The Dangerous Staircase of Stress
Author'(s):Alfvén G1 and Andersson E2,3
1Clintec, Karolinska Institutet, Sweden
2The Swedish School of Sport and Health Sciences, Sweden
3Department of Neuroscience, Karolinska Institutet, Stockholm,Sweden
*Correspondence:
G Alfven, Clintec, Karolinska Institute, SE 11620 Stockholm,Sweden, Tel: +46 739660835.
Received: 30 March 2021; Accepted: 11 July 2021
Citation: Alfvén G, Andersson E. The Dangerous Staircase of Stress. Anesth Pain Res. 2021; 5(2): 1-6.
Abstract
Chronic negative stress may be the start of a progress of illness, that may end in serious troubles for the affected. In this Perspective we highlight the steps in such a progress, what we call a staircase of stress. This underlines the importance of recognition, understanding and therapeutic measures at an early stage of the stress disorders.
Keywords
Negative stress can lead to a defense reaction, a withdrawal reaction from threat of physical or psychological nature. Chronic pain disorders are pandemic [1] and negative chronic stress is a major cause [2-5]. In this article, based on clinical experience and research from children 6-18 y, we highlight that chronic negative stress can cause a negative pain development, starting with one pain, in a next step two and sometimes several pains. An increased risk for developing central sensitization of the pain system increases pain spread with an increased risk of ending with fibromyalgia. Fibromyalgia is a serious pain disorder [6,7], with a history starting often after maltreatment in childhood [8]. It is more common in females, and has an increased risk of depression [9] and suicide [10].
We call this progress of chronic negative stress into increasing ill health the staircase of stress, see Figure 1. In this article we will clarify this perspective by presenting the different steps.
Step one
Psychosomatic pain can start with one pain, and after some time and/or with increasing severity of the stress, a second pain or more may be added to the illness. In a study population consisted of a representative national sample of 2597 children aged 10-18 years with headache, stomachache and perceived stress was measured. Many children had either headache or stomachache (Figure 2) [4].
Step two
This study also showed that with increasing frequency of perceived stress, the occurrence of pains increased and so did the likelihood of co-occurrence of these pain [4] (Figure 2).
In an exploratory descriptive study compromising 47 children aged 6-17 years with psychosomatic recurrent pain, the number of pains increased with longer duration of the illness [11], see also below. Thus, these two studies confirm the notion that longer and more severe negative stress increases the likelihood of occurrence of pains.
Step three and four
A pathophysiological understanding of the pain process is a prerequisite for a clear understanding of a disorder. Two principles explain the spread of pain in psychosomatic illness.
First, negative stress often results in a general reaction affecting the muscular system, which has been demonstrated in a case- control study comprising 19 teenagers with psychosomatic pain and a matched control group of 21 children. An increase of muscle tension in rest was recognized [12] (Figure 3). The study also demonstrated (when given unexpected startle sound provocations in ear phones) more frequent, higher, longer and earlier muscle activity bursts [12] (Figure 4), in several areas of the body where the pattern of tender points, so called stress tender points are found in the psychosomatic pain patients [13] (Figure 5). These areas are also related to the recurrent pain i.e. headache, shoulder and back pains, breast pains and stomach pains. Thus, in these children with
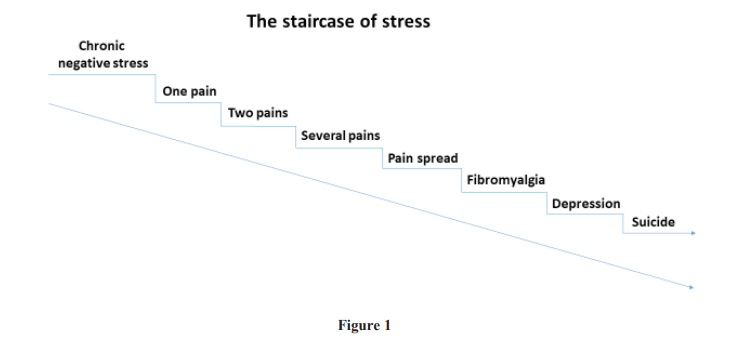
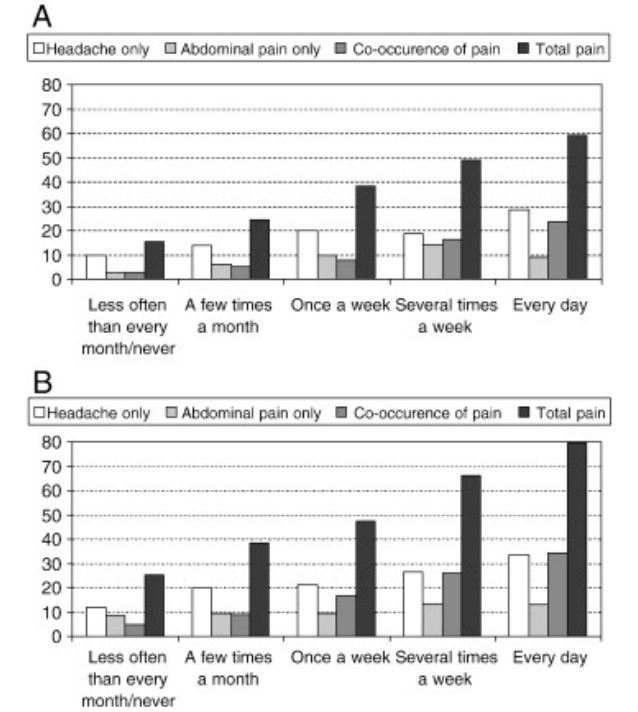
Figure 2: (A) Proportion of boys (%) experiencing recurrent pain (at least every week) by frequency of perceived stress. Sweden 2002-2003, n=1303 (Alfvén et al. 2008). (B) Proportion of girls (%) experiencing recurrent pain (at least every week) by frequency of perceived stress. Sweden 2002- 2003, n=1294.
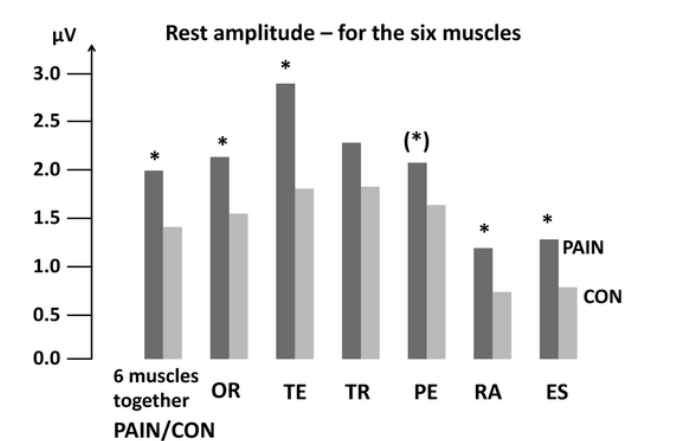
Figure 3: Mean EMG amplitude (μV) during rest. Values are shown for all six muscles together and separate muscles: OR-orbicularis occuli, TE- temporalis, TR-trapezius, PE-pectoralis, RA-rectus abdominis and ES-erector spinae. PAIN versus CON showed significantly higher values (dark vs. light grey bars) for all muscles together and for majority of each muscle. (Strong trend for PE *p = 0.052).
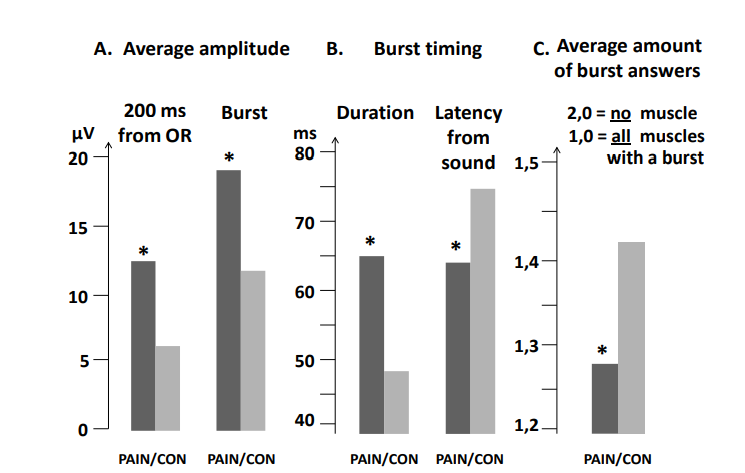
Figure 4: Average for all eight startle sound events together (no other stress provocation), including all six muscles, for: (A) Mean amplitude (μV) during 200 ms from OR-activity-start and during burst, (B) Burst duration and -latency (ms) from sound to muscle-activity-start (≥10 μV), (C) Average amount of bursts:- mean of 1.0 = all muscles burst (peak ≥ 10 μV) and 2.0 = no muscle had burst (peak ≥ 10 μV) in any of the eight stimuli. PAIN versus CON showed significant differences (star). (OR, orbicularis oculi).
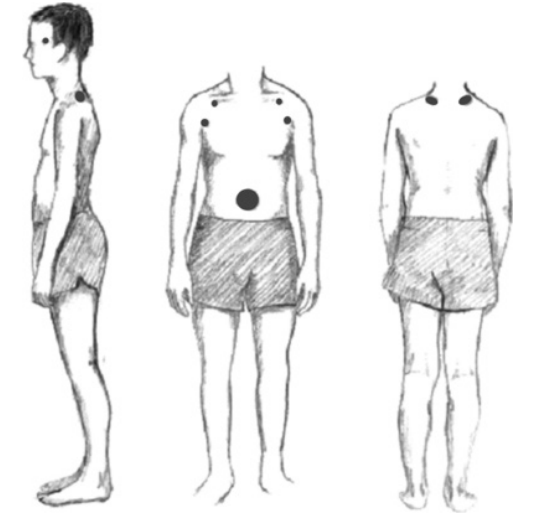
Figure 5: Stress tender points and typical startle reaction position. From a photo of an adolescent with long-standing recurrent psychosomatic pain. Stress tender point pattern is shown as grey dots.
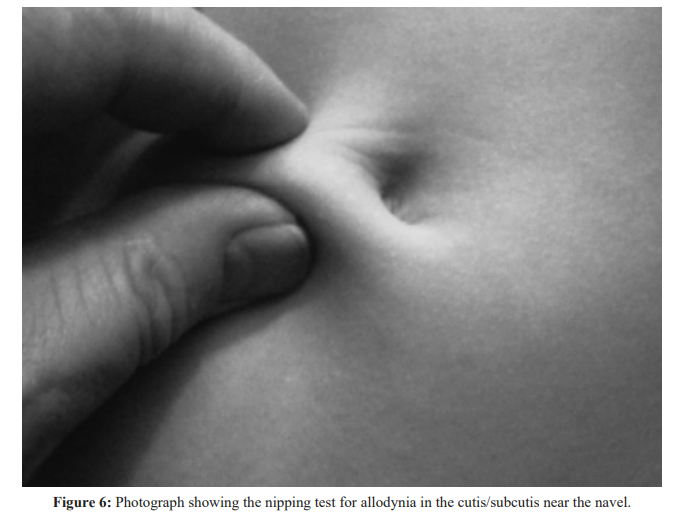
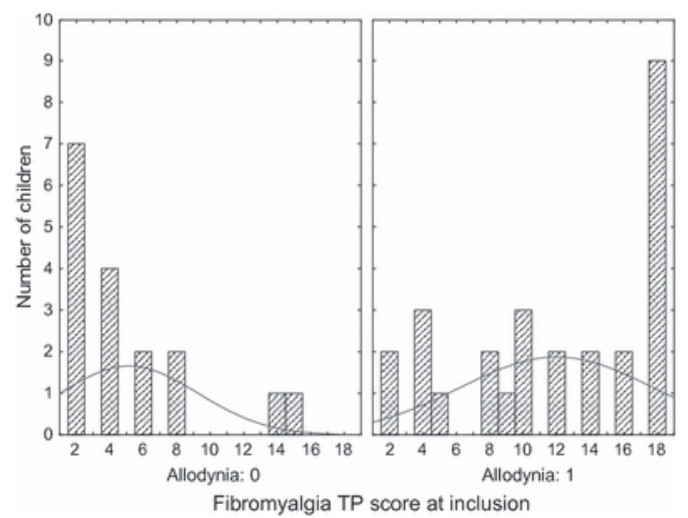
Figure 7: Histogram of the fibromyalgia TP score at inclusion for children without (histogram on left) and children with (histogram on right) allodynia.The curved lines indicate the mean values for the scores.
recurrent psychosomatic pain the found increased muscle activity excitability indicate a disturbance in the muscle motor control of the central nervous systems [5,12].
Second, It is known that pain can primarily result from central sensitization leading to pain spread. Gunnarsson et al. found an increased deep pain sensitivity in patients with persistent musculoskeletal pain, but not in regularly recurrent pain patients or in acute pain [14]. In a headache study, signs of sensitization were secondary to the primary pain [15].
In the study mentioned above compromising 47 children [11] we demonstrated allodynia, a sign of central sensitization, with the Nipping test, (Figure 6 and Appendix 1). It was accompanied with a higher frequency of tender points for fibromyalgia (Figure 7). With longer duration of the illness and more pains, allodynia was more frequent, factors that increases the risk for sensitization, pain spread and fibromyalgia.
To be more specific, we present some more data from this study. The mean duration of abdominal pain was 28.9 (3-108) months. The duration of pain and the fibromyalgia TP score were correlated significantly (r=0.35, p<0.05). For the children with a fibromyalgia with TP score >10 (n=16), the mean duration of abdominal pain was 40.2 (3-108) months, whereas for the children with a fibromyalgia TP score <11, the mean duration was 22.9 (3-60) months. This difference was significant (p<0.01). The age of the children in these two groups did not differ (p=0.47). The number of locations of pain varied, with a mean of 2.5 (range 1-5). Five children reported only abdominal pain, 25 had two locations of pain (abdominal pain and most often headache), seven children had three, six children had four and two children had five different locations of pain. The number of pain locations was correlated significantly with the duration of pain (r=0.35, p<0.05). The total number of pain locations was also correlated with the fibromyalgia TP score (n=46; r=0.37, p<0.01).
Step five
Fibromyalgia is a medical problem already in the teenage [6], but according to our knowledge seldom searched for in clinical practice. The etiology is multiple, but negative stress is one important factor.
Step six
Fibromyalgia increases the occurrence of depression [9], and vice versa, depression increases the occurrence of fibromyalgia.
Step seven
It is well known that depression is a major cause of suicide [10].
Limitations and strengths
Several conclusions made in this article is based on limited data from own studies. The psychosomatic pain diagnosis has for long been unclear as based on weak diagnostic approach. A diagnosis based on firm diagnostic criteria, see Appendix 2 [17], as the studies referred to here, has opened up for scientific studies and a deeper understanding of the psychosomatic disorder. An important finding emphasized in this report is the increased excitability in several muscles shown with an increased startle reflex and higher resting electromyographic activity among youth with recurrent psychosomatic pain due to stress. However, more studies are need to confirm several of the findings discussed in this article.
References
1.King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain. 2011; 152: 2729-2738.
2.Teodorescu D-S, Heir T, Siqveland J, et al. Chronic pain in multi-traumatized outpatients with a refugee background resettled in Norway: a cross-sectional study. BMC Psychology. 2015; 3: 7.
3.Östberg V, Låftman SB, Modin B, et al. Bullying as a Stressor in Mid-Adolescent Girls and Boys–Associations with Perceived Stress, Recurrent Pain, and Salivary Cortisol. Int J Environ Res Public Health. 2018; 15: 364.
4.Alfven G, Östberg V, Hjern A. Stressor, perceived stress and recurrent pain in Swedish schoolchildren. Journal of Psychosomatic Research. 2008; 65: 381-387.
5.Alfvén G, Grillner S, Andersson E. Children with chronic stress-induced recurrent muscle pain have enhanced startle reaction. Eur J Pain. 2017; 21: 1561-1570.
6.Mikkelsson M. Musculoskeletal pain and fibromyalgia in preadolescents. Prospective 1-year. Turun Yliopoista. Turko. 1998.
7.Matera E, Palumbi R, Peschechera A, et al. Juvenile Fibromyalgia and Headache Comorbidity in Children and Adolescents: A Literature Review. Pain Res Manag. 2019; 1-4.
8.Häuser W, Hoffman E-M, Wolfe F, et al. Self-reported childhood maltreatment, lifelong traumatic events and mental disorders in fibromyalgia syndrome: a comparison of US and German outpatients. Multicenter Study. Clin Exp Rheumatol. 2015; 33: 86-92.
9.Gracely RH, Ceko M, Bushnell MC. Fibromyalgia and Depression. Review Article. Hindawi Publishing Corporation. Pain Research Treatment. 2012; 9: 486-590.
10.Dreyer L, Kendall S, Danneskiold-Samso B, et al. Mortality in a cohort of Danish patients with fibromyalgia: Increased frequency of suicide. Arthritis Rheumatism. 2010; 62: 3101-3108.
11.Alfven G. Recurrent pain, stress, tender points and fibromyalgia in childhood: an exploratory descriptive clinical study. Acta Paediatr. 2012; 101: 283-291.
12.Alfven G, Grillner S, Andersson E. Review of childhood pain highlights the role of negative stress. Acta Paediatr. 2019; 108: 2148-2151.
13.Alfven G. Psychosomatic pain in children: A psychomuscular tension reaction? Eur J Pain. 1997; 1: 5-14.
14.Gunnarsson HE, Grahn B, Agerström J. Increased deep pain sensitivity in persistent musculoskeletal pain but not in other musculoskeletal pain states. Scandinavian Journal of Pain. 2016; 13: 1-5.
15.Clifford J Woolf. Central sensitization: Implications for the diagnosis and treatment of pain. Pain. 2011; 152: 2-15.
16.Buchgreitz L, Lyngberg AC, Bendtsen L, et al. Frequency of headache is related to sensitization: a population study. Pain. 2006; 123: 19-27.
17.Alfven G. One hundred cases of recurrent abdominal pain in children: Diagnostic procedures and criteria for a psychosomatic diagnosis. Acta Paediatr. 2003; 92: 43-49.
18.Alfvén G. The pressure pain threshold (PPT) of certain muscles in children suffering from recurrent abdominal pain of non-organic origin. An algometric study. Acta Paediatr. 1993; 82: 481-483.