.5% of patients) were noted in our study. A flapping cervical mass suggesting vascularity was found in 39 cases (95% of patients). Compressive nature: Goiters were compressive in 11 cases in our series, i.e. 27.5% of patients.
All patients showed signs of hyperthyroidism, including 38 with thyrotoxicosis, i.e. 95% of patients. However, there were no cases of clinical hypothyroidism. 35 cases of signs associated with goitre were found, i.e. 87.5% of patients. These 35 cases were distributed as follows Exophthalmos: 14 cases (35%). Dysphagia: 08 cases or 20% of patients, Dyspnea: 01 cases or 2.5% of patients, Dysphonia: 02 cases or 5% of patients, Tachycardia: 25 cases or 62.5 of patients.
Paraclinical data
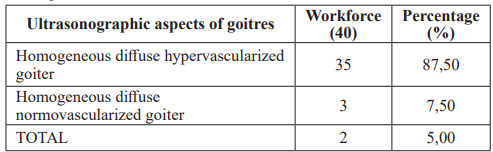
All patients in the series underwent hormone assays. Serum TSH levels were decreased in 39 cases and normal in 1. T4L was increased in the entire sample, i.e. 100%. The assay was performed on 17 cases, i.e. 42.5% in our study period, and all the results obtained came back with high levels. Thyroid ultrasonography was performed in all our patients, i.e. 100% (Table 2).
Table 2: Distribution of patients according to the ultrasound appearance of the goiter.
Therapeutic aspects
All dysthyroid patients underwent preoperative medical treatment. The aim of this treatment was to normalize thyroid hormone secretion and achieve euthyroidism. This treatment is prolonged for at least 18 months. Total thyroidectomy was performed in all our patients. No incidents were recorded for all thyroidectomies.
Evolution
An average hospital stay of 2 days, with the Redon drains removed on D2.
Post-operative complications were found in 3 cases (7.5%); one case of intermittent dysphonia after total thyroidectomy. Two cases of transient acute hypocalcemia corrected by calcium supplementation. There were no cases of hematoma. No cases of postoperative hypothyroidism were found; all our patients received hormone replacement therapy monitored by remote hormone assays. No definitive postoperative hypocalcemia complications.
Anatomopathological examination was carried out in all our patients (100%), including 38 cases compatible with balanced or treated basedow disease and 2 cases of basedow disease associated with atypical nodules; absence of signs of malignancy.
Discussion
Our study has certain limitations. Data collection was not exhaustive. Clinical and paraclinical antibody tests were not performed by our patients, due to the high cost of these examinations. All the variables studied had a satisfactory level of completeness, with variables filled in in 95% of cases. The frequency of Graves' disease was 8.52%. This frequency is not high, and can be explained by the fact that thyroid surgery is also performed for various thyroid pathologies. The primary treatment for basedow's disease is medical. In the literature, the frequency of thyroidectomy as a treatment option for Graves' disease varies from study to study. In their study, Imane et al. found a similar frequency of 7.01% [2]. Other authors found a much lower frequency [3-6].
In our study, we found a sex ratio of 0.26, with a clear female predominance. Moreover, the female sex is a risk factor for basedow's disease. Other studies have shown similar results with some variability. In our series, the mean age was 32 years. In another study in Saint Louis, the average age was 40 [13]. Studies carried out in Africa and elsewhere have found an average age of around 40 [14-16]. Stress plays an important role in the onset of the disease. Delevaux [17] states that stress can be a trigger for autoimmune thyroiditis. Less than half the patients (42.6%) reported a trigger for their disease. The mean duration of evolution was 2 years in our study, with extremes ranging from 1 month to 2 years. Imane and Sani R found a mean evolutionary time of 24 months, the majority of patients were seen after at least one year. For Sanogo, the average consultation time was 9 years [18]. These relatively long delays may be explained by the fact that surgery is not the first-line treatment for BASEDOW disease. The first-line treatment is medical, with an attack phase of 12 to 18 months [19,20].
In our study, the majority of our patients had no particular antecedents. However, the notion of familial goiter was found in 1st place and psychoaffective disorders in 3rd place. Bilosi [21] had shown in his study that psychoaffective disorders were present in 7.4%; genetic predispositions in 2.27%; Basedow's disease is known to occur in families with a predisposition to the disease. In our study, 95% presented with a diffuse homogeneous goiter with signs of thyrotoxicosis. Other studies had found similar values with diffuse homogeneous goitre with signs of thyrotoxicosis [8,13,19,22]. 35% ofpatientshadexophthalmos. Indeed, basedowian orthopathy is present in 20 to 60% of cases of BASEDOW disease [21]. In Sani R's study, exophthalmos was found in all patients [20].M. BARBUSCIA [8] found exophthalmos in 84.21% of cases; Insaf H [19] found exophthalmos in 63.3% of cases.
The thyroid hormone assay enabled us to assess the functional state of the thyroid gland. The TSH assay can be used to detect thyroid dysfunction in the general population. The very high sensitivity of this TSH level in thyroid gland function explains the choice of this parameter. The diagnosis of Graves' disease was based on the following criteria: a clinical thyrotoxicosis syndrome, with at least a decrease in TSH level or an increase in T4 or T3; these two criteria had to be associated with exophthalmos and/or a positive anti-THSH receptor antibody level [23]. Thyrotoxicosis is confirmed by TSH measurement, which, if normal, confirms hyperthyroidism. When the concentration is low, an elevated T4 and/or T3 confirms the diagnosis [24].
Graves' disease is confirmed in cases of hyperthyroidism, bilateral orbitopathy and non-painful, non-nodular goitre. In all other cases, the anti-THSH receptor antibodies specific to Graves' disease, detected in 95% of Graves' disease patients, should be measured. When the cause remains uncertain, ultrasound and scintigraphy are useful in distinguishing Graves' disease from other causes of hyperthyroidism [24].
In our series, TSHus was low in all our patients (100%; n=40), with a mean level of 0.03 µIU/m. This result is comparable to those of Moro [25] and Doho [23], who found 0.04 µIU/ml and 0.07 µIU/ ml respectively. FT4 was elevated in 90% (n=27) of our patients, with a mean level of 128.58 pmol/l. This result is similar to that of Doho [23] (120 pmol/l) but differs from that of Moro [25], who found a mean level of 49.42 pmol/l. Twenty-one (21) patients had undergone TSH receptor antibody assay, which was positive in 81% (n=17) of cases. This result is close to that of Anaddam et al. [26], who in their series found 87.5% (n=35) positive. Ultrasound is an easily accessible and inexpensive examination. In our study, all patients had undergone cervical ultrasonography; 77.5% were found to have diffuse goiter with varying degrees of hypervascularity. Similar results were found in the study by Ndour [27] and Ndiaye [22].
All our patients had received preoperative medical treatment, either 100% of cases. In our series, 100% had undergone total thyroidectomy. In several studies, this is the type of thyroidectomy most frequently used [2,27-29,11]. Over the past twenty years, the surgical treatment of thyroid disease, and in particular of basedow's disease, has evolved considerably. Despite this evolution, the risks are still present and should never be minimized. Haemorrhage is a major risk of surgery. In our series, there was no bleeding. During surgery for BASEDOW's disease, due to hypervascularization of the goiter. Its incidence is estimated at 0-2.8%. In our study, recurential paralysis was noted in 2.5% of patients. Toplica Bojic [30] reported unilateral postoperative recurrential palsy in 0.9% of patients. However, in the literature, the rate of occurrence is low (less than or equal to 3%).
In our study, we had 2 cases of acute transient hypocalcemia corrected by calcium supplementation. According to Singer's study [29], transient hypoparathyroidism after subtotal or total thyroidectomy is frequent at around 10%; persistent hypocalcemia is rare, with a low percentage [31] ranging from 1 to 7%. Any patient who has undergone total or subtotal thyroidectomy should have his or her blood calcium level checked systematically after the operation.
In our series, anatomopathology was performed on all surgical specimens, and we found 38 cases with histological aspects compatible with basedow's disease and 2 associated cases of an atypical nodule with signs of malignancy. The various studies carried out: Mssouri R et al. [3], in a study carried out in Morocco, found 1.1% thyroid cancers in 547 cases of Graves' disease, and considers the appearance of nodules during Graves' disease to be a strong indication of goiter degeneration. The incidence of thyroid cancer varies between 0% and 21% according to the authors [20].
The incidence of thyroid cancer in patients with Graves' disease varies from 0.15% to 15%, depending on the study. In other studies, Limonard et al. [32] show a cancer rate of 3.13%. A study carried out in Japan in 1985 found that 5.1% of patients had Graves' disease associated with papillary carcinoma. The variability of these results can be explained by the varying quality of anatomopathology examinations.
References
- Allix, Wémeau JL, Carnaille B, et Treatment of hyperthyroidism Endocrinologie. Encycl Méd Chir Elsevier Paris. 2007.
- Imane Rida, Jerome Hershman Hyperthyroidism. Clin Immunol Immunopathol. 2020; 84: 212.
- Missouri R, Thiriona M, Percherona S, et al. Thyrotoxicose Réanimation. 2006; 15: 497-505.
- Diagnosis and management of thyrotoxicosis. BMJ.2006; 332: 1369-1373.
- Sissoko, Goichot Clinical Endocrinology. 2016; 84: 445-451.
- Diallo, Nouedoui C, Moukouri E, et al. Hyperthyroidism in Yaoundé Cameroon some epidemiological etiological and therapeutic aspects review of our Médecine d Afrique Noire. 1999; 46: 192-198.
- Nqjeh Coli DH, Kake A, Sylla D, et al. Autoimmune attacks during thyroid pathology in RAFMI. 2019; 6: 14-19.
- Barbuchia M, Koffi Dago, Fagnidi, et Kouamé Les Hyperthyroïdies à Abidjan Aspects Cliniques Biologiques Thérapeutiques et Évolutifs à Propos de 399. Cas Health Sci. 2019; 20.
- Leyes A, Ndiaye N, Léye YM, et al. I Sène Thyroidectomies at the Centre Hospitalier National de Pikine Dakar indications and results in 417 RAFMI. 2016; 1: 36-110.
- Lallement JC, Astruc F, Tassin X, et Le traitement chirurgical de la maladie de basedow à propos de 112 cas. Cahier d ORL P d Artigues Bonnip. 1998; 33: 145-150.
- Amélie Ryndak Swiercz. Ontogenèse anatomie histologie et physiologie de la thyroïde. Elsevier Masson 2010; 3-10.
- Defechereux T, Meurisse M. Hemostasis and ultracision in thyroid Ann Chir. 2006; 131: 154-156.
- Dia A, Leenhardt L, Aurengo A, et al. Thyroid ultrasonography La thyroïde. Paris 2001; 293-301.
- Dieng F, Cissé F, Gdour FD, et al. Indications and results of thyroµdectomies performed in a general surgery department About 402 patients operated Chir Lpéc. 2010; 4: 24.
- Darre M, megbor D, mana, et al. Epidemiological profile of tumors of the thyroµde Fédecine d frique noire. 2014;1: 242-251.
- Dieng F, Gdour O, Da O, et Surgical treatment of hyperthyroµdies of asedop disease and nodular goiter basedopi Ûé. Revue frique de chirurgie. 2000; 2: 31-41.
- Zeriouh B, Avisse C, Flament J, et La thyroïde 2° éd. Paris Elsevier. 2001; 7-11.
- Insaf AH, Karima K, Lotfi C, et Treatment of Graves disease. Presse Med. 2004; 33: 17-21.
- Bilosi M, Bimguet, Goudet P, et al. Subtotal thyroidectomy remains as indicated in basedow disease. Ann Chir. 2002; 5: 10-20.
- Brunauda L, Ayava S, Chatelinb J, et al. Is thyroid scintigraphy still useful in the management of a thyroid nodule The surgeons point of Annales de chirurgie. 2006; 131: 514-517.
- Ndiaye M, Ndiaye N, Kouama Nandjou P, et al. Chirurgie de l hyperthyroïdie medical. 2006; 51.
- Doho, ZARA Lathyroide Connaissances acquisitions perspectives. Expansion scientifique Française. 1974; II: 456- 460.
- Chapuis Anatomy of the thyroid body. Encyclopédie Médecine Chirurgie Paris. 1997; 1000: 10-16.
- Moro C, Chevallier JM, Martelli H, et al. The surgical discovery of the parathyroid gland and the notion of known Ann Chir. 1995; 49: 296-304.
- Anaddam S, Ba rakate K, Ouleghzal H, et al. Graves disease about 40 In Thyroïde. 2011; 2: 375- 401.
- Ndour O, Leclere J. La thyroïde des concepts à la pratique Elsevier. 200; 617.
- Ndiaye M, Ndiaye N, Kouama Nandjou P, et al. Surgery for hyperthyroidism Medical. 2006; 51.
- medical management of non para thyroid hypercalcemia and hypocalcemia otolaryngologic. clin North Am. 1999; 29: 707-710.
- Robbins KT. Neck dissection classification update revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology Head and Neck Surgery. Arch Otolaryngol Head Neck 2002; 128: 751-758.
- Menconi F, Marcocci C, Marinò M, et al. Diagnosis and classification of Graves disease. Auto immun Rev. 2014; 13: 398-402.
- Limonard E, Bisshops Fillers E Thyroid function after subtotal thyroidectomy in patients with the graves. Disease J surg Res. 2011; 168: 1-4.